Abstract
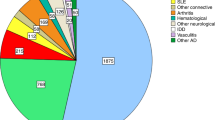
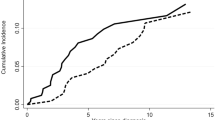
VEXAS (acronym for Vacuoles, E1 enzyme, X-linked, Autoinflammatory, Somatic) is a fascinating new entity encompassing a variety of clinical manifestations, spanning from auto-inflammatory symptoms to hematologic disorders, including myelodysplastic syndromes and plasma cell dyscrasias. Genetically defined by somatic mutations of the X-linked gene UBA1 in hematopoietic stem and progenitor cells, VEXAS typically manifests in males during the fifth/sixth decade of life. Since its discovery, several groups have documented pleomorphic clinical phenotypes, in addition to a plethora of therapeutic options (e.g., JAK inhibitors, hypomethylating agents, and allogeneic stem cell transplant, allo-HCT) in retrospective case series. However, no treatment guidelines have been validated to date, VEXAS patients are typically steroid-dependent and may manifest life-threatening inflammatory symptoms refractory to multiple lines of therapy. To date, the only curative option appears to be allo-HCT in suitable individuals. Nonetheless, this procedure carries an inherent risk of morbidity and mortality that must be judiciously evaluated against a phenotypically diverse disorder where the optimal therapeutic algorithm remains ill-defined. Herein, we provide an overview of the current VEXAS data/ therapeutic evidence and discuss the curative potential of allo-HCT whilst highlighting the efforts required for generation of robust data able to inform therapeutic decisions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Hasserjian RP. This Year’s Best in Hematology Diagnosis: A New Disease Is Discovered. The Hematologist. 2022;19.
Beck DB, Ferrada MA, Sikora KA, Ombrello AK, Collins JC, Pei W, et al. Somatic mutations in UBA1 and severe adult-onset autoinflammatory disease. N. Engl J Med. 2020;383:2628–38.
Oganesyan A, Jachiet V, Chasset F, Hirsch P, Hage-Sleiman M, Fabiani B, et al. VEXAS syndrome: Still expanding the clinical phenotype. Rheumatol (Oxf, Engl). 2021;60:e321–e3.
Oganesyan A, Hakobyan Y, Terrier B, Georgin-Lavialle S, Mekinian A. Looking beyond VEXAS: Coexistence of undifferentiated systemic autoinflammatory disease and myelodysplastic syndrome. Semin Hematol. 2021;58:247–53.
Gurnari C, Pagliuca S, Durkin L, Terkawi L, Awada H, Kongkiatkamon S, et al. Vacuolization of hematopoietic precursors: an enigma with multiple etiologies. Blood 2021;137:3685–9.
Gurnari C, Rogers HJ. Copper Deficiency. N. Engl J Med. 2021;385:640.
Lacombe V, Prevost M, Bouvier A, Thépot S, Chabrun F, Kosmider O, et al. Vacuoles in neutrophil precursors in VEXAS syndrome: diagnostic performances and threshold. Br J Haematol. 2021;195:286–9.
Poulter JA, Collins JC, Cargo C, De Tute RM, Evans P, Ospina Cardona D, et al. Novel somatic mutations in UBA1 as a cause of VEXAS syndrome. Blood 2021;137:3676–81.
Poulter JA, Savic S. Genetics of somatic auto-inflammatory disorders. Semin Hematol. 2021;58:212–7.
Templé M, Duroyon E, Croizier C, Rossignol J, Huet T, Friedrich C, et al. Atypical splice-site mutations causing VEXAS syndrome. Rheumatol (Oxf, Engl). 2021;60:e435–e7.
Dunford A, Weinstock DM, Savova V, Schumacher SE, Cleary JP, Yoda A, et al. Tumor-suppressor genes that escape from X-inactivation contribute to cancer sex bias. Nat Genet. 2017;49:10–6.
Stubbins RJ, McGinnis E, Johal B, Chen LY, Wilson L, Cardona DO, et al. VEXAS syndrome in a female patient with constitutional 45,X (Turner syndrome). Haematologica 2022;107:1011–3.
Arlet JB, Terrier B, Kosmider O. Mutant UBA1 and Severe Adult-Onset Autoinflammatory Disease. N. Engl J Med. 2021;384:2163.
Tsuchida N, Kunishita Y, Uchiyama Y, Kirino Y, Enaka M, Yamaguchi Y, et al. Pathogenic UBA1 variants associated with VEXAS syndrome in Japanese patients with relapsing polychondritis. Ann Rheum Dis. 2021;80:1057–61.
Barba T, Jamilloux Y, Durel CA, Bourbon E, Mestrallet F, Sujobert P, et al. VEXAS syndrome in a woman. Rheumatol (Oxf, Engl). 2021;60:e402–e3.
Gurnari C, Panetta P, Fabiani E, Nardone AM, Postorivo D, Falconi G, et al. Identification of i(X)(p10) as the sole molecular abnormality in atypical chronic myeloid leukemia evolved into acute myeloid leukemia. Mol Clin Oncol. 2018;8:463–5.
Zakine E, Schell B, Battistella M, Vignon-Pennamen MD, Chasset F, Mahévas T, et al. UBA1 Variations in Neutrophilic Dermatosis Skin Lesions of Patients With VEXAS Syndrome. JAMA Dermatol. 2021;157:1349–54.
Lacombe V, Beucher A, Urbanski G, Le Corre Y, Cottin L, Croué A, et al. Distinction between clonal and paraclonal cutaneous involvements in VEXAS syndrome. Exp Hematol Oncol. 2022;11:6.
Ferrada MA, Savic S, Ospina Cardona D, Collins JC, Alessi H, Gutierrez-Rodrigues F, et al. Translation of cytoplasmic UBA1 contributes to VEXAS syndrome pathogenesis. Blood. 2022:blood.2022016985. https://doi.org/10.1182/blood.2022016985. Online ahead of print.
Obiorah IE, Patel BA, Groarke EM, Wang W, Trick M, Ombrello AK, et al. Benign and malignant hematologic manifestations in patients with VEXAS syndrome due to somatic mutations in UBA1. Blood Adv. 2021;5:3203–15.
Pfeilstöcker M, Tuechler H, Sanz G, Schanz J, Garcia-Manero G, Solé F, et al. Time-dependent changes in mortality and transformation risk in MDS. Blood 2016;128:902–10.
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 2016;127:2391–405.
Kusne Y, Fernandez J, Patnaik MM. Clonal hematopoiesis and VEXAS syndrome: survival of the fittest clones? Semin Hematol. 2021;58:226–9.
Shaukat F, Hart M, Burns T, Bansal P. UBA1 and DNMT3A mutations in VEXAS syndrome. A case report and literature review. Mod Rheumatol case Rep. 2022;6:134–9.
Georgin-Lavialle S, Terrier B, Guedon AF, Heiblig M, Comont T, Lazaro E, et al. Further characterization of clinical and laboratory features in VEXAS syndrome: large-scale analysis of a multicentre case series of 116 French patients. Br J Dermatol. 2022;186:564–74.
van der Made CI, Potjewijd J, Hoogstins A, Willems HPJ, Kwakernaak AJ, de Sevaux RGL, et al. Adult-onset autoinflammation caused by somatic mutations in UBA1: A Dutch case series of patients with VEXAS. J Allergy Clin Immunol. 2022;149:432–9. e4
Groarke EM, Dulau-Florea AE, Kanthi Y. Thrombotic manifestations of VEXAS syndrome. Semin Hematol. 2021;58:230–8.
Emmi G, Silvestri E, Squatrito D, Amedei A, Niccolai E, D’Elios MM, et al. Thrombosis in vasculitis: from pathogenesis to treatment. Thrombosis J. 2015;13:15.
Oo TM, Koay JTJ, Lee SF, Lee SMS, Lim XR, Fan BE. Thrombosis in VEXAS syndrome. J Thrombosis Thrombolysis. 2022;53:965–70.
Heiblig M, Patel BA, Groarke EM, Bourbon E, Sujobert P. Toward a pathophysiology inspired treatment of VEXAS syndrome. Semin Hematol. 2021;58:239–46.
Bourbon E, Heiblig M, Gerfaud Valentin M, Barba T, Durel C-A, Lega JC, et al. Therapeutic options in VEXAS syndrome: insights from a retrospective series. Blood 2021;137:3682–4.
Raaijmakers M, Hermans M, Aalbers A, Rijken M, Dalm V, van Daele P, et al. Azacytidine Treatment for VEXAS Syndrome. HemaSphere. 2021;5:e661.
Comont T, Heiblig M, Rivière E, Terriou L, Rossignol J, Bouscary D, et al. Azacitidine for patients with Vacuoles, E1 Enzyme, X-linked, Autoinflammatory, Somatic syndrome (VEXAS) and myelodysplastic syndrome: data from the French VEXAS registry. Br J Haematol. 2022;196:969–74.
Mekinian A, Grignano E, Braun T, Decaux O, Liozon E, Costedoat-Chalumeau N, et al. Systemic inflammatory and autoimmune manifestations associated with myelodysplastic syndromes and chronic myelomonocytic leukaemia: a French multicentre retrospective study. Rheumatol (Oxf, Engl). 2016;55:291–300.
Gang AO, Frøsig TM, Brimnes MK, Lyngaa R, Treppendahl MB, Grønbæk K, et al. 5-Azacytidine treatment sensitizes tumor cells to T-cell mediated cytotoxicity and modulates NK cells in patients with myeloid malignancies. Blood cancer J. 2014;4:e197.
Landman S, Cruijsen M, Urbano PCM, Huls G, van Erp PEJ, van Rijssen E, et al. DNA Methyltransferase Inhibition Promotes Th1 Polarization in Human CD4(+)CD25(high) FOXP3(+) Regulatory T Cells but does not affect their suppressive capacity. J Immunol Res. 2018;2018:4973964.
Stübig T, Badbaran A, Luetkens T, Hildebrandt Y, Atanackovic D, Binder TM, et al. 5-azacytidine promotes an inhibitory T-cell phenotype and impairs immune mediated antileukemic activity. Mediators Inflamm. 2014;2014:418292.
Frikeche J, Clavert A, Delaunay J, Brissot E, Grégoire M, Gaugler B, et al. Impact of the hypomethylating agent 5-azacytidine on dendritic cells function. Exp Hematol. 2011;39:1056–63.
McLornan DP, Pope JE, Gotlib J, Harrison CN. Current and future status of JAK inhibitors. Lancet (Lond, Engl). 2021;398:803–16.
McLornan DP, Khan AA, Harrison CN. Immunological Consequences of JAK Inhibition: Friend or Foe? Curr hematologic Malignancy Rep. 2015;10:370–9.
Heiblig M, Ferrada MA, Koster MJ, Barba T, Gerfaud-Valentin M, Mékinian A, et al. Ruxolitinib is more effective than other JAK Inhibitors to treat VEXAS Syndrome: A retrospective multi center study. Blood. 2022:blood.2022016642. https://doi.org/10.1182/blood.2022016642. Online ahead of print.
Islam S, Cullen T, Sumpton D, Damodaran A, Heath D, Bosco A, et al. VEXAS syndrome: lessons learnt from an early Australian case series. Intern Med J. 2022;52:658–62.
Staels F, Betrains A, Woei AJF, Boeckx N, Beckers M, Bervoets A, et al. Case Report: VEXAS Syndrome: From Mild Symptoms to Life-Threatening Macrophage Activation Syndrome. Front Immunol. 2021;12:678927.
Goyal A, Narayanan D, Wong W, Laga AC, Connell NT, Ritter SY, et al. Tocilizumab for treatment of cutaneous and systemic manifestations of vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic (VEXAS) syndrome without myelodysplastic syndrome. JAAD case Rep. 2022;23:15–9.
Kirino Y, Takase-Minegishi K, Tsuchida N, Hirahara L, Kunishita Y, Yoshimi R, et al. Tocilizumab in VEXAS relapsing polychondritis: a single-center pilot study in Japan. Ann Rheum Dis. 2021;80:1501–2.
Vila AT, Puig L, Fernández-Figueras MT, Laiz AM, Vidal D, Alomar A. Adverse cutaneous reactions to anakinra in patients with rheumatoid arthritis: clinicopathological study of five patients. Br J Dermatol. 2005;153:417–23.
Kaiser C, Knight A, Nordström D, Pettersson T, Fransson J, Florin-Robertsson E, et al. Injection-site reactions upon Kineret (anakinra) administration: experiences and explanations. Rheumatol Int. 2012;32:295–9.
Diarra A, Duployez N, Fournier E, Preudhomme C, Coiteux V, Magro L, et al. Successful allogeneic hematopoietic stem cell transplantation in patients with VEXAS syndrome: a two center experience. Blood Adv. 2022;6:998–1003.
Diarra A, Duployez N, Terriou L. Mutant UBA1 and severe adult-onset autoinflammatory disease. N. Engl J Med. 2021;384:2163–4.
Loschi M, Roux C, Sudaka I, Ferrero-Vacher C, Marceau-Renaut A, Duployez N, et al. Allogeneic stem cell transplantation as a curative therapeutic approach for VEXAS syndrome: a case report. Bone marrow Transplant. 2022;57:315–8.
Elsawy M, Sorror ML. Up-to-date tools for risk assessment before allogeneic hematopoietic cell transplantation. Bone marrow Transplant. 2016;51:1283–300.
Alexander T, Greco R. Hematopoietic stem cell transplantation and cellular therapies for autoimmune diseases: overview and future considerations from the Autoimmune Diseases Working Party (ADWP) of the European Society for Blood and Marrow Transplantation (EBMT). Bone Marrow Transplant. 2022;57:1055–62.
Snowden JA, Sánchez-Ortega I, Corbacioglu S, Basak GW, Chabannon C, de la Camara R, et al. Indications for haematopoietic cell transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe, 2022. Bone Marrow Transplant. 2022:57:1217–39.
Poulter J, Gough A, Isaacs JD, Green M, McHugh N, Hordon L, et al. A High-Throughput Amplicon Screen for Somatic UBA1 Variants in Cytopenic and Giant Cell Arteritis Cohorts. J Clin Immunol. 2022. https://doi.org/10.1007/s10875-022-01258-w. Online ahead of print.
Voso MT, Gurnari C. Have we reached a molecular era in myelodysplastic syndromes? Hematol Am Soc Hematol Educ Program. 2021;2021:418–27.
Acknowledgements
This work was supported by a grant from the Edward P. Evans Foundation (to CG). The Authors thank Dr. Heesun J. Rogers for providing histopathology pictures.
Author information
Authors and Affiliations
Contributions
CG and DPM conceived the idea and wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gurnari, C., McLornan, D.P. Update on VEXAS and role of allogeneic bone marrow transplant: Considerations on behalf of the Chronic Malignancies Working Party of the EBMT. Bone Marrow Transplant 57, 1642–1648 (2022). https://doi.org/10.1038/s41409-022-01774-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01774-8
This article is cited by
-
VEXAS syndrome: complete molecular remission after hypomethylating therapy
Annals of Hematology (2024)
-
Clinical characteristics, disease trajectories and management of vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic (VEXAS) syndrome: a systematic review
Rheumatology International (2023)
-
How I Manage Transplant Ineligible Patients with Myelodysplastic Neoplasms
Clinical Hematology International (2022)