Abstract
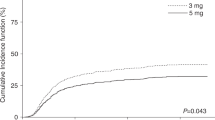
Allogeneic hematopoietic cell transplantation (allo-HCT) is potentially curative for patients with malignant and benign hematologic conditions. Graft-versus-host disease (GVHD) is a known complication of allo-HCT that results in significant morbidity and mortality. A common GVHD prophylaxis strategy combines a calcineurin inhibitor with methotrexate. When mucositis and organ toxicity develop, the day +11 dose is frequently omitted to limit further organ damage. The potential impact of this practice on allo-HCT outcomes is unclear as published data show conflicting results. Thus, we performed a systematic review/meta-analysis of the available literature to assess the impact of omitting day +11 methotrexate on allo-HCT recipients. Data were extracted in relation to benefits (overall survival [OS], progression-free survival [PFS]) and harms (acute and chronic GVHD, non-relapse mortality [NRM], and relapse). Pooled OS rate favored those who received day +11 methotrexate vs. those who did not (HR = 1.21; 95% CI = 1.02–1.43; p = 0.03). There was no significant difference in pooled rates of PFS (HR = 0.96; 95% CI = 0.60–1.52; p = 0.85), acute GVHD (HR = 1.03; 95% CI = 0.35–2.98; p = 0.96), chronic GVHD (HR = 0.83; 95% CI = 0.44–1.57; p = 0.57), NRM (HR = 0.86; 95% CI = 0.67–1.11; p = 0.25), and relapse (HR = 0.97; 95% CI = 0.75–1.26; p = 0.83) between the two groups. Large prospective multicenter studies are needed to better define the significance of day +11 methotrexate omission.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Gooley TA, Chien JW, Pergam SA, Hingorani S, Sorror ML, Boeckh M, et al. Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med. 2010;363:2091–101.
Kharfan-Dabaja MA, Al Malki MM, Deotare U, Raj RV, El-Jurdi N, Majhail N, et al. Haematopoietic cell transplantation for blastic plasmacytoid dendritic cell neoplasm: a North American multicentre collaborative study. Br J Haematol. 2017;179:781–9.
Hsieh MM, Kang EM, Fitzhugh CD, Link MB, Bolan CD, Kurlander R, et al. Allogeneic hematopoietic stem-cell transplantation for sickle cell disease. N Engl J Med. 2009;361:2309–17.
Hamilton BK, Storer BE, Wood WA, Pidala JA, Cutler CS, Martin PJ, et al. Disability related to chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2020;26:772–7.
Storb R, Pepe M, Deeg HJ, Anasetti C, Appelbaum FR, Bensinger W, et al. Long-term follow-up of a controlled trial comparing a combination of methotrexate plus cyclosporine with cyclosporine alone for prophylaxis of graft-versus-host disease in patients administered HLA-identical marrow grafts for leukemia. Blood. 1992;80:560–1.
Ringden O, Horowitz MM, Sondel P, Gale RP, Biggs JC, Champlin RE, et al. Methotrexate, cyclosporine, or both to prevent graft-versus-host disease after HLA-identical sibling bone marrow transplants for early leukemia? Blood. 1993;81:1094–101.
Storb R, Deeg HJ, Whitehead J, Appelbaum F, Beatty P, Bensinger W, et al. Methotrexate and cyclosporine compared with cyclosporine alone for prophylaxis of acute graft versus host disease after marrow transplantation for leukemia. N Engl J Med. 1986;314:729–35.
Inamoto Y, Flowers ME, Appelbaum FR, Carpenter PA, Deeg HJ, Furlong T, et al. A retrospective comparison of tacrolimus versus cyclosporine with methotrexate for immunosuppression after allogeneic hematopoietic cell transplantation with mobilized blood cells. Biol Blood Marrow Transplant. 2011;17:1088–92.
Nash RA, Antin JH, Karanes C, Fay JW, Avalos BR, Yeager AM, et al. Phase 3 study comparing methotrexate and tacrolimus with methotrexate and cyclosporine for prophylaxis of acute graft-versus-host disease after marrow transplantation from unrelated donors. Blood. 2000;96:2062–8.
Yanada M, Emi N, Naoe T, Sakamaki H, Takahashi S, Hirabayashi N, et al. Tacrolimus instead of cyclosporine used for prophylaxis against graft-versus-host disease improves outcome after hematopoietic stem cell transplantation from unrelated donors, but not from HLA-identical sibling donors: a nationwide survey conducted in Japan. Bone Marrow Transplant. 2004;34:331–7.
Cutler C, Logan B, Nakamura R, Johnston L, Choi S, Porter D, et al. Tacrolimus/sirolimus vs tacrolimus/methotrexate as GVHD prophylaxis after matched, related donor allogeneic HCT. Blood. 2014;124:1372–7.
Pidala J, Kim J, Jim H, Kharfan-Dabaja MA, Nishihori T, Fernandez HF, et al. A randomized phase II study to evaluate tacrolimus in combination with sirolimus or methotrexate after allogeneic hematopoietic cell transplantation. Haematologica. 2012;97:1882–9.
Terakura S, Kuwatsuka Y, Sugita J, Takahashi S, Ozawa Y, Ozeki K, et al. Effect of methotrexate dose in graft-versus-host disease prophylaxis after single-unit cord blood transplantation in adult acute myeloid leukemia. Int J Hematol. 2021;113:840–50.
Kharfan-Dabaja M, Mhaskar R, Reljic T, Pidala J, Perkins JB, Djulbegovic B, et al. Mycophenolate mofetil versus methotrexate for prevention of graft-versus-host disease in people receiving allogeneic hematopoietic stem cell transplantation. Cochrane Database Syst Rev. 2014:CD010280.
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14:641–50.
De Jong CN, Meijer E, Bakunina K, Nur E, van Marwijk Kooij M, de Groot MR, et al. Post-transplantation cyclophosphamide after allogeneic hematopoietic stem cell transplantation: results of the prospective randomized HOVON-96 trial in recipients of matched related and unrelated donors. Blood. 2019;134:1.
Bolanos-Meade J, Reshef R, Fraser R, Fei M, Abhyankar S, Al-Kadhimi Z, et al. Three prophylaxis regimens (tacrolimus, mycophenolate mofetil, and cyclophosphamide; tacrolimus, methotrexate, and bortezomib; or tacrolimus, methotrexate, and maraviroc) versus tacrolimus and methotrexate for prevention of graft-versus-host disease with haemopoietic cell transplantation with reduced-intensity conditioning: a randomised phase 2 trial with a non-randomised contemporaneous control group (BMT CTN 1203). Lancet Haematol. 2019;6:e132–43.
Jagasia M, Arora M, Flowers ME, Chao NJ, McCarthy PL, Cutler CS, et al. Risk factors for acute GVHD and survival after hematopoietic cell transplantation. Blood. 2012;119:296–307.
Anasetti C, Logan BR, Lee SJ, Waller EK, Weisdorf DJ, Wingard JR, et al. Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl J Med. 2012;367:1487–96.
Atkinson K, Downs K. Omission of day 11 methotrexate does not appear to influence the incidence of moderate to severe acute graft-versus-host disease, chronic graft-versus-host disease, relapse rate or survival after HLA-identical sibling bone marrow transplantation. Bone Marrow Transplant. 1995;16:755–8.
Kumar S, Wolf RC, Chen MG, Gastineau DA, Gertz MA, Inwards DJ, et al. Omission of day +11 methotrexate after allogeneic bone marrow transplantation is associated with increased risk of severe acute graft-versus-host disease. Bone Marrow Transplant. 2002;30:161–5.
Bensinger W, Stem Cell Trialists’ Collaborative Group Individual patient data meta-analysis of allogeneic peripheral blood stem cell transplant vs bone marrow transplant in the management of hematological malignancies: indirect assessment of the effect of day 11 methotrexate administration. Bone Marrow Transplant. 2006;38:539–46.
Honda A, Kakihana K, Aoki J, Kobayashi T, Doki N, Sakamaki H, et al. Omission of day-11 MTX, in combination with tacrolimus, is not associated with increased risk of acute graft-versus-host disease after allo-BMT. Bone Marrow Transplant. 2013;48:307–9.
Hamilton BK, Rybicki L, Haddad H, Abounader D, Yurch M, Majhail NS, et al. Does day 11 omission of methotrexate due to toxicity influence the outcome in myeloablative hematopoietic cell transplant? Results from a single-center retrospective cohort study. Blood Cancer J. 2015;5:e344.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos W, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2019. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed on July 12, 2021.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Kendall MG, Stuart A, Ord JK. Kendall’s advanced theory of statistics. Oxford University Press, Inc.; 1987. Accessed on July 12, 2021
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
StataCorp. Stata Statistical Software: Release 16. College Station, TX: StataCorp LP; 2016.
Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72:39.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Author information
Authors and Affiliations
Contributions
MAK-D: developed the concept, obtained the data, analyzed the data, interpreted the results, and wrote the manuscript. TR: obtained the data, analyzed the data, interpreted the results, and wrote the manuscript. AK: obtained the data, analyzed the data, and interpreted the results. FY: obtained the data, analyzed the data, interpreted the results, and edited the manuscript. KK: obtained the data, analyzed the data, and interpreted the results. AF: obtained the data, analyzed the data, and interpreted the results. HM: interpreted the results and edited the manuscript. EA: interpreted the results and edited the manuscript. MA: interpreted the results and edited the manuscript. MI: analyzed the data, interpreted the results, and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
MAK-D reports consultancy for Daiichi Sankyo in the past 36 months. All other authors declare no relevant conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kharfan-Dabaja, M.A., Reljic, T., Kumar, A. et al. Omission of day +11 methotrexate dose and allogeneic hematopoietic cell transplantation outcomes: results of a systematic review/meta-analysis. Bone Marrow Transplant 57, 65–71 (2022). https://doi.org/10.1038/s41409-021-01496-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01496-3