Abstract
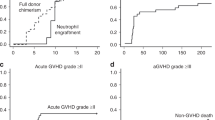
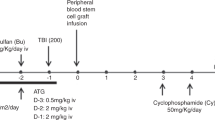
Allogeneic hematopoietic stem cell transplantation (HSCT) currently stands as the sole remedy for individuals afflicted with hemophagocytic lymphohistiocytosis (HLH). In this study, we retrospectively evaluated how pediatric patients with relapsed or refractory (R/R) HLH responded to our institution’s cocktail conditioning regimen. The disease was diagnosed according to criteria applicable to patients with familial/genetic, relapsing, or severe/persistent HLH. All donors were HLA haplo-identical family donors. In our cohort, sixty-five patients (P-HLH), including 28 with familial/genetic HLH, 36 with secondary HLH, and 1 with an unknown cause, underwent haplo-identical family donor HSCT. The conditioning regimen consisted of intravenous administration of etoposide (VP-16), busulfan, fludarabine, rabbit anti-human thymocyte globulin (r-ATG), and cyclophosphamide (Cy). Tacrolimus and mycophenolate mofetil were used for graft-versus-host disease (GvHD) prevention. We observed that the median time for neutrophil recovery was 11 days (range, 8–24), and for platelet counts to exceed 20 × 109/L, it was 14 days (range, 7–130). There were 5 patients (7.7%) who experienced grades III to IV acute GvHD, and 6 patients (9.2%) developed extensive chronic GvHD. The estimated 3- and 5-year overall survival rates were 78.1% (95% CI, 65.8–84.6%) and 74.9% (95% CI, 61.2–84.4%), respectively. The estimated 3- and 5-year event-free survival rates were 73.5% (95% CI, 60.8–82.6%) and 70.3% (95% CI, 56.4–80.5%), respectively. Our findings demonstrate that our innovative conditioning regimen is both effective and safe, offering valuable insights for healthcare professionals evaluating the merits of existing therapies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Detailed data are available upon request to corresponding author.
References
Janka GE. Familial hemophagocytic lymphohistiocytosis: diagnostic problems and differential diagnosis. Pediatr Hematol Oncol. 1989;6:219–25. https://doi.org/10.3109/08880018909034290.
Janka GE. Familial hemophagocytic lymphohistiocytosis. Eur J Pediatr. 1983;140:221–30. https://doi.org/10.1007/BF00443367.
Bergsten E, Horne A, Hed Myrberg I, Arico M, Astigarraga I, Ishii E, et al. Stem cell transplantation for children with hemophagocytic lymphohistiocytosis: results from the HLH-2004 study. Blood Adv. 2020;4:3754–66. https://doi.org/10.1182/bloodadvances.2020002101.
Kawa K, Sawada A, Sato M, Okamura T, Sakata N, Kondo O, et al. Excellent outcome of allogeneic hematopoietic SCT with reduced-intensity conditioning for the treatment of chronic active EBV infection. Bone Marrow Transpl. 2011;46:77–83. https://doi.org/10.1038/bmt.2010.122.
Sandler RD, Carter S, Kaur H, Francis S, Tattersall RS, Snowden JA. Haemophagocytic lymphohistiocytosis (HLH) following allogeneic haematopoietic stem cell transplantation (HSCT)-time to reappraise with modern diagnostic and treatment strategies? Bone Marrow Transpl. 2020;55:307–16. https://doi.org/10.1038/s41409-019-0637-7.
Brisse E, Wouters CH, Matthys P. Advances in the pathogenesis of primary and secondary haemophagocytic lymphohistiocytosis: differences and similarities. Br J Haematol. 2016;174:203–17. https://doi.org/10.1111/bjh.14147.
Arico M, Imashuku S, Clementi R, Hibi S, Teramura T, Danesino C, et al. Hemophagocytic lymphohistiocytosis due to germline mutations in SH2D1A, the X-linked lymphoproliferative disease gene. Blood. 2001;97:1131–3. https://doi.org/10.1182/blood.v97.4.1131.
Stepp SE, Dufourcq-Lagelouse R, Le Deist F, Bhawan S, Certain S, et al. Perforin gene defects in familial hemophagocytic lymphohistiocytosis. Science. 1999;286:1957–9. https://doi.org/10.1126/science.286.5446.1957.
Cooper N, Rao K, Gilmour K, Hadad L, Adams S, Cale C, et al. Stem cell transplantation with reduced-intensity conditioning for hemophagocytic lymphohistiocytosis. Blood. 2006;107:1233–6. https://doi.org/10.1182/blood-2005-05-1819.
Marsh RA, Jordan MB, Filipovich AH. Reduced-intensity conditioning haematopoietic cell transplantation for haemophagocytic lymphohistiocytosis: an important step forward. Br J Haematol. 2011;154:556–63. https://doi.org/10.1111/j.1365-2141.2011.08785.x.
Baker KS, Filipovich AH, Gross TG, Grossman WJ, Hale GA, Hayashi RJ, et al. Unrelated donor hematopoietic cell transplantation for hemophagocytic lymphohistiocytosis. Bone Marrow Transpl. 2008;42:175–80. https://doi.org/10.1038/bmt.2008.133.
Dahlberg A, Kurtzberg J, Boelens J, Martinez C, Carpenter P, Tewari P, et al. Guidelines for Pediatric Unrelated Cord Blood Transplantation-Unique Considerations. Transpl Cell Ther. 2021;27:968–72. https://doi.org/10.1016/j.jtct.2021.09.013.
Horne A, Trottestam H, Arico M, Egeler RM, Filipovich AH, Gadner H, et al. Frequency and spectrum of central nervous system involvement in 193 children with haemophagocytic lymphohistiocytosis. Br J Haematol. 2008;140:327–35. https://doi.org/10.1111/j.1365-2141.2007.06922.x.
Cesaro S, Locatelli F, Lanino E, Porta F, Di Maio L, Messina C, et al. Hematopoietic stem cell transplantation for hemophagocytic lymphohistiocytosis: a retrospective analysis of data from the Italian Association of Pediatric Hematology Oncology (AIEOP). Haematologica. 2008;93:1694–701. https://doi.org/10.3324/haematol.13142.
Allen CE, Marsh R, Dawson P, Bollard CM, Shenoy S, Roehrs P, et al. Reduced-intensity conditioning for hematopoietic cell transplant for HLH and primary immune deficiencies. Blood. 2018;132:1438–51. https://doi.org/10.1182/blood-2018-01-828277.
Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–31. https://doi.org/10.1002/pbc.21039.
Messina C, Zecca M, Fagioli F, Rovelli A, Giardino S, Merli P, et al. Outcomes of Children with Hemophagocytic Lymphohistiocytosis Given Allogeneic Hematopoietic Stem Cell Transplantation in Italy. Biol Blood Marrow Transpl. 2018;24:1223–31. https://doi.org/10.1016/j.bbmt.2018.01.022.
Wei A, Ma HH, Zhang LP, Lian HY, Du JY, Wang D, et al. Ruxolitinib combined with liposomal doxorubicin, etoposide, methylprednisolone+/-PEG-asparaginase in treatment of relapsed/refractory pediatric hemophagocytic lymphohistiocytosis. Zhonghua Yi Xue Za Zhi. 2022;102:2167–72. https://doi.org/10.3760/cma.j.cn112137-20211224-02888
Ciurea SO, Cao K, Fernandez-Vina M, Kongtim P, Malki MA, Fuchs E, et al. The European Society for Blood and Marrow Transplantation (EBMT) Consensus Guidelines for the Detection and Treatment of Donor-specific Anti-HLA Antibodies (DSA) in Haploidentical Hematopoietic Cell Transplantation. Bone Marrow Transpl. 2018;53:521–34. https://doi.org/10.1038/s41409-017-0062-8.
Marsh RA, Allen CE, McClain KL, Weinstein JL, Kanter J, Skiles J, et al. Salvage therapy of refractory hemophagocytic lymphohistiocytosis with alemtuzumab. Pediatr Blood Cancer. 2013;60:101–9. https://doi.org/10.1002/pbc.24188.
Olsson R, Remberger M, Schaffer M, Berggren DM, Svahn BM, Mattsson J, et al. Graft failure in the modern era of allogeneic hematopoietic SCT. Bone Marrow Transpl. 2013;48:537–43. https://doi.org/10.1038/bmt.2012.239.
Ali S, Wall DA, Ali M, Chiang KY, Naqvi A, Weitzman S, et al. Effect of different conditioning regimens on survival and engraftment for children with hemophagocytic lymphohistiocytosis undergoing allogeneic hematopoeitic stem cell transplantation: A single institution experience. Pediatr Blood Cancer. 2020;67:e28477. https://doi.org/10.1002/pbc.28477.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transpl. 1995;15:825–8.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: I. The 2014 Diagnosis and Staging Working Group report. Biol Blood Marrow Transpl. 2015;21:389–401.e381. https://doi.org/10.1016/j.bbmt.2014.12.001.
Bosnak M, Erdogan S, Aktekin EH, Bay A. Therapeutic plasma exchange in primary hemophagocytic lymphohistiocytosis: Reports of two cases and a review of the literature. Transfus Apher Sci. 2016;55:353–6. https://doi.org/10.1016/j.transci.2016.09.015.
Patel SA, Allewelt HA, Troy JD, Martin PL, Driscoll TA, Prasad VK, et al. Durable Chimerism and Long-Term Survival after Unrelated Umbilical Cord Blood Transplantation for Pediatric Hemophagocytic Lymphohistiocytosis: A Single-Center Experience. Biol Blood Marrow Transpl. 2017;23:1722–8. https://doi.org/10.1016/j.bbmt.2017.06.013.
Cooper N, Rao K, Goulden N, Webb D, Amrolia P, Veys P. The use of reduced-intensity stem cell transplantation in haemophagocytic lymphohistiocytosis and Langerhans cell histiocytosis. Bone Marrow Transpl. 2008;42:S47–50. https://doi.org/10.1038/bmt.2008.283.
Eapen M, Ahn KW, Orchard PJ, Cowan MJ, Davies SM, Fasth A, et al. Long-term survival and late deaths after hematopoietic cell transplantation for primary immunodeficiency diseases and inborn errors of metabolism. Biol Blood Marrow Transpl. 2012;18:1438–45. https://doi.org/10.1016/j.bbmt.2012.03.003.
Felber M, Steward CG, Kentouche K, Fasth A, Wynn RF, Zeilhofer U, et al. Targeted busulfan-based reduced-intensity conditioning and HLA-matched HSCT cure hemophagocytic lymphohistiocytosis. Blood Adv. 2020;4:1998–2010. https://doi.org/10.1182/bloodadvances.2020001748.
Abdelkefi A, Ben Othman T, Torjman L, Ladeb S, Lakhal A, Belhadj S, et al. Plasmodium falciparum causing hemophagocytic syndrome after allogeneic blood stem cell transplantation. Hematol J. 2004;5:449–50. https://doi.org/10.1038/sj.thj.6200531.
Baker KS, DeLaat CA, Steinbuch M, Gross TG, Shapiro RS, Loechelt B, et al. Successful correction of hemophagocytic lymphohistiocytosis with related or unrelated bone marrow transplantation. Blood. 1997;89:3857–63.
Author information
Authors and Affiliations
Contributions
YY, SF and YS designed, wrote and revised the manuscript. YY, ZL, YS, FJ, SF collected data and provided clinical care. YY, JC and JQ analyzed the clinical data. All authors approved the final manuscript for publication.
Corresponding author
Ethics declarations
Competing interests
Author JQ was employed by Acornmed Biotechnology Co., Ltd. The remaining authors declare that the research was conducted without any commercial or financial relationships that could be considered potential conflicts of interest.
Ethics approval
Informed consent was obtained from the patients/participants included in the study. All procedures conducted in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, and they were conducted following the Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yue, Y., Fan, S., Liu, Z. et al. Sequential haplo-identical conditioning transplant regimen for pediatric patients with relapsed or refractory hemophagocytic lymphohistiocytosis. Bone Marrow Transplant 59, 513–517 (2024). https://doi.org/10.1038/s41409-024-02212-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-024-02212-7