Abstract
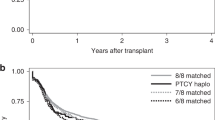
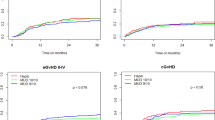
The objective of this study was to compare clinical outcomes between noninherited maternal antigen (NIMA)-mismatched and noninherited paternal antigen (NIPA)-mismatched haploidentical hematopoietic stem cell transplantation (haplo-HSCT) among patients with hematological malignancies and perform a subgroup analysis. We retrospectively analyzed 378 patients with hematological malignancies who received haplo-HSCT from NIMA-mismatched (n = 201) and NIPA-mismatched (n = 177) donors between January 2012 and December 2017. The cumulative incidence of 100-d grades II–IV acute graft-versus-host disease (aGVHD) (19.2% vs. 32.8%, P = 0.003) was significantly lower in NIMA mismatch. Multivariate analysis showed that NIMA mismatch was associated with lower incidence of grades II–IV aGVHD and better overall survival (OS) and disease-free survival (DFS). According to the subgroup analysis, the clinical outcomes of older and/or female NIMA mismatches were comparable to those of younger and/or male NIPA mismatches with respect to grades II–IV aGVHD, chronic GVHD (cGVHD), nonrelapse mortality (NRM), relapse, DFS, and OS. In conclusion, this study confirmed the NIMA effect on aGVHD and demonstrated that NIMA mismatch was associated with better survival. In the NIMA mismatch context, donor age and sex did not seem to influence haplo-HSCT, which provides a basis for the selection of sibling donors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Xu L, Chen H, Chen J, Han M, Huang H, Lai Y, et al. The consensus on indications, conditioning regimen, and donor selection of allogeneic hematopoietic cell transplantation for hematological diseases in China-recommendations from the Chinese Society of Hematology. J Hematol Oncol. 2018;11:33 https://doi.org/10.1186/s13045-018-0564-x.
Apperley J, Niederwieser D, Huang XJ, Nagler A, Fuchs E, Szer J, et al. Haploidentical hematopoietic stem cell transplantation: a global overview comparing Asia, the European Union, and the United States. Biol Blood Marrow Transpl. 2016;22:23–26. https://doi.org/10.1016/j.bbmt.2015.11.001.
Chang YJ, Huang XJ. Haploidentical SCT: the mechanisms underlying the crossing of HLA barriers. Bone Marrow Transpl. 2014;49:873–9. https://doi.org/10.1038/bmt.2014.19.
Tang F, Xu Y, Chen H, Xu L, Zhang X, Wang Y, et al. Comparison of the clinical outcomes of hematologic malignancies after myeloablative haploidentical transplantation with G-CSF/ATG and posttransplant cyclophosphamide: results from the Chinese Bone Marrow Transplantation Registry Group (CBMTRG). Sci China Life Sci. 2020;63:571–81. https://doi.org/10.1007/s11427-019-9594-7.
Bracamonte-Baran W, Burlingham W. Non-inherited maternal antigens, pregnancy, and allotolerance. Biomed J. 2015;38:39–51. https://doi.org/10.4103/2319-4170.143498.
van Rood JJ, Loberiza FR Jr., Zhang MJ, Oudshoorn M, Claas F, Cairo MS, et al. Effect of tolerance to noninherited maternal antigens on the occurrence of graft-versus-host disease after bone marrow transplantation from a parent or an HLA-haploidentical sibling. Blood. 2002;99:1572–7. https://doi.org/10.1182/blood.v99.5.1572.
Ichinohe T, Uchiyama T, Shimazaki C, Matsuo K, Tamaki S, Hino M, et al. Feasibility of HLA-haploidentical hematopoietic stem cell transplantation between noninherited maternal antigen (NIMA)-mismatched family members linked with long-term fetomaternal microchimerism. Blood. 2004;104:3821–8. https://doi.org/10.1182/blood-2004-03-1212.
Hirayama M, Azuma E, Ito T, Keida Y, Komada Y. A feasibility study on the prediction of acute graft-vs.-host disease before hematopoietic stem cell transplantation based on fetomaternal tolerance. Chimerism. 2013;4:84–86. https://doi.org/10.4161/chim.24718.
Hirayama M, Azuma E, Komada Y. Tolerogenic effect of non-inherited maternal antigens in hematopoietic stem cell transplantation. Front Immunol. 2012;3:135 https://doi.org/10.3389/fimmu.2012.00135.
Wang Y, Chang YJ, Xu LP, Liu KY, Liu DH, Zhang XH, et al. Who is the best donor for a related HLA haplotype-mismatched transplant? Blood. 2014;124:843–50. https://doi.org/10.1182/blood-2014-03-563130.
Wang Y, Zhao XY, Xu LP, Zhang XH, Han W, Chen H, et al. Lower incidence of acute GVHD is associated with the rapid recovery of CD4(+)CD25(+)CD45RA(+) regulatory T cells in patients who received haploidentical allografts from NIMA-mismatched donors: A retrospective (development) and prospective (validation) cohort-based study. Oncoimmunology. 2016;5:e1242546 https://doi.org/10.1080/2162402X.2016.1242546.
Kongtim P, Ciurea SO. Who is the best donor for haploidentical stem cell transplantation? Semin Hematol. 2019;56:194–200. https://doi.org/10.1053/j.seminhematol.2018.08.003.
Chang YJ, Luznik L, Fuchs EJ, Huang XJ. How do we choose the best donor for T-cell-replete, HLA-haploidentical transplantation? J Hematol Oncol. 2016;9:35 https://doi.org/10.1186/s13045-016-0265-2.
Tang FF, Sun YQ, Mo XD, Lv M, Chen YH, Wang Y, et al. Incidence, risk factors, and outcomes of primary prolonged isolated thrombocytopenia after haploidentical hematopoietic stem cell transplant. Biol Blood Marrow Transpl. 2020;26:1452–8. https://doi.org/10.1016/j.bbmt.2020.03.024.
Tang FF, Cheng YF, Xu LP, Zhang XH, Yan CH, Han W, et al. Incidence, risk factors, and outcomes of chronic graft-versus-host disease in pediatric patients with hematologic malignancies after T cell-replete myeloablative haploidentical hematopoietic stem cell transplantation with antithymocyte globulin/granulocyte colony-stimulating factor. Biol Blood Marrow Transpl. 2020;26:1655–62. https://doi.org/10.1016/j.bbmt.2020.05.021.
Wang Y, Chen H, Chen J, Han M, Hu J, Jiong H, et al. The consensus on the monitoring, treatment, and prevention of leukemia relapse after allogeneic hematopoietic stem cell transplantation in China. Cancer Lett. 2018;438:63–75. https://doi.org/10.1016/j.canlet.2018.08.030.
Wang Y, Liu QF, Wu DP, Wang JB, Zhang X, Wang HX, et al. Impact of prophylactic/preemptive donor lymphocyte infusion and intensified conditioning for relapsed/refractory leukemia: a real-world study. Sci China Life Sci. 2020;63:1552–64. https://doi.org/10.1007/s11427-019-1610-2.
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, et al. Validation and refinement of the disease risk index for allogeneic stem cell transplantation. Blood. 2014;123:3664–71. https://doi.org/10.1182/blood-2014-01-552984.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transpl. 1995;15:825–8.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 diagnosis and staging working group report. Biol Blood Marrow Transpl. 2015;21:389–401 e381. https://doi.org/10.1016/j.bbmt.2014.12.001.
Tamaki S, Ichinohe T, Matsuo K, Hamajima N, Hirabayashi N, Dohy H, et al. Superior survival of blood and marrow stem cell recipients given maternal grafts over recipients given paternal grafts. Bone Marrow Transpl. 2001;28:375–80. https://doi.org/10.1038/sj.bmt.1703146.
Stern M, Ruggeri L, Mancusi A, Bernardo ME, de Angelis C, Bucher C, et al. Survival after T cell-depleted haploidentical stem cell transplantation is improved using the mother as donor. Blood. 2008;112:2990–5. https://doi.org/10.1182/blood-2008-01-135285.
Matsuoka K, Ichinohe T, Hashimoto D, Asakura S, Tanimoto M, Teshima T. Fetal tolerance to maternal antigens improves the outcome of allogeneic bone marrow transplantation by a CD4+ CD25+ T-cell-dependent mechanism. Blood. 2006;107:404–9. https://doi.org/10.1182/blood-2005-07-3045.
Aoyama K, Koyama M, Matsuoka K, Hashimoto D, Ichinohe T, Harada M, et al. Improved outcome of allogeneic bone marrow transplantation due to breastfeeding-induced tolerance to maternal antigens. Blood. 2009;113:1829–33. https://doi.org/10.1182/blood-2008-05-155283.
Miller RA. The aging immune system: primer and prospectus. Science. 1996;273:70–4. https://doi.org/10.1126/science.273.5271.70.
Lipschitz DA, Udupa KB, Indelicato SR, Das M. Effect of age on second messenger generation in neutrophils. Blood. 1991;78:1347–54.
Kollman C, Howe CW, Anasetti C, Antin JH, Davies SM, Filipovich AH, et al. Donor characteristics as risk factors in recipients after transplantation of bone marrow from unrelated donors: the effect of donor age. Blood. 2001;98:2043–51. https://doi.org/10.1182/blood.v98.7.2043.
Loren AW, Bunin GR, Boudreau C, Champlin RE, Cnaan A, Horowitz MM, et al. Impact of donor and recipient sex and parity on outcomes of HLA-identical sibling allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transpl. 2006;12:758–69. https://doi.org/10.1016/j.bbmt.2006.03.015.
Acknowledgements
This work was supported by the National Key Research and Development Program of China (2019YFC0840606) from the Ministry of Science and Technology, the National Natural Science Foundation of China (81900178, 82070189, 81770189, 81621001, and 81530046), the Science and Technology Project of Guangdong Province of China (2016B030230003), and the Project of Health Collaborative Innovation of Guangzhou City (201704020214).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tang, FF., Zhao, XY., Huo, MR. et al. Comparison of the clinical outcomes between NIMA-mismatched and NIPA-mismatched haploidentical hematopoietic stem cell transplantation for patients with hematological malignancies. Bone Marrow Transplant 56, 2723–2731 (2021). https://doi.org/10.1038/s41409-021-01382-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01382-y