Abstract
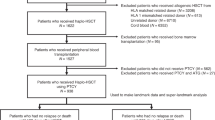
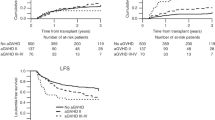
Second transplantation (HSCT2) is a potential treatment for primary graft failure (pGF). We assessed the outcome of HSCT2, performed between 2000 and 2021, for pGF in 243 patients with acute leukemia. Median age was 44.8 years. Conditioning at first HSCT (HSCT1) was myeloablative (MAC) in 58.4%. Median time from HSCT1 to HSCT2 was 48 days. Donors for HSCT2 were the same as for HSCT1 in 49%. Engraftment post HSCT2 was achieved by 73.7% of patients. The incidence of acute (a) graft versus host disease (GVHD) grades II-IV and III-IV was 23.2 and 8.1%. 5-year total and extensive chronic (c) GVHD was 22.3 and 10.1%. 5-year nonrelapse mortality (NRM), relapse incidence (RI), leukemia-free survival (LFS), overall survival (OS) and GVHD free, relapse-free survival (GRFS) was 51.6, 18.8, 29.6, 30.7 and 22.4%, respectively. Infections were the main cause of death. In multivariable analysis, being transplanted at second vs. first remission, lower Karnofsky performance status (KPS; <90) and receiving MAC at HSCT1 were adverse prognostic factors for NRM, LFS, OS, and GRFS, as was increased age for NRM, LFS, OS. We conclude that HSCT2 can rescue about a third of the patients who experienced pGF, but NRM is as high as 50%.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
AN, ML, and MM had full access to all study data (available upon data-specific request).
References
Kharfan-Dabaja MA, Kumar A, Ayala E, Aljurf M, Nishihori T, Marsh R, et al. Standardizing definitions of hematopoietic recovery, graft rejection, graft failure, poor graft function, and donor chimerism in allogeneic hematopoietic cell transplantation: a report on behalf of the American Society for Transplantation and Cellular Therapy. Transpl Cell Ther. 2021;27:642–9.
Chen J, Pang A, Zhao Y, Liu L, Ma R, Wei J, et al. Primary graft failure following allogeneic hematopoietic stem cell transplantation: risk factors, treatment and outcomes. Hematology. 2022;27:293–9. https://doi.org/10.1080/16078454.2022.2042064
Park JH, Lee JH, Lee JH, Park HS, Choi EJ, Kang YA, et al. Incidence, management, and prognosis of graft failure and autologous reconstitution after allogeneic hematopoietic stem cell transplantation. J Korean Med Sci. 2021;36:e151. https://doi.org/10.3346/jkms.2021.36.e151
Schriber J, Agovi MA, Ho V, Ballen KK, Bacigalupo A, Lazarus HM, et al. Second unrelated donor hematopoietic cell transplantation for primary graft failure. Biol Blood Marrow Transpl. 2010;16:1099–106. https://doi.org/10.1016/j.bbmt.2010.02.013
Davies SM, Kollman C, Anasetti C, Antin JH, Gajewski J, Casper JT, et al. Engraftment and survival after unrelated-donor bone marrow transplantation: a report from the national marrow donor program. Blood. 2000;96:4096–102.
Rubinstein P, Carrier C, Scaradavou A, Kurtzberg J, Adamson J, Migliaccio AR, et al. Outcomes among 562 recipients of placental-blood transplants from unrelated donors. N. Engl J Med. 1998;339:1565–77. https://doi.org/10.1056/NEJM199811263392201
Servais S, Beguin Y, Baron F. Emerging drugs for prevention of graft failure after allogeneic hematopoietic stem cell transplantation. Expert Opin Emerg Drugs. 2013;18:173–92.
Ruggeri A, Labopin M, Angelucci E, Blaise D, Ciceri F, Koc Y, et al. Prognostic factors for neutrophil engraftment after haploidentical cell transplantation with PT-Cy in patients with acute myeloid leukemia in complete remission, on behalf of the ALWP-EBMT. Bone Marrow Transpl. 2021;56:1842–9.
Chakrabarty JH, Glover J, Schmidt S, Phan M, Bycko M, Duong Q, et al. Incidence and risk factors for graft failure in the modern era of cord blood transplantation. Vox Sang. 2022;117:1405–10.
Ciurea SO, Cao K, Fernandez-Vina M, Kongtim P, Malki MA, Fuchs E, et al. The European society for blood and marrow transplantation (EBMT) consensus guidelines for the detection and treatment of donor-specific anti-HLA antibodies (DSA) in haploidentical hematopoietic cell transplantation. Bone Marrow Transpl. 2018;53:521–34.
Guru Murthy GS, Logan BR, Bo-Subait S, Beitinjaneh A, Devine S, Farhadfar N, et al. Association of ABO mismatch with the outcomes of allogeneic hematopoietic cell transplantation for acute leukemia. Am J Hematol. 2023;98:608–19.
Olsson R, Remberger M, Schaffer M, Berggren DM, Svahn BM, Mattsson J, et al. Bone Marrow Transplant. Erratum : Bone Marrow Transpl. 2013;48:537–43. https://doi.org/10.1038/bmt.2012.239
Cluzeau T, Lambert J, Raus N, Dessaux K, Absi L, Delbos F, et al. Risk factors and outcome of graft failure after HLA matched and mismatched unrelated donor hematopoietic stem cell transplantation: a study on behalf of SFGM-TC and SFHI. Bone Marrow Transpl. 2016;51:687–91. https://doi.org/10.1038/bmt.2015.351
Ferrà C, Sanz J, Díaz-Pérez MA, Morgades M, Gayoso J, Cabrera JR, et al. Grupo Español de Trasplante Hematopoyético (Geth) Spanish Society of Hematology. Outcome of graft failure after allogeneic stem cell transplant: study of 89 patients. Leuk Lymphoma. 2015;56:656–62. https://doi.org/10.3109/10428194.2014.930849
Moscardó F, Romero S, Sanz J, Sanz MA, Montesinos P, Lorenzo I, et al. T cell-depleted related HLA-mismatched peripheral blood stem cell transplantation as salvage therapy for graft failure after single unit unrelated donor umbilical cord blood transplantation. Biol Blood Marrow Transpl. 2014;20:1060–3. https://doi.org/10.1016/j.bbmt.2014.03.024
Rondón G, Saliba RM, Khouri I, Giralt S, Chan K, Jabbour E, et al. Long-term follow-up of patients who experienced graft failure post allogeneic progenitor cell transplantation. Results of a single institution analysis. Biol Blood Marrow Transpl. 2008;14:859–66. https://doi.org/10.1016/j.bbmt.2008.05.005
Sun Y-Q, Wang Y, Wang F-R, Yan C-H, Cheng Y-F, Chen Y-H, et al. Graft failure in patients with hematological malignancies: a successful salvage with a second transplantation from a different haploidentical donor. Front Med. 2021;8:604085 https://doi.org/10.3389/fmed.2021.604085
Giammarco S, Raiola AM, Di Grazia C, Bregante S, Gualandi F, Varaldo R, et al. Second haploidentical stem cell transplantation for primary graft failure. Bone Marrow Transpl. 2021;56:1291–6. https://doi.org/10.1038/s41409-020-01183-9
Fuji S, Nakamura F, Hatanaka K, Taniguchi S, Sato M, Mori S, et al. Peripheral blood as a preferable source of stem cells for salvage transplantation in patients with graft failure after cord blood transplantation: a retrospective analysis of the registry data of the Japanese Society for Hematopoietic Cell Transplantation. Biol Blood Marrow Transpl. 2012;18:1407–14. https://doi.org/10.1016/j.bbmt.2012.02.014
Harada K, Fuji S, Seo S, Kanda J, Ueki T, Kimura F, et al. Transplant complications working group of the Japan Society for Hematopoietic Cell Transplantation. Comparison of the outcomes after haploidentical and cord blood salvage transplantations for graft failure following allogeneic hematopoietic stem cell transplantation. Bone Marrow Transpl. 2020;55:1784–95. https://doi.org/10.1038/s41409-020-0821-9
Shouval R, Fein JA, Labopin M, Kröger N, Duarte RF, Bader P, et al. Outcomes of allogeneic haematopoietic stem cell transplantation from HLA-matched and alternative donors: a European Society for Blood and Marrow Transplantation registry retrospective analysis. Lancet Haematol. 2019;6:e573–84.
Passweg JR, Baldomero H, Chabannon C, Basak GW, de la Cámara R, Corbacioglu S, et al. Hematopoietic cell transplantation and cellular therapy survey of the EBMT: monitoring of activities and trends over 30 years.; European Society for Blood and Marrow Transplantation (EBMT). Bone Marrow Transpl. 2021;56:1651–64.
Phelan R, Chen M, Bupp C, Bolon YT, Broglie L, Brunner-Grady J, et al. Updated trends in hematopoietic cell transplantation in the United States with an additional focus on adolescent and young adult transplantation activity and outcomes. Transpl Cell Ther. 2022;28:409.e1–9.e10.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transpl. 2009;15:1628–33.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transpl. 1995;15:825–8.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE, et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med. 1980;69:204–17.
Ruggeri A, Labopin M, Ciceri F, Mohty M, Nagler A. Definition of GvHD-free, relapse-free survival for registry-based studies: an ALWP-EBMT analysis on patients with AML in remission. Bone Marrow Transpl. 2016;51:610–11.
Kanate AS, Nagler A, Savani B. Summary of scientific and statistical methods, study endpoints and definitions for observational and registry-based studies in hematopoietic cell transplantation. Clin Hematol Int. 2019;2:2–4.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2020. https://www.R-project.org/
Nagler A, Mohty M. In 2022, which is preferred: haploidentical or cord transplant? Hematol Am Soc Hematol Educ Program. 2022;2022:64–73.
Nakamura H, Gress RE. Graft rejection by cytolytic T cells. Specificity of the effector mechanism in the rejection of allogeneic marrow. Transplantation. 1990;49:453–8.
Masouridi-Levrat S, Simonetta F, Chalandon Y. Immunological basis of bone marrow failure after allogeneic hematopoietic stem cell transplantation. Front Immunol. 2016;7:362. https://doi.org/10.3389/fimmu.2016.00362
Aversa F, Velardi A, Tabilio A, Reisner Y, Martelli MF. Haploidentical stem cell transplantation in leukemia. Blood Rev. 2001;15:111–9.
Reisner Y, Hagin D, Martelli MF. Haploidentical hematopoietic transplantation: current status and future perspectives. Blood 2011;118:6006–17.
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transpl. 2008;14:641–50. https://doi.org/10.1016/j.bbmt.2008.03.005
Fuchs EJ. HLA-haploidentical blood or marrow transplantation with high-dose, post-transplantation cyclophosphamide. Bone Marrow Transpl. 2015;50:S31–6. https://doi.org/10.1038/bmt.2015.92.
Robinson TM, Fuchs EJ, Zhang MJ, St Martin A, Labopin M, Keesler DA, et al. Acute Leukemia Working Party of the European Society for Blood and Marrow Transplant and the Center for International Blood and Marrow Transplant Research. Related donor transplants: has posttransplantation cyclophosphamide nullified the detrimental effect of HLA mismatch? Blood Adv. 2018;2:1180–6. https://doi.org/10.1182/bloodadvances.2018018291
Gooptu M, Romee R, St Martin A, Arora M, Al Malki M, Antin JH, et al. HLA-haploidentical vs matched unrelated donor transplants with posttransplant cyclophosphamide-based prophylaxis. Blood. 2021;138:273–82. https://doi.org/10.1182/blood.2021011281
Shimoni A, Labopin M, Finke J, Ciceri F, Deconinck E, Kröger N, et al. Donor selection for a second allogeneic stem cell transplantation in AML patients relapsing after a first transplant: a study of the Acute Leukemia Working Party of EBMT. Blood Cancer J. 2019;9:88.
Yerushalmi Y, Shem-Tov N, Danylesko I, Canaani J, Avigdor A, Yerushalmi R, et al. Second hematopoietic stem cell transplantation as salvage therapy for relapsed acute myeloid leukemia/ myelodysplastic syndromes after a first transplantation. Haematologica. 2022. https://doi.org/10.3324/haematol.2022.281877
Hickey CL, Zhang MJ, Johnson MA, Romee R, Milano F, Brunstein CG, et al. Late Graft Failure in MDS and Acute Leukemia Patients Receiving Allogenic Hematopoietic Cell Transplantation with Post Transplant Cyclophosphamide as GVHD Prophylaxis. ASH 2022 Abstract 369.
Harada K, Najima Y, Kato M, Fuji S, Shinohara A, Nakamae H, et al. Outcomes of salvage haploidentical transplantation using posttransplant cyclophosphamide for graft failure following allogeneic hematopoietic stem cell transplantation. Int J Hematol. 2022;116:744–53. https://doi.org/10.1007/s12185-022-03405-w
Rudakova T, Moiseev I, Morozova E, Vlasova J, Vitrishchak A, Kulagin A. Combination of Fludarabine and cyclophosphamide as conditioning regimen in second HSCT for graft failure (EBMT 2023 abstract P551).
Volt F, Ruggeri A, Scigliuolo GM, de Latour RP, Bierings M, Al-Seraihy A, et al. Umbilical cord blood transplantation after graft failure from a previous hematopoietic stem cell transplantation. Transpl Cell Ther. 2022;28:46.e1–e7. https://doi.org/10.1016/j.jtct.2021.10.014
Konuma T, Harada K, Kondo T, Masuko M, Uchida N, Yano S, et al. Adult Acute Myeloid Leukemia Working Group of the Japanese Society for Transplantation and Cellular Therapy. Salvage single-unit unrelated cord blood transplantation for graft failure following initial allogeneic transplantation in adult acute myeloid leukemia: trends in outcomes over the past 20 years. Bone Marrow Transpl. 2022;57:1848–50. https://doi.org/10.1038/s41409-022-01840-1
Nagler A, Labopin M, Dholaria B, Finke J, Brecht A, Schanz U, et al. Second allogeneic stem cell transplantation in patients with acute lymphoblastic leukaemia: a study on behalf of the Acute Leukaemia Working Party of the European Society for Blood and Marrow Transplantation. Br J Haematol. 2019;186:767–76.
Christopeit M, Kuss O, Finke J, Bacher U, Beelen DW, Bornhäuser M, et al. Second allograft for hematologic relapse of acute leukemia after first allogeneic stem-cell transplantation from related and unrelated donors: the role of donor change. J Clin Oncol Sept. 2013;31:3259–71.
Ortí G, Sanz J, García-Cadenas I, Sánchez-Ortega I, Alonso L, Jiménez MJ, et al. Analysis of relapse after transplantation in acute leukemia: A comparative on second allogeneic hematopoietic cell transplantation and donor lymphocyte infusions. Exp Hematol. 2018;62:24–32.
Guardiola P, Kuentz M, Garban F, Blaise D, Reiffers J, Attal M, et al. French Society of Bone Marrow Transplantation. Second early allogeneic stem cell transplantations for graft failure in acute leukemia, chronic myeloid leukemia and aplastic anemia. Br J Haematol. 2000;111:292–302.
Platzbecker U, Binder M, Schmid C, Rutt C, Ehninger G, Bornhäuser M. Second donation of hematopoietic stem cells from unrelated donors for patients with relapse or graft-failure after allogeneic transplantation. Haematologica. 2008;93:1276–8.
Author information
Authors and Affiliations
Contributions
AN wrote the manuscript, designed the study, and interpreted the data. RS helped writing the first draft of the manuscript and reviewed the manuscript. ML and MM designed the study, performed the statistical analyses, interpreted the data, and edited the manuscript. AK, AV, JS, HLW, VP, JK, SS, EP, WB, XL, UP, FS, FC reviewed the manuscript and provided clinical data. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The scientific boards of the ALWP of the EBMT approved this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nagler, A., Labopin, M., Swoboda, R. et al. Long-term outcome of second allogeneic hematopoietic stem cell transplantation (HSCT2) for primary graft failure in patients with acute leukemia in remission: A study on behalf of the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Bone Marrow Transplant 58, 1008–1016 (2023). https://doi.org/10.1038/s41409-023-02012-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-02012-5