Abstract
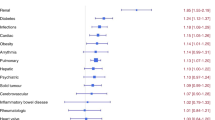
Patients undergoing allogeneic hematopoietic stem cell transplantation (allo-hsct) can require intensive care unit (ICU) admission in the post-transplant period. Whereas outcomes of ICU admission are poor, little is known about the pre-transplant risk factors leading to them. We conducted a retrospective analysis to investigate the impact of pre-transplant individual comorbidities on acute inpatient complications, focusing on ICU admission, ventilator support and multi-system organ failure, following allo-hsct. During the initial hospitalization, 33 (11%) patients required ICU admission, 29 (10%) required ventilator support and 33 (11%) developed multi-system organ failure. Risk factors for ICU admission and ventilator support included pre-transplant infection, pre-transplant diabetes, time to neutrophil engraftment, donor type and older transplant decade (2008-2010). Risk factors for multi-system organ failure included pre-transplant diabetes, time to neutrophil engraftment and older transplant decade (2008–2010). For ICU patients, the 60-day and 6-month mortality was 58% and 67%, respectively and the median overall survival was 1.4 months. Patients with diabetes and infection at the time of HSCT and longer time to neutrophil engraftment during transplant are at an increased risk for ICU admission, ventilator support and multi-system organ failure. Patients admitted to the ICU are also at a high risk for mortality leading to poor survival.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Jamy O, Chen A, Battles K, Francisco L, Salzman D, Bal S, et al. Impact of access to care on 1-year mortality following allogeneic blood or marrow transplantation. Bone Marrow Transpl. 2021;56:1364–72. https://doi.org/10.1038/s41409-020-01184-8.
Majhail NS, Chitphakdithai P, Logan B, King R, Devine S, Rossmann SN, et al. Significant improvement in survival after unrelated donor hematopoietic cell transplantation in the recent era. Biol Blood Marrow Transpl. 2015;21:142–50. https://doi.org/10.1016/j.bbmt.2014.10.001.
Depuydt P, Kerre T, Noens L, Nollet J, Offner F, Decruyenaere J, et al. Outcome in critically ill patients with allogeneic BM or peripheral haematopoietic SCT: a single-centre experience. Bone Marrow Transpl. 2011;46:1186–91. https://doi.org/10.1038/bmt.2010.255.
Garcia Borrega J, Heger JM, Koehler P, Holtick U, Hallek M, Scheid C, et al. Allogeneic stem cell transplant recipients admitted to the intensive care unit during the peri-transplant period have unfavorable outcomes-results of a retrospective analysis from a German university hospital. Ann Hematol. 2022;101:389–95. https://doi.org/10.1007/s00277-021-04698-3.
Saillard C, Blaise D, Mokart D. Critically ill allogeneic hematopoietic stem cell transplantation patients in the intensive care unit: reappraisal of actual prognosis. Bone Marrow Transpl. 2016;51:1050–61. https://doi.org/10.1038/bmt.2016.72.
Benz R, Schanz U, Maggiorini M, Seebach JD, Stussi G. Risk factors for ICU admission and ICU survival after allogeneic hematopoietic SCT. Bone Marrow Transpl. 2014;49:62–65. https://doi.org/10.1038/bmt.2013.141.
Scales DC, Thiruchelvam D, Kiss A, Sibbald WJ, Redelmeier DA. Intensive care outcomes in bone marrow transplant recipients: a population-based cohort analysis. Crit Care. 2008;12:R77. https://doi.org/10.1186/cc6923.
Townsend WM, Holroyd A, Pearce R, Mackinnon S, Naik P, Goldstone AH, et al. Improved intensive care unit survival for critically ill allogeneic haematopoietic stem cell transplant recipients following reduced intensity conditioning. Br J Haematol. 2013;161:578–86. https://doi.org/10.1111/bjh.12294.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9. https://doi.org/10.1182/blood-2005-05-2004.
Fein JA, Shimoni A, Labopin M, Shem-Tov N, Yerushalmi R, Magen H, et al. The impact of individual comorbidities on non-relapse mortality following allogeneic hematopoietic stem cell transplantation. Leukemia. 2018;32:1787–94. https://doi.org/10.1038/s41375-018-0185-y.
Khalil MMI, Lipton JH, Atenafu EG, Gupta V, Kim DD, Kuruvilla J, et al. Impact of comorbidities constituting the hematopoietic cell transplant (HCT)-comorbidity index on the outcome of patients undergoing allogeneic HCT for acute myeloid leukemia. Eur J Haematol. 2018;100:198–205. https://doi.org/10.1111/ejh.13000.
Takano K, Fuji S, Uchida N, Ogawa H, Ohashi K, Eto T, et al. Pre-transplant diabetes mellitus is a risk factor for non-relapse mortality, especially infection-related mortality, after allogeneic hematopoietic SCT. Bone Marrow Transpl. 2015;50:553–8. https://doi.org/10.1038/bmt.2014.315.
National Death Index. Vol. 2018. https://www.cdc.gov/nchs/ndi/index.htm.
Accurint databases. Vol. 2018. http://www.accurint.com.
Lueck C, Stadler M, Koenecke C, Hoeper MM, Dammann E, Schneider A, et al. Improved short- and long-term outcome of allogeneic stem cell recipients admitted to the intensive care unit: a retrospective longitudinal analysis of 942 patients. Intensive Care Med. 2018;44:1483–92. https://doi.org/10.1007/s00134-018-5347-x.
Lengliné E, Chevret S, Moreau AS, Pène F, Blot F, Bourhis JH, et al. Changes in intensive care for allogeneic hematopoietic stem cell transplant recipients. Bone Marrow Transpl. 2015;50:840–5. https://doi.org/10.1038/bmt.2015.55.
Naeem N, Eyzaguirre A, Kern JA, Lazarus HM, Hejal RB, Laughlin MJ, et al. Outcome of adult umbilical cord blood transplant patients admitted to a medical intensive care unit. Bone Marrow Transpl. 2006;38:733–8. https://doi.org/10.1038/sj.bmt.1705502.
Kew AK, Couban S, Patrick W, Thompson K, White D. Outcome of hematopoietic stem cell transplant recipients admitted to the intensive care unit. Biol Blood Marrow Transpl. 2006;12:301–5. https://doi.org/10.1016/j.bbmt.2005.10.020.
Bayraktar UD, Shpall EJ, Liu P, Ciurea SO, Rondon G, de Lima M, et al. Hematopoietic cell transplantation-specific comorbidity index predicts inpatient mortality and survival in patients who received allogeneic transplantation admitted to the intensive care unit. J Clin Oncol. 2013;31:4207–14. https://doi.org/10.1200/jco.2013.50.5867.
Fuji S, Kim SW, Mori S, Fukuda T, Kamiya S, Yamasaki S, et al. Hyperglycemia during the neutropenic period is associated with a poor outcome in patients undergoing myeloablative allogeneic hematopoietic stem cell transplantation. Transplantation. 2007;84:814–20. https://doi.org/10.1097/01.tp.0000296482.50994.1c.
Hammer MJ, Casper C, Gooley TA, O’Donnell PV, Boeckh M, Hirsch IB. The contribution of malglycemia to mortality among allogeneic hematopoietic cell transplant recipients. Biol Blood Marrow Transpl. 2009;15:344–51. https://doi.org/10.1016/j.bbmt.2008.12.488.
Orlandi A, Chavakis E, Seeger F, Tjwa M, Zeiher AM, Dimmeler S. Long-term diabetes impairs repopulation of hematopoietic progenitor cells and dysregulates the cytokine expression in the bone marrow microenvironment in mice. Basic Res Cardiol. 2010;105:703–12. https://doi.org/10.1007/s00395-010-0109-0.
Peck AJ, Corey L, Boeckh M. Pretransplantation respiratory syncytial virus infection: impact of a strategy to delay transplantation. Clin Infect Dis. 2004;39:673–80. https://doi.org/10.1086/422994.
Forcina A, Lorentino F, Marasco V, Oltolini C, Marcatti M, Greco R, et al. Clinical impact of pretransplant multidrug-resistant gram-negative colonization in autologous and allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transpl. 2018;24:1476–82. https://doi.org/10.1016/j.bbmt.2018.02.021.
Barral S, Mamin A, Dantin C, Masouridi-Levrat S, Chalandon Y, Kaiser L, et al. Rhinovirus infections among hematopoietic stem cell transplant recipients: a pre-transplant dilemma? Viruses. 2022;14:267.
Chi AK, Soubani AO, White AC, Miller KB. An update on pulmonary complications of hematopoietic stem cell transplantation. Chest. 2013;144:1913–22. https://doi.org/10.1378/chest.12-1708.
Author information
Authors and Affiliations
Contributions
OJ, RB, and SB contributed towards the conception of the presented study. OJ and AC contributed towards data collection. OJ, AC and SB contributed towards data analysis. OJ, JD, AC, DS, RB and SB contributed towards drafting, revising and approving the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jamy, O., Dasher, J., Chen, A. et al. Impact of pre-transplant individual comorbidities on risk of ICU admission and survival outcomes following allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 58, 311–316 (2023). https://doi.org/10.1038/s41409-022-01897-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01897-y