Abstract
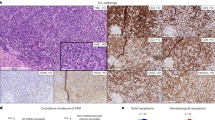
Pre-transplant detectable measurable residual disease (MRD) is still associated with high risk of relapse and poor outcomes in acute myeloid leukemia (AML). We aimed at evaluating the impact of disease burden on prediction of relapse and survival in patients receiving allogeneic hematopoietic cell transplantation (allo-HCT) in first remission (CR1). We identified a total of 3202 adult AML patients, of these 1776 patients were in CR1 and MRD positive and 1426 patients were primary refractory at time of transplant. After a median follow-up of 24.4 months, non-relapse mortality and relapse rate were significantly higher in the primary refractory group compared to the CR1 MRD positive group (Hazards Ratio (HR) = 1.82 (95% CI: 1.47–2.24) p < 0.001 and HR = 1.54 (95% CI: 1.34–1.77), p < 0.001), respectively. Leukemia-free survival (LFS) and overall survival (OS) were significantly worse in the primary refractory group (HR = 1.61 (95% CI: 1.44-1.81), p < 0.001 and HR = 1.71 (95% CI: 1.51–1.94), p < 0.001, respectively). Our real-life data suggest that patients in CR1 and MRD positive at time of transplant could still be salvaged by allo-HCT with a 2-year OS of 63%, if negative MRD cannot be obtained and their outcomes are significantly better than patients transplanted with active disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Upon request from the corresponding author.
References
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–47. https://doi.org/10.1182/blood-2016-08-733196.
Heuser M, Freeman SD, Ossenkoppele GJ, Buccisano F, Hourigan CS, Ngai LL, et al. 2021 Update on MRD in acute myeloid leukemia: a consensus document from the European LeukemiaNet MRD Working Party. Blood. 2021;138:2753–67. https://doi.org/10.1182/blood.2021013626.
Schuurhuis GJ, Heuser M, Freeman S, Bene MC, Buccisano F, Cloos J, et al. Minimal/measurable residual disease in AML: a consensus document from the European LeukemiaNet MRD Working Party. Blood. 2018;131:1275–91. https://doi.org/10.1182/blood-2017-09-801498.
Nagler A, Baron F, Labopin M, Polge E, Esteve J, Bazarbachi A, et al. Measurable residual disease (MRD) testing for acute leukemia in EBMT transplant centers: a survey on behalf of the ALWP of the EBMT. Bone Marrow Transpl. 2021;56:218–24. https://doi.org/10.1038/s41409-020-01005-y.
Buckley SA, Wood BL, Othus M, Hourigan CS, Ustun C, Linden MA, et al. Minimal residual disease prior to allogeneic hematopoietic cell transplantation in acute myeloid leukemia: a meta-analysis. Haematologica. 2017;102:865–73. https://doi.org/10.3324/haematol.2016.159343.
Walter RB, Gooley TA, Wood BL, Milano F, Fang M, Sorror ML, et al. Impact of pretransplantation minimal residual disease, as detected by multiparametric flow cytometry, on outcome of myeloablative hematopoietic cell transplantation for acute myeloid leukemia. J Clin Oncol. 2011;29:1190–7. https://doi.org/10.1200/jco.2010.31.8121.
Araki D, Wood BL, Othus M, Radich JP, Halpern AB, Zhou Y, et al. Allogeneic hematopoietic cell transplantation for acute myeloid leukemia: time to move toward a minimal residual disease-based definition of complete remission? J Clin Oncol. 2016;34:329–36. https://doi.org/10.1200/jco.2015.63.3826.
Zhou Y, Othus M, Araki D, Wood BL, Radich JP, Halpern AB, et al. Pre- and post-transplant quantification of measurable (‘minimal’) residual disease via multiparameter flow cytometry in adult acute myeloid. Leuk Leuk. 2016;30:1456–64. https://doi.org/10.1038/leu.2016.46.
Ustun C, Courville EL, DeFor T, Dolan M, Randall N, Yohe S, et al. Myeloablative, but not reduced-intensity, conditioning overcomes the negative effect of flow-cytometric evidence of leukemia in acute myeloid leukemia. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2016;22:669–75. https://doi.org/10.1016/j.bbmt.2015.10.024.
Morsink LM, Bezerra ED, Othus M, Wood BL, Fang M, Sandmaier BM, et al. Comparative analysis of total body irradiation (TBI)-based and non-TBI-based myeloablative conditioning for acute myeloid leukemia in remission with or without measurable residual disease. Leukemia. 2020;34:1701–5. https://doi.org/10.1038/s41375-019-0671-x.
Morsink LM, Sandmaier BM, Othus M, Palmieri R, Granot N, Bezerra ED, et al. Conditioning intensity, pre-transplant flow cytometric measurable residual disease, and outcome in adults with acute myeloid leukemia undergoing allogeneic hematopoietic cell transplantation. Cancers. 2020;12:2339.
Gilleece MH, Labopin M, Yakoub-Agha I, Volin L, Socié G, Ljungman P, et al. Measurable residual disease, conditioning regimen intensity, and age predict outcome of allogeneic hematopoietic cell transplantation for acute myeloid leukemia in first remission: A registry analysis of 2292 patients by the Acute Leukemia Working Party. Eur Soc Blood Marrow Transplant Am J Hematol. 2018;93:1142–52. https://doi.org/10.1002/ajh.25211.
Schlenk RF, Döhner K, Mack S, Stoppel M, Király F, Götze K, et al. Prospective evaluation of allogeneic hematopoietic stem-cell transplantation from matched related and matched unrelated donors in younger adults with high-risk acute myeloid leukemia: German-Austrian trial AMLHD98A. J Clin Oncol. 2010;28:4642–8. https://doi.org/10.1200/jco.2010.28.6856.
Duval M, Klein JP, He W, Cahn JY, Cairo M, Camitta BM, et al. Hematopoietic stem-cell transplantation for acute leukemia in relapse or primary induction failure. J Clin Oncol. 2010;28:3730–8. https://doi.org/10.1200/jco.2010.28.8852.
Le Bourgeois A, Labopin M, Marçais A, de Latour RP, Blaise D, Chantepie S, et al. Sequential allogeneic hematopoietic stem cell transplantation for active refractory/relapsed myeloid malignancies: results of a reduced-intensity conditioning preceded by clofarabine and cytosine arabinoside, a retrospective study on behalf of the SFGM-TC. Ann Hematol. 2020;99:1855–62. https://doi.org/10.1007/s00277-020-04074-7.
Malard F, Labopin M, Stuhler G, Bittenbring J, Ganser A, Tischer J, et al. Sequential intensified conditioning regimen allogeneic hematopoietic stem cell transplantation in adult patients with intermediate- or high-risk acute myeloid leukemia in complete remission: a study from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2017;23:278–84. https://doi.org/10.1016/j.bbmt.2016.11.002.
Schmid C, Schleuning M, Ledderose G, Tischer J, Kolb HJ. Sequential regimen of chemotherapy, reduced-intensity conditioning for allogeneic stem-cell transplantation, and prophylactic donor lymphocyte transfusion in high-risk acute myeloid leukemia and myelodysplastic syndrome. J Clin Oncol. 2005;23:5675–87. https://doi.org/10.1200/jco.2005.07.061.
Pfrepper C, Klink A, Behre G, Schenk T, Franke GN, Jentzsch M, et al. Risk factors for outcome in refractory acute myeloid leukemia patients treated with a combination of fludarabine, cytarabine, and amsacrine followed by a reduced-intensity conditioning and allogeneic stem cell transplantation. J Cancer Res Clin Oncol. 2016;142:317–24. https://doi.org/10.1007/s00432-015-2050-y.
Kebriaei P, Kline J, Stock W, Kasza K, Le Beau MM, Larson RA, et al. Impact of disease burden at time of allogeneic stem cell transplantation in adults with acute myeloid leukemia and myelodysplastic syndromes. Bone Marrow Transpl. 2005;35:965–70. https://doi.org/10.1038/sj.bmt.1704938.
Thol F, Gabdoulline R, Liebich A, Klement P, Schiller J, Kandziora C, et al. Measurable residual disease monitoring by NGS before allogeneic hematopoietic cell transplantation in AML. Blood. 2018;132:1703–13. https://doi.org/10.1182/blood-2018-02-829911. e-pub ahead of print 2018/09/08.
Jentzsch M, Grimm J, Bill M, Brauer D, Backhaus D, Schulz J, et al. Prognostic relevance of remission and measurable residual disease status in AML patients prior to reduced intensity or non-myeloablative allogeneic stem cell transplantation. Blood Cancer J. 2021;11:80 https://doi.org/10.1038/s41408-021-00471-x.
Lachowiez CA, Atluri H, DiNardo CD. Advancing the standard: venetoclax combined with intensive induction and consolidation therapy for acute myeloid leukemia. Ther Adv Hematol. 2022;13:20406207221093964 https://doi.org/10.1177/20406207221093964.
Stelljes M, Middeke JM, Bug G, Wagner E-M, Mueller LP, Christoph S, et al. In patients with relapsed/refractory AML sequential conditioning and immediate allogeneic stem cell transplantation (allo-HCT) results in similar overall and leukemia-free survival compared to intensive remission induction chemotherapy followed by Allo-HCT: results from the randomized phase III ASAP trial. Blood. 2022;140:9–11. https://doi.org/10.1182/blood-2022-159962.
Bazarbachi A, Bug G, Baron F, Brissot E, Ciceri F, Dalle IA, et al. Clinical practice recommendation on hematopoietic stem cell transplantation for acute myeloid leukemia patients with FLT3-internal tandem duplication: a position statement from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2020;105:1507–16. https://doi.org/10.3324/haematol.2019.243410.
Bazarbachi A, Labopin M, Battipaglia G, Djabali A, Passweg J, Socié G, et al. Sorafenib improves survival of FLT3-mutated acute myeloid leukemia in relapse after allogeneic stem cell transplantation: a report of the EBMT Acute Leukemia Working Party. Haematologica. 2019;104:e398–e401. https://doi.org/10.3324/haematol.2018.211615.
Abou Dalle I, El Cheikh J, Bazarbachi A. Pharmacologic strategies for post-transplant maintenance in acute myeloid leukemia: it is time to consider! Cancers. 2022; 14. https://doi.org/10.3390/cancers14061490.
Acknowledgements
We acknowledge all participating EBMT centers as well as the patients and their respective treating physicians that made this database accessible for research.
Author information
Authors and Affiliations
Contributions
IA and AB wrote the manuscript with input from the coauthors. ML performed the statistical analysis. IA, MM, and AB conceived and designed the study. MM and AB directed and edited the manuscript. All authors participated in the discussion, intellectual content, and have reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abou Dalle, I., Labopin, M., Kröger, N. et al. Impact of disease burden on clinical outcomes of AML patients receiving allogeneic hematopoietic cell transplantation: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Bone Marrow Transplant 58, 784–790 (2023). https://doi.org/10.1038/s41409-023-01961-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-01961-1