Abstract
Aim This study aimed to evaluate the potential discolouration and carious lesion arresting effect of silver diamine fluoride (SDF) and silver diamine fluoride/potassium iodide (SDF/KI) in the treatment of carious primary teeth.
Materials and method A total of 30 carious primary canines were randomly assigned to treatment groups where Group I was treated with SDF while Group II was treated with SDF/KI. Caries arrest was assessed based on consistency and stability of lesion size while the discolouration of treated lesions was assessed digitally using a VITA Easyshade spectrophotometer.
Results Both treatments demonstrated 100% efficacy in arresting active caries lesions. Regarding discolouration, the total colour difference represented by delta E (ΔE) was 16.45 ± 5.69 for Group I compared to 9.54 ± 3.09 for Group II immediately post-operative, with a statistically significant difference (p = 0.003). Both groups showed similar values at 1, 3, 6 and 12 months after the treatment, with no statistically significant difference. No incidence of serious adverse effects related to either treatment and the majority of parents/guardians were satisfied with both treatments compromising their child's aesthetic appearance.
Conclusions Both SDF and SDF/KI are effective in arresting carious lesions in primary teeth but in terms of the discolouration potential, the use of KI significantly reduced the discolouration caused by SDF immediately post-operatively. Unfortunately, marked discolouration was recorded in the subsequent follow-up visits, compromising the aesthetic outcome.
Key points
-
Based on the results of our study, both silver diamine fluoride and silver diamine fluoride/potassium iodide were effective in arresting carious lesions in primary anterior teeth, but the application of potassium iodide didn't prevent the discolouration caused by silver diamine fluoride application.
-
No adverse events were reported with either materials.
-
Although parents/guardians perceived discolouration, they were open to compromise aesthetics in favour of using a less invasive approach.
Similar content being viewed by others
Introduction
Dental caries has been recognised as a major public health problem and one of the most frequent chronic diseases impacting humans worldwide, affecting 60-90% of schoolchildren.1 In children from families from a low-income background, the majority of carious lesions were left untreated due to cost and limited availability or access to dental services. For these reasons, the severity of the disease increases, which leads to pain, expense and a decreased quality of life for the affected children and their families.2
In this context, there was a great interest in simple, effective, accessible, affordable and safe treatments to halt the progress of carious lesions. Among these treatments is silver diamine fluoride (SDF), which can be used as the best strategy to control the burden of dental caries in children around the world.3
The Food and Drug Administration authorised the use of SDF as a dentine hypersensitivity agent in 2014 and acknowledged its off-label use for caries arrest and prevention in the United States, the United Kingdom and Thailand.1 Moreover, the American Dental Association and American Association of Paediatric Dentistry support its off-label usage in a comprehensive caries management programme to arrest cavitated caries lesions in primary teeth.4
Clinically, there are a multitude of benefits associated with the application of SDF in the clinical management of caries. One such benefit is the simple and relatively painless application that allow it to be widely used in special conditions, such as early childhood caries, paediatric patients with additional needs and patients with behavioural or medical issues impeding conventional therapy. Another major advantage is its cost-effectiveness, where small volumes (25 μL) of SDF can be used to treat up to five teeth. Thus, dentists can offer dental treatment to those who cannot afford or access regular dental care.5
The black discolouration of carious enamel and dentin that resulted from the application of SDF may limit its use. Because the discolouration affects the aesthetic appearance of the tooth, many parents/guardians may oppose treatment, making the dentist hesitant of proposing it as a treatment option.6
In an attempt to minimise the black discolouration, the use of a potassium iodide (KI) solution after SDF application has been suggested. Unfortunately, there is insufficient evidence to demonstrate its effectiveness in reducing tooth discolouration, so clinical studies with a long period of observation are still needed.5,7 Our study aimed to evaluate the potential discolouration and carious lesion arresting effect after application of SDF versus SDF/KI in the treatment of carious primary anterior teeth.
Materials and methods
Study design
This was a split-mouth, randomised, controlled, clinical study conducted to evaluate the potential discolouration and carious lesion arresting effect after application of SDF versus SDF/KI in the treatment of carious primary anterior teeth. The Consolidated Standards of Reporting Trials (CONSORT) guidelines were followed to ensure the reporting of this clinical study.8
Sample size
The power and sample size calculations programme (Sealed Envelope Ltd, 2012) was used to calculate the sample size.9 The continuous outcome superiority trial power calculator is available online at https://www.sealedenvelope.com/power/continuous-superiority/. Based on the results of Nguyen et al.,10 a total sample size of 30 patients was calculated, with an 80% chance of detecting an increase in the mean lightness values from 53.6 in the control group to 71.3 in the experimental group, at a 5% level of significance and a 35% dropout rate.
Ethical aspects
The current research was carried out in compliance with the Helsinki Declaration.11 Ethical approval was obtained from the Ethics Committee of Scientific Research, Faculty of Dentistry, Cairo University. After a comprehensive explanation of the treatment procedure, benefits and possible complications, informed consent was obtained by the children's parent/guardian.
This study has been registered on clinicaltrials.gov under the title 'Staining potential and caries arresting effect of silver diamine fluoride⁄potassium iodide and silver diamine fluoride' with the identifier NCT04196829.
Study setting
Children were recruited from the outpatient clinic of the paediatric dentistry and dental public health department and they were carefully assessed for eligibility to participate in the study.
Inclusion criteria
-
Children aged from 3-6 years old
-
Children with bilateral carious primary canines
-
Active carious lesions which have International Caries Detection and Assessment System (ICDAS)12 code 4 or 5.
Exclusion criteria
-
Children with spontaneous pain or any signs of pulpal infection
-
Children having any clinical or radiographic signs of periapical infection
-
Active carious lesions which have ICDAS codes other than 4 or 5
-
Children which have sensitivity to silver or other heavy metal ions
-
Children which have any gingival or perioral ulceration or stomatitis.
Randomisation and allocation concealment
Owing to the split-mouth study design, randomisation was performed to assign right side carious canines to one of the treatment modalities using a sealed envelope, while the left side carious canines were assigned to the opposite group automatically, with a 1:1 allocation ratio dividing the 30 carious primary canines into two equal groups with 15 teeth in each group as follows:
-
Group I (n = 15): teeth treated with SDF (e-SDF, Kids e-Dental, India. One bottle [3.25 mL] containing 38% SDF)
-
Group II (n = 15): teeth treated with SDF/KI (Riva Star, SDI, Bayswater, Australia. Two bottles - a silver bottle [1.5 mL] containing 38% silver fluoride in an ammonia solution and a green bottle [3.0 mL] containing KI solution).
Blinding
The child participants and their legal guardians, the outcomes assessors and the statistician were blinded.
Baseline clinical examination
Participants' personal, medical and dental histories were obtained at the baseline examination. Through meticulous visual inspection of the carious lesion, the state of carious lesions was recorded and scored according to the ICDAS using a ball-ended World Health Organisation probe with gentle force.
The colour of the carious lesion was assessed digitally using a VITA Easyshade spectrophotometer after being calibrated in accordance with the manufacturer's instructions to assess the baseline shade of the carious lesion before treatment. A single operator replicated the L*, a* and b* values three times and the average values were recorded. The L* axis represented lightness ranging from black (0) to white (100), the a* axis ranging from red (+a*) to green (-a*), and the b* axis ranging from yellow (+b*) to blue (-b*).
Clinical procedure
In Group I, the gingival tissue in the anterior area was protected with petroleum jelly and the affected tooth surface was gently cleaned and dried with cotton gauze. Using a micro brush, the affected tooth surface was coated with a 38% SDF solution. Moisture control was maintained for at least one minute after SDF placement using a gentle flow of compressed air to allow for absorption, then excess SDF was removed using cotton gauze.
In Group II, the application of SDF was carried out in the same manner as in Group I, followed by the immediate application of the KI solution using a separate micro brush, saturated with KI solution, until the precipitate went from yellow to white and then clear.
The colour of the treated carious lesion was recorded immediately post-operatively using a digital VITA Easyshade spectrophotometer to calculate the delta E (ΔE) value that defines the total colour difference. Then, children were instructed to avoid rinsing, eating and drinking for one hour after treatment. All children were recalled back after 1, 3, 6, 9 and 12 months to assess treatment outcomes.
Outcomes
-
Discolouration of the carious lesion was assessed digitally using ΔE as follows: ΔE = ([ΔL]2 + [Δa]2 + [Δb]2)
-
Carious lesion arrest was judged based on:
-
The stability in the size of the carious lesion, evaluated using the ICDAS index, into stable or progressing
-
The consistency of the lesion was evaluated upon gentle probing using a ball-ended World Health Organisation probe into soft or hard
-
-
Evaluation of the presence or absence of adverse events observed or complaints from either parents/guardians or the children, including pain, transient gingival swelling and gingival bleaching
-
Parent/guardian satisfaction for SDF treatment was recorded using a detailed questionnaire.13
Statistical analysis
Quantitative data were represented as mean and standard deviation (mean ± SD) values and the t-test was used to assess the significant differences. Qualitative data were described as frequencies and percentages and the chi-square test was used to assess the significant differences. The p-value was considered statistically significant if ≤0.05. The IBM SPSS Statistics (22.0) software package for Microsoft Windows was used to conduct the statistical analysis.
Results
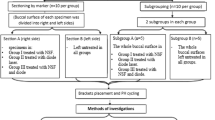
The flow of patients throughout the study, as demonstrated in Figure 1, showed that 13 patients with 26 carious lesions completed the 12-month study period, while only two subjects with four carious lesions failed to complete the entire follow-up period. Due to the COVID-19 lockdown, patients couldn't attend the clinic for follow-up at nine months.
Patients who participated in the present study were aged between 4-6 years, with a mean age of 5.33 ± 0.64 years, while the distribution of sexes was 60% boys and 40% girls. At the baseline examination by ICDAS classification, 60% scored 4 and 40% scored 5.
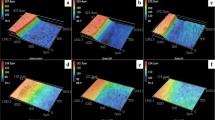
Regarding the discolouration of treated carious lesions, the colour parameter that changed the most in both groups was ΔL, which represented a greater darkening of the teeth. With a p-value of 0.006, there was a statistically significant difference between the two groups immediately after the treatment, while no statistically significant differences were found at 1, 3, 6 and 12 months, as shown in Table 1.
Regarding the ΔE values among both groups, Group I recorded higher values immediately after treatment in comparison to Group II, with a statistically significant difference (p = 0.003). Both groups showed similar values at 1, 3, 6 and 12 months after the treatment with no statistically significant difference, as shown in Table 2.
When comparing ΔE at different time intervals, both groups showed a progressive increase in ΔE throughout the entire follow-up period, with only a statistically significant difference between the immediate post-operative and one month (p = 5.6E-08 for Group I and p = 1.1E-07 for Group II).
Assessment of the effect of both treatments in arresting carious lesions has relied on the tactile evaluation of lesion consistency and the employment of the ICDAS codes to evaluate the stability of the lesion size. In both groups, all the treated teeth were considered arrested at the 6- and 12-month follow-up periods, as shown in Figure 2.
Concerning adverse events observed or complained about from either parents/guardians or children, only one case (7.7%) in Group I complained of pain and transient gingival swelling, while gingival bleaching was observed in 23.1% and 15.4% in Group I and II, respectively, with no statistically significant difference (p = 0.30782).
Regarding parental satisfaction with treatment, most parents/guardians agreed or strongly agreed about the ease of application, the painlessness of the process and the taste of both materials, while 84.6% in Group I and 69.2% in Group II weren't comfortable with the discoloration of teeth, as shown in Figure 3.
Discussion
SDF was proposed as an alternative treatment for caries prevention and arrest because it is simple, relatively painless and affordable, as well as conforming to the concept of minimally invasive dentistry. As a result, treating caries lesions with SDF appears to be particularly appropriate for younger, less compliant and socially vulnerable children.14
The discolouration that follows SDF application has significantly diminished its use in paediatric and adult patients. One of the proposed methods for preventing this adverse side effect is the application of KI immediately after SDF.15
Unfortunately, there is conflicting evidence regarding the effect of SDF/KI on tooth colour. In vitro studies on both primary and permanent teeth showed that KI was effective in preventing tooth discolouration, while a clinical study on root caries in the older population found no effect.15 Moreover, only a single clinical trial with six months of follow-up revealed a 25% reduction in the incidence of discolouration following KI application, owing to the scarcity of studies that evaluate the effect of SDF with KI and its methodological limitations.16,17 The present study aimed to evaluate the potential discolouration and carious lesion arresting effect after application of SDF versus SDF/KI in the treatment of carious primary anterior teeth.
The current study demonstrated 100% efficacy of both treatments in arresting all active caries lesions where all lesions were hard and stable in size. These findings were in accordance with previous studies and can be attributed to the high silver and fluoride ion concentrations, the synergic effect of these ions and its increased alkalinity.1,13,18,19
The silver component interacts with the sulphhydryl groups of proteins and DNA from the microorganisms, interfering in the bacterial metabolism and causing its destruction and inhibiting the formation of biofilm. Additionally, the silver salts formed on the dentin surface block the dentinal tubules, reducing tooth sensitivity and contributing to forming a very resistant dentin outer layer.1,20,21
The fluoride component of the SDF reacts with calcium phosphate and hydroxyapatite to form fluorapatite and calcium fluoride, which improves the acid resistance, mineral density and hardness of the carious dentin, which is consistent with dentin remineralisation.22
Additionally, SDF inhibits the breakdown of the exposed collagen matrix, owing to the high concentration of silver which inhibits matrix metalloproteinases and cysteine cathepsins. This is very important, as the collagen network provides the scaffold for the new remineralisation cores.22,23
The evaluation of discolouration was done using a digital VITA Easyshade spectrophotometer. VITA Easyshade measures the complex colour of tooth structure numerically, where the L*, a* and b* colour system was used to elucidate each colour three-dimensionally in space. This device has shown high reliability and reproducibility, eliminating the problems of subjectivity in colour assessment by giving quantitative values to calculate the ΔE value that defines the total colour difference between the final and baseline values.7,24,25
Immediately after the application of both materials, both groups showed a degree of discolouration represented by a mean ΔE value equal to 16.45 ± 5.69 for Group I and 9.54 ± 3.09 for Group II, which was in agreement with previous studies.7,26,27
This finding can be attributed to black precipitate formed on the surface of carious dentine because of the reaction of unreacted silver ions on the partially denatured collagen, where the excess unreacted silver ions precipitated as silver sulphide, inducing discolouration.27,28
In both groups, the degree of discolouration increased markedly at one-month follow-up, represented by the progressive increase in mean ΔE value by 35.84 ± 3.94 in Group I and 33.75 ± 8.50 in Group II, with a statistically significant difference between the immediate post-operative and one-month follow-up (p = 5.6E-08 in Group I and a p = 1.1E-07 in Group II). The difference in mean ΔE value between 1, 3, 6 and 12 months wasn't statistically significant in both groups.
This finding can be linked to the fact that metallic silver was formed by the reaction of SDF and hydroxyapatite and its production was accelerated when exposed to light and high temperatures that eventually increase the brown-black appearance of the carious lesion over time.24,27,28,29
When discolouration was compared in both groups immediately post-operatively, Group I showed more discolouration, represented by a higher mean ΔL value (-13.76 ± 5.72), compared to Group II (-6.84 ± 3.98), with a statistically significant difference (p = 0.006) and a higher mean ΔE value (16.45 ± 5.69) compared to Group II (9.54 ± 3.09), with a statistically significant difference (p = 0.003), which was in agreement with previous studies.26,27,28,29
The ability of KI in reducing the discolouration caused by SDF can be justified through reaction with the free silver ions, producing a creamy white precipitate of silver iodide.27,28
On the contrary, both groups showed a similar degree of discolouration represented by mean ΔE values equal to 35.84 ± 3.94, 37.85 ± 9.08, 40.29 ± 10.11 and 45.24 ± 6.94 at 1, 3, 6 and 12 months, respectively, for Group I, and mean ΔE values equal to 33.75 ± 8.50, 36.42 ± 7.87, 39.72 ± 6.63 and 44.65 ± 5.80 at 1, 3, 6 and 12 months, respectively, for Group II. There was no statistically significant difference between groups at 1, 3, 6 and 12 months, with a p-value of 0.489, 0.717, 0.896 and 0.857, respectively.
These findings were in accordance with several studies2,16,17,26,30 that reported the ability of KI to improve initial aesthetic appearance after SDF application. However, after time, KI does not seem to result in any significant difference in discolouration. This can be attributed to the fact that silver iodide, which is formed upon the application of KI following SDF, is a photosensitive material that can dissociate into silver and iodine when exposed to light.15,29
No incidence of serious adverse effects related to both treatments occurred during the whole study period. Oral pain, transient gum swelling and gum bleaching were seldom reported in the present study, which were in accordance with previous studies reporting no major side effects among children.20,31,32 This finding can be attributed to the diffusion of SDF onto surrounding tissues, resulting in temporary irritation of gingiva that subsided within days.17
The majority of parents/guardians in the present survey were satisfied with both treatments in terms of ease of application, painlessness of the process and material taste compromising their child's aesthetic appearance. These findings were in accordance with several studies13,18,33 and can be attributed to the fact that parents/guardians may perceive the discolouration from SDF in anterior teeth as being unaesthetic, but most parents/guardians are open to compromise aesthetics in favour of using a less invasive approach, especially when the child's co-operation becomes a barrier for traditional treatment to avoid the possibility of their children having to undergo sedation or general anaesthesia.3,28
Since parents/guardians may not have other affordable options for treating and alleviating pain in their children, the simplicity and cost-effectiveness of SDF make it a very favourable treatment for children of lower socioeconomic status.6
Conclusions
Based on the results of our study, both SDF and SDF/KI were effective in arresting carious lesions in primary anterior teeth but the application of KI didn't prevent the discolouration caused by SDF application. No adverse events were reported with both materials. Although parents/guardians perceived the discolouration, they were open to compromising aesthetics in favour of using a less invasive approach.
References
Abdellatif H M, Ali A M, Baghdady S I, ElKateb M A. Caries arrest effectiveness of silver diamine fluoride compared to alternative restorative technique: randomized clinical trial. Eur Arch Paediatr Dent 2021; 22: 575-585.
Garg S, Sadr S, Chan D. Potassium Iodide Reversal of Silver Diamine Fluoride Staining: A Case Report. Oper Dent 2019; 44: 221-226.
Crystal Y O, Janal M N, Hamilton D S, Niederman R. Parental perceptions and acceptance of silver diamine fluoride staining. J Am Dent Assoc 2017; 148: 510-518.
Gao S S, Amarquaye G, Arrow P et al. Global Oral Health Policies and Guidelines: Using Silver Diamine Fluoride for Caries Control. Front Oral Heal 2021; DOI: 10.3389/froh.2021.685557.
Roberts A, Bradley J, Merkley S, Pachal T, Gopal J V, Sharma D. Does potassium iodide application following silver diamine fluoride reduce staining of tooth? A systematic review. Aust Dent J 2020; 65: 109-117.
Sabbagh H, Othman M, Khogeer L, Al-Harbi H, Al Harthi A, Abdulgader Yaseen Abdulgader A. Parental acceptance of silver Diamine fluoride application on primary dentition: a systematic review and meta-analysis. BMC Oral Health 2020; 20: 227.
Fröhlich T T, Gindri L D O, Pedrotti D, Cavalheiro C P, Soares F Z M, de Oliverira Rocha R. Evaluation of the Use of Potassium Iodide Application on Stained Demineralized Dentin Under Resin Composite Following Silver Diamine Fluoride Application. Paediatr Dent 2021; 43: 57-61.
Sarkis-Onofre R, Poletto-Neto V, Cenci M S, Moher D, Pereira-Cenci T. CONSORT endorsement improves the quality of reports of randomized clinical trials in dentistry. J Clin Epidemiol 2020; 122: 20-26.
Sealed Envelope Ltd. Power calculator for continuous outcome superiority trial. 2012. Available at https://www.sealedenvelope.com/power/continuous-superiority/ (accessed November 2022).
Nguyen V, Neill C, Felsenfeld J, Primus C. Potassium Iodide. The Solution to Silver Diamine Fluoride Discoloration? Adv Dent Oral Heal 2017; 5: 1-6.
World Medical Association Inc. Declaration of Helsinki. Ethical principles for medical research involving human subjects. J Indian Med Assoc 2009; 107: 403-405.
Pitts N B, Ekstrand K, ICDAS Foundation. International Caries Detection and Assessment System (ICDAS) and its International Caries Classification and Management System (ICCMS) - methods for staging of the caries process and enabling dentists to manage caries. Community Dent Oral Epidemiol 2013; DOI: 10.1111/cdoe.12025.
Clemens J, Gold J, Chaffin J. Effect and acceptance of silver diamine fluoride treatment on dental caries in primary teeth. J Public Health Dent 2018; 78: 63-68.
Oliveira B H, Rajendra A, Veitz-Keenan A, Niederman R. The Effect of Silver Diamine Fluoride in Preventing Caries in the Primary Dentition: A Systematic Review and Meta-Analysis. Caries Res 2019; 53: 24-32.
Haiat A, Ngo H C, Samaranayake L P, Fakhruddin K S. The effect of the combined use of silver diamine fluoride and potassium iodide in disrupting the plaque biofilm microbiome and alleviating tooth discoloration: A systematic review. PLoS One 2021; DOI: 10.1371/journal.pone.0252734.
Li R, Lo E C M, Liu B Y, Wong M C M, Chu C H. Randomized clinical trial on arresting dental root caries through silver diammine fluoride applications in community-dwelling elders. J Dent 2016; 51: 15-20.
Turton B, Horn R, Durward C. Caries arrest and lesion appearance using two different silver fluoride therapies with and without potassium iodide: 6-month results. Heliyon 2020; DOI: 10.1016/j.heliyon.2020.e04287.
Vollú A, Rodrigues G, Rougemount Teixeira R et al. Efficacy of 30% silver diamine fluoride compared to atraumatic restorative treatment on dentine caries arrestment in primary molars of preschool children: A 12-months parallel randomized controlled clinical trial. J Dent 2019; 88: 103165.
Gao S S, Zhao I S, Hiraishi N et al. Clinical Trials of Silver Diamine Fluoride in Arresting Caries among Children: A Systematic Review. JDR Clin Trans Res 2016; 1: 201-210.
Rosenblatt A, Stamford T C M, Niederman R. Silver diamine fluoride: A caries 'silver-fluoride bullet'. J Dent Res 2009; 88: 116-125.
Fung M H T, Duangthip D, Wong M C M, Lo E C M, Chu C H. Arresting Dentine Caries with Different Concentration and Periodicity of Silver Diamine Fluoride. JDR Clin Trans Res 2016; 1: 143-152.
Mei M L, Lo E C M, Chu C H. Arresting Dentine Caries with Silver Diamine Fluoride: What's Behind It? J Dent Res 2018; 97: 751-758.
Thanatvarakorn O, Islam S, Nakashima S, Sadr A, Nikaido T, Tagami J. Effects of zinc fluoride on inhibiting dentin demineralization and collagen degradation in vitro: A comparison of various topical fluoride agents. Dent Mater J 2016; 35: 769-775.
Sayed M, Matsui N, Hiraishi N, Nikaido T, Burrow M F, Tagami J. Effect of Glutathione Bio-Molecule on Tooth Discoloration Associated with Silver Diammine Fluoride. Int J Mol Sci 2018; 19: 1322.
AlGhazali N, Burnside G, Smith R W, Preston A J, Jarad F D. Performance assessment of Vita Easy Shade spectrophotometer on colour measurement of aesthetic dental materials. Eur J Prosthodont Restor Dent 2011; 19: 168-174.
Zhao I S, Mei M L, Burrow M F, Lo E C-M, Chu C-H. Effect of Silver Diamine Fluoride and Potassium Iodide Treatment on Secondary Caries Prevention and Tooth Discolouration in Cervical Glass Ionomer Cement Restoration. Int J Mol Sci 2017; 18: 340.
Gupte M, Saraf T, Jawdekar A M, Khare D S, Tiku A. A comparative analysis of staining propensity of SDF, SDF with potassium iodide and SDF with glutathione biomolecule on demineralized enamel: An in vitro study. Int J Appl Dent Sci 2021; 7: 297-301.
Vennela E, Sharada J, Hasanuddin S, Suhasini K, Haemachandrika I, Singh I. Comparison of staining potential of silver diamine fluoride versus silver diamine fluoride and potassium iodide under tooth-coloured restorations: An in vitro study. J Indian Soc Pedod Prev Dent 2021; 39: 47-52.
Zhao I S, Chu S, Yu O Y, Mei M L, Chu C H, Lo E C M. Effect of silver diamine fluoride and potassium iodide on shear bond strength of glass ionomer cements to caries-affected dentine. Int Dent J 2019; 69: 341-347.
Miller M B, López L A, Quock R L. Silver diamine fluoride, potassium iodide, and esthetic perception: An in vitro pilot study. Am J Dent 2016; 29: 248-250.
Duangthip D, Jiang M, Chu C H, Lo E C M. Non-surgical treatment of dentin caries in preschool children - systematic review. BMC Oral Health 2015; 15: 44.
Duangthip D, Fung M H T, Wong M C M, Chu C H, Lo E C M. Adverse Effects of Silver Diamine Fluoride Treatment among Preschool Children. J Dent Res 2018; 97: 395-401.
Chaurasiya A, Gojanur S. Evaluation of the clinical efficacy of 38% silver diamine fluoride in arresting dental caries in primary teeth and its parental acceptance. J Indian Soc Pedod Prev Dent 2021; 39: 85-89.
Acknowledgements
The authors acknowledge the children and their parents/guardians for their co-operation in accomplishing this work.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Mariam M. Mohsen and Yasmin M. Yousry contributed to the study's conception and design, material preparation, data collection and analysis. The first draft of the manuscript was written by Mariam Mohsen and Yasmin Yousry contributed. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
This study was approved by the Ethics Committee of Scientific Research, Faculty of Dentistry, Cairo University with approval number 19-12-23. The research was carried out in accordance with the Declaration of Helsinki. Written informed consent to participate was obtained from the children's parents/guardians.
The authors have no relevant financial or non-financial interests to disclose.
Rights and permissions
About this article
Cite this article
Aly, ., Yousry, Y. Potential discolouration of silver diamine fluoride versus silver diamine fluoride/potassium iodide in primary teeth: a randomised clinical study. Br Dent J (2022). https://doi.org/10.1038/s41415-022-5272-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-022-5272-9