Abstract
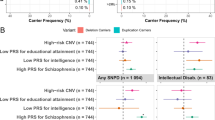
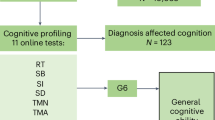
Cognitive impairment is prevalent in blood or marrow transplantation (BMT) recipients, albeit with inter-individual variability. We conducted a genome-wide association study of objective cognitive function assessed longitudinally in 239 adult BMT recipients for discovery and replicated in an independent cohort of 540 BMT survivors. Weighted genome-wide polygenic risk scores (PRS) were constructed using linkage disequilibrium pruned significant SNPs. Forty-four genome-wide significant SNPs were identified using additive (n = 3); codominant (n = 20) and genotype models (n = 21). Each additional copy of a risk allele was associated with a 0.28-point (p = 1.07 × 10−8) to a 1.82-point (p = 6.7 × 10−12) increase in a global deficit score. We replicated two SNPs (rs11634183 and rs12486041) with links to neural integrity. Patients in the top PRS quintile were at increased risk of cognitive impairment in discovery (RR = 1.95, 95%CI: 1.28–2.96, p = 0.002) and replication cohorts (OR = 1.84, 95%CI, 1.02–3.32, p = 0.043). Associations were stronger among individuals with lowest clinical risk for cognitive impairment. These findings support potential utility of PRS-based risk classification in the development of targeted interventions aimed at improving cognitive outcomes in BMT survivors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data underlying this article cannot be shared publicly for the privacy of individuals that participated in the study. The data will be shared on reasonable request to the corresponding authors.
References
Sharafeldin N, Bosworth A, Patel SK, Chen Y, Morse E, Mather M, et al. Cognitive functioning after hematopoietic cell transplantation for hematologic malignancy: results from a prospective longitudinal study. J Clin Oncol. 2018;36:463–75.
Syrjala KL, Artherholt SB, Kurland BF, Langer SL, Roth-Roemer S, Elrod JB, et al. Prospective neurocognitive function over 5 years after allogeneic hematopoietic cell transplantation for cancer survivors compared with matched controls at 5 years. J Clin Oncol. 2011;29:2397–404.
Syrjala KL, Langer SL, Abrams JR, Storer B, Sanders JE, Flowers ME, et al. Recovery and long-term function after hematopoietic cell transplantation for leukemia or lymphoma. JAMA 2004;291:2335–43.
Booth-Jones M, Jacobsen PB, Ransom S, Soety E. Characteristics and correlates of cognitive functioning following bone marrow transplantation. Bone Marrow Transpl. 2005;36:695–702.
Harris SE, Deary IJ. The genetics of cognitive ability and cognitive ageing in healthy older people. Trends Cogn Sci. 2011;15:388–94.
Jonsson T, Stefansson H, Steinberg S, Jonsdottir I, Jonsson PV, Snaedal J, et al. Variant of TREM2 associated with the risk of Alzheimer’s disease. N. Engl J Med. 2013;368:107–16.
Lacour A, Espinosa A, Louwersheimer E, Heilmann S, Hernandez I, Wolfsgruber S, et al. Genome-wide significant risk factors for Alzheimer’s disease: role in progression to dementia due to Alzheimer’s disease among subjects with mild cognitive impairment. Mol Psychiatry. 2017;22:153–60.
Seshadri S, Fitzpatrick AL, Ikram MA, DeStefano AL, Gudnason V, Boada M, et al. Genome-wide analysis of genetic loci associated with Alzheimer disease. JAMA 2010;303:1832–40.
Strittmatter WJ, Saunders AM, Schmechel D, Pericak-Vance M, Enghild J, Salvesen GS, et al. Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proc Natl Acad Sci USA. 1993;90:1977–81.
Ahles TA, Saykin AJ, Noll WW, Furstenberg CT, Guerin S, Cole B, et al. The relationship of APOE genotype to neuropsychological performance in long-term cancer survivors treated with standard dose chemotherapy. Psychooncology. 2003;12:612–9.
Small BJ, Rawson KS, Walsh E, Jim HS, Hughes TF, Iser L, et al. Catechol-O-methyltransferase genotype modulates cancer treatment-related cognitive deficits in breast cancer survivors. Cancer 2011;117:1369–76.
Koleck TA, Bender CM, Sereika SM, Brufsky AM, Lembersky BC, McAuliffe PF, et al. Polymorphisms in DNA repair and oxidative stress genes associated with pre-treatment cognitive function in breast cancer survivors: an exploratory study. Springerplus 2016;5:422.
Sharafeldin N, Richman J, Bosworth A, Chen Y, Singh P, Patel SK, et al. Clinical and genetic risk prediction of cognitive impairment after blood or marrow transplantation for hematologic malignancy. J Clin Oncol. 2020;38:1312–21.
Fan J, Tao W, Li X, Li H, Zhang J, Wei D, et al. The Contribution of genetic factors to cognitive impairment and dementia: apolipoprotein e gene, gene interactions, and polygenic risk. Int J Mol Sci. 2019;20:1177.
Khera AV, Chaffin M, Aragam KG, Haas ME, Roselli C, Choi SH, et al. Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nat Genet. 2018;50:1219–24.
Yanes T, McInerney-Leo AM, Law M, Cummings S, The emerging field of polygenic risk scores and perspective for use in clinical care. Hum Mol Genet. 2020;29:R165–R76.
Choi SW, O’Reilly PF PRSice-2: Polygenic Risk Score software for biobank-scale data. Gigascience. 2019;8.
Euesden J, Lewis CM, O’Reilly PF. PRSice: Polygenic Risk Score software. Bioinformatics 2015;31:1466–8.
Inouye M, Abraham G, Nelson CP, Wood AM, Sweeting MJ, Dudbridge F, et al. Genomic risk prediction of coronary artery disease in 480,000 adults: implications for primary prevention. J Am Coll Cardiol. 2018;72:1883–93.
Torkamani A, Wineinger NE, Topol EJ. The personal and clinical utility of polygenic risk scores. Nat Rev Genet. 2018;19:581–90.
Blackstone K, Moore DJ, Franklin DR, Clifford DB, Collier AC, Marra CM, et al. Defining neurocognitive impairment in HIV: deficit scores versus clinical ratings. Clin Neuropsychol. 2012;26:894–908.
Carey CL, Woods SP, Gonzalez R, Conover E, Marcotte TD, Grant I, et al. Predictive validity of global deficit scores in detecting neuropsychological impairment in HIV infection. J Clin Exp Neuropsychol. 2004;26:307–19.
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81:559–75.
Baker KS, Gurney JG, Ness KK, Bhatia R, Forman SJ, Francisco L, et al. Late effects in survivors of chronic myeloid leukemia treated with hematopoietic cell transplantation: results from the Bone Marrow Transplant Survivor Study. Blood 2004;104:1898–906.
Manduchi E, Orzechowski PR, Ritchie MD, Moore JH. Exploration of a diversity of computational and statistical measures of association for genome-wide genetic studies. BioData Min. 2019;12:14.
Tsepilov YA, Shin SY, Soranzo N, Spector TD, Prehn C, Adamski J, et al. Nonadditive effects of genes in human metabolomics. Genetics 2015;200:707–18.
Park JH, Gail MH, Weinberg CR, Carroll RJ, Chung CC, Wang Z, et al. Distribution of allele frequencies and effect sizes and their interrelationships for common genetic susceptibility variants. Proc Natl Acad Sci USA. 2011;108:18026–31.
Kozomara A, Birgaoanu M, Griffiths-Jones S. miRBase: from microRNA sequences to function. Nucleic Acids Res. 2019;47:D155–D62.
Griffiths-Jones S, Saini HK, van Dongen S, Enright AJ. miRBase: tools for microRNA genomics. Nucleic Acids Res 2008;36:D154–8.
Griffiths-Jones S. The microRNA Registry. Nucleic Acids Res 2004;32:D109–11.
Consortium EP. An integrated encyclopedia of DNA elements in the human genome. Nature 2012;489:57–74.
Davis CA, Hitz BC, Sloan CA, Chan ET, Davidson JM, Gabdank I, et al. The Encyclopedia of DNA elements (ENCODE): data portal update. Nucleic Acids Res. 2018;46:D794–D801.
Sethupathy P, Collins FS. MicroRNA target site polymorphisms and human disease. Trends Genet. 2008;24:489–97.
Macfarlane LA, Murphy PR. MicroRNA: biogenesis, function and role in cancer. Curr Genomics. 2010;11:537–61.
Rouillard AD, Gundersen GW, Fernandez NF, Wang Z, Monteiro CD, McDermott MG, et al. The harmonizome: a collection of processed datasets gathered to serve and mine knowledge about genes and proteins. Database. 2016;2016:1–16.
Welter D, MacArthur J, Morales J, Burdett T, Hall P, Junkins H, et al. The NHGRI GWAS Catalog, a curated resource of SNP-trait associations. Nucleic Acids Res. 2014;42:D1001–6.
Kumar S, Vijayan M, Reddy PH. MicroRNA-455-3p as a potential peripheral biomarker for Alzheimer’s disease. Hum Mol Genet. 2017;26:3808–22.
Martinez B, Peplow PV. MicroRNAs as biomarkers of diabetic retinopathy and disease progression. Neural Regen Res. 2019;14:1858–69.
Walter S, Atzmon G, Demerath EW, Garcia ME, Kaplan RC, Kumari M, et al. A genome-wide association study of aging. Neurobiol Aging. 2011;32:2109 e15–28.
Zhao L, Spassieva S, Gable K, Gupta SD, Shi LY, Wang J, et al. Elevation of 20-carbon long chain bases due to a mutation in serine palmitoyltransferase small subunit b results in neurodegeneration. Proc Natl Acad Sci USA. 2015;112:12962–7.
Chen Y, Cao B, Ou R, Wei Q, Chen X, Zhao B, et al. Determining the effect of the HNMT, STK39, and NMD3 polymorphisms on the Incidence of Parkinson’s disease, amyotrophic lateral sclerosis, and multiple system atrophy in Chinese populations. J Mol Neurosci. 2018;64:574–80.
Kamburov A, Stelzl U, Lehrach H, Herwig R. The ConsensusPathDB interaction database: 2013 update. Nucleic Acids Res 2013;41:D793–800.
Hu W, Wang Z, Zheng H. Mitochondrial accumulation of amyloid beta (Abeta) peptides requires TOMM22 as a main Abeta receptor in yeast. J Biol Chem. 2018;293:12681–9.
Desler C, Lillenes MS, Tonjum T, Rasmussen LJ. The role of mitochondrial dysfunction in the progression of Alzheimer’s disease. Curr Med Chem. 2018;25:5578–87.
Marioni RE, Harris SE, Zhang Q, McRae AF, Hagenaars SP, Hill WD, et al. GWAS on family history of Alzheimer’s disease. Transl Psychiatry. 2018;8:99.
Han Z, Huang H, Gao Y, Huang Q. Functional annotation of Alzheimer’s disease associated loci revealed by GWASs. PLoS One. 2017;12:e0179677.
Huang H, Zhao J, Xu B, Ma X, Dai Q, Li T, et al. The TOMM40 gene rs2075650 polymorphism contributes to Alzheimer’s disease in Caucasian, and Asian populations. Neurosci Lett. 2016;628:142–6.
Goes FS, McGrath J, Avramopoulos D, Wolyniec P, Pirooznia M, Ruczinski I, et al. Genome-wide association study of schizophrenia in Ashkenazi Jews. Am J Med Genet B Neuropsychiatr Genet. 2015;168:649–59.
Ikeda M, Takahashi A, Kamatani Y, Momozawa Y, Saito T, Kondo K, et al. Genome-wide association study detected novel susceptibility genes for schizophrenia and shared trans-populations/diseases genetic effect. Schizophr Bull. 2019;45:824–34.
Esserman LJ, Study W, Athena I. The WISDOM Study: breaking the deadlock in the breast cancer screening debate. NPJ Breast Cancer. 2017;3:34.
Roman M, Sala M, Domingo L, Posso M, Louro J, Castells X. Personalized breast cancer screening strategies: a systematic review and quality assessment. PLoS One. 2019;14:e0226352.
Lee A, Mavaddat N, Wilcox AN, Cunningham AP, Carver T, Hartley S, et al. BOADICEA: a comprehensive breast cancer risk prediction model incorporating genetic and nongenetic risk factors. Genet Med. 2019;21:1708–18.
Licher S, Ahmad S, Karamujic-Comic H, Voortman T, Leening MJG, Ikram MA, et al. Genetic predisposition, modifiable-risk-factor profile and long-term dementia risk in the general population. Nat Med. 2019;25:1364–9.
Khera AV, Emdin CA, Drake I, Natarajan P, Bick AG, Cook NR, et al. Genetic risk, adherence to a healthy lifestyle, and coronary disease. N. Engl J Med. 2016;375:2349–58.
Costa DSJ, Fardell JE. Why are objective and perceived cognitive function weakly correlated in patients with cancer? J Clin Oncol. 2019;37:1154–8.
Louie AD, Robison LL, Bogue M, Hyde S, Forman SJ, Bhatia S. Validation of self-reported complications by bone marrow transplantation survivors. Bone Marrow Transpl. 2000;25:1191–6.
Murdaugh DL, Bosworth A, Patel SK, Sharafeldin N, Chen Y, Francisco L, et al. Self-endorsed cognitive problems versus objectively assessed cognitive impairment in blood or bone marrow transplantation recipients: a longitudinal study. Cancer. 2020;126:2174–82.
Acknowledgements
The authors thank Emily Morse, Molly Mather, and Canlan Sun for their roles in the data collection and patient management of the discovery cohort at City of Hope.
Funding
This work was supported in part by research funding from the Leukemia andLymphoma Society (LLS) (62771-11) to SB and LLS Career Development Award (3386-19) to NS. NS is also supported by the National Marrow Donor Program Be The Match Foundation.
Author information
Authors and Affiliations
Contributions
SB constructed the study cohort and SB, NS, SP, SJF contributed to the study design. AB, LF collected, maintained, and stored the data. NS, YJ, XW, and FLW prepared the data for analysis. PS handled and processed the genetic samples. NS designed and performed the statistical data analysis. NS, JZ, AIO, and SB interpreted the genetic results. NS and SB drafted the manuscript with critical revisions from all authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sharafeldin, N., Zhang, J., Singh, P. et al. Genome-wide variants and polygenic risk scores for cognitive impairment following blood or marrow transplantation. Bone Marrow Transplant 57, 925–933 (2022). https://doi.org/10.1038/s41409-022-01642-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01642-5