Abstract
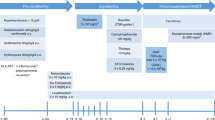
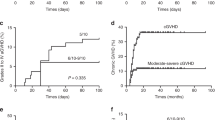
The use of HLA-mismatched (un)related donors is historically associated with a higher incidence of transplant-related complications and mortality. However, the use of such donors may overcome the limited availability of HLA-matched donors for patients with β-thalassemia major (TM) and sickle cell disease (SCD). We investigated hematopoietic stem cell transplantation (HSCT) outcomes of pediatric TM and SCD patients treated with a mismatched donor using a treosulfan-based conditioning in combination with ATG and post-transplant cyclophosphamide (PT-CY) and compared these results to the clinical outcome of patients treated by matched donor HSCT without PT-CY. Thirty-eight children (n = 24 HLA-identical or 10/10-matched donors; n = 14 HLA-mismatched donors), who received a non-depleted bone marrow graft were included. Event-free survival (EFS) and GvHD were not higher in the mismatched PT-Cy group as compared to the matched group. Moreover, despite delayed neutrophil engraftment (day +22 vs. +26, p = 0.002) and immune recovery in the mismatched PT-Cy group, this did not result in more infectious complications. Therefore, we conclude that in the absence of an HLA-identical or a matched unrelated donor, HSCT with a mismatched unrelated or haploidentical donor in combination with ATG plus PT-CY can be considered a safe and effective treatment option for pediatric hemoglobinopathy patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Strocchio L, Locatelli F. Hematopoietic stem cell transplantation in thalassemia. Hematol Oncol Clin North Am. 2018;32:317–28.
Angelucci E, Matthes-Martin S, Baronciani D, Bernaudin F, Bonanomi S, Cappellini MD, et al. Hematopoietic stem cell transplantation in thalassemia major and sickle cell disease: Indications and management recommendations from an international expert panel. Haematologica. 2014;99:811–20.
Cappelli B, Volt F, Tozatto-Maio K, Scigliuolo GM, Ferster A, Dupont S, et al. Risk factors and outcomes according to age at transplantation with an HLA-identical sibling for sickle cell disease. Haematologica. 2019;104:e543–e546.
Stallings AM, Majhail NS, Nowacki AS, Onimoe GI, Hanna R, Piccone CM. Paediatric haematologists’ attitudes regarding haematopoietic cell transplantation as treatment for sickle cell disease. Br J Haematol. 2020;188:976–84.
Khemani K, Ross D, Sinha C, Haight A, Bakshi N, Krishnamurti L. Experiences and decision making in hematopoietic stem cell transplant in sickle cell disease: patients’ and caregivers’ perspectives. Biol Blood Marrow Transpl. 2018;24:1041–8.
Baronciani D, Angelucci E, Potschger U, Gaziev J, Yesilipek A, Zecca M, et al. Hemopoietic stem cell transplantation in thalassemia: a report from the european society for blood and bone marrow transplantation hemoglobinopathy registry, 2000–2010. Bone Marrow Transpl. 2016;51:536–41.
Gluckman E, Cappelli B, Bernaudin F, Labopin M, Volt F, Carreras J, et al. Sickle cell disease: an international survey of results of HLA-identical sibling hematopoietic stem cell transplantation. Blood. 2017;129:1548–56.
Gluckman E, Fuente J, de la, Cappelli B, Scigliuolo GM, Volt F, Tozatto-Maio K, et al. The role of HLA matching in unrelated donor hematopoietic stem cell transplantation for sickle cell disease in Europe. Bone Marrow Transpl. 2020;55:1946–54.
Li C, Mathews V, Kim S, George B, Hebert K, Jiang H, et al. Related and unrelated donor transplantation for β-thalassemia major: Results of an international survey. Blood Adv. 2019;3:2562–70.
Eapen M, Brazauskas R, Walters MC, Bernaudin F, Bo-Subait K, Fitzhugh CD, et al. Effect of donor type and conditioning regimen intensity on allogeneic transplantation outcomes in patients with sickle cell disease: a retrospective multicentre, cohort study. Lancet Haematol. 2019;6:e585–e596.
Brazauskas R, Scigliuolo GM, Wang H, Cappelli B, Ruggeri A, Fitzhugh CD, et al. Risk score to predict event-free survival after hematopoietic cell transplant for sickle cell disease. Blood. 2020;136:623–6.
Tiercy JM. How to select the best available related or unrelated donor of hematopoietic stem cells? Haematologica. 2016;101:680–7.
Gaziev D, Galimberti M, Lucarelli G, Polchi P, Giardini C, Angelucci E, et al. Bone marrow transplantation from alternative donors for thalassemia: HLA-phenotypically identical relative and HLA-nonidentical sibling or parent transplants. Bone Marrow Transpl. 2000;25:815–21.
Bertaina A, Pitisci A, Sinibaldi M, Algeri M. T cell-depleted and T cell-replete HLA-haploidentical stem cell transplantation for non-malignant disorders. Curr Hematol Malig Rep. 2017;12:68–78.
Gaziev J, Isgrò A, Sodani P, Paciaroni K, De Angelis G, Marziali M, et al. Haploidentical HSCT for hemoglobinopathies: Improved outcomes with TCRαβ+/CD19+-depleted grafts. Blood Adv. 2018;2:263–70.
Prem S, Atenafu EG, Al-Shaibani Z, Loach D, Law A, Lam W, et al. Low rates of acute and chronic GVHD with ATG and PTCy in matched and mismatched unrelated donor peripheral blood stem cell transplants. Eur J Haematol. 2019;102:486–93.
Bolaños-Meade J, Fuchs EJ, Luznik L, Lanzkron SM, Gamper CJ, Jones RJ, et al. HLA-haploidentical bone marrow transplantation with posttransplant cyclophosphamide expands the donor pool for patients with sickle cell disease. Blood. 2012;120:4285–91.
Law AD, Salas MQ, Lam W, Michelis FV, Thyagu S, Kim D, et al. Reduced-intensity conditioning and dual T lymphocyte suppression with antithymocyte globulin and post-transplant cyclophosphamide as graft-versus-host disease prophylaxis in haploidentical hematopoietic stem cell transplants for hematological malignancies. Biol Blood Marrow Transpl. 2018;24:2259–64.
Deotare U, Atenafu EG, Loach D, Michelis FV, Kim DH, Thyagu S, et al. Reduction of severe acute graft-versus-host disease using a combination of pre transplant anti-thymocyte globulin and post-transplant cyclophosphamide in matched unrelated donor transplantation. Bone Marrow Transpl. 2018;53:361–5.
Anurathapan U, Hongeng S, Pakakasama S, Songdej D, Sirachainan N, Pongphitcha P, et al. Hematopoietic stem cell transplantation for severe thalassemia patients from haploidentical donors using a novel conditioning regimen. Biol Blood Marrow Transpl. 2020;26:1106–12.
Anurathapan U, Pakakasama S, Rujkijyanont P, Sirachainan N, Songdej D, Chuansumrit A, et al. Pretransplant immunosuppression followed by reduced-toxicity conditioning and stem cell transplantation in high-risk thalassemia: a safe approach to disease control. Biol Blood Marrow Transpl. 2013;19:1259–62.
Admiraal R, van Kesteren C, Jol-van der Zijde CM, van Tol MJD, Bartelink IH, Bredius RGM, et al. Population pharmacokinetic modeling of thymoglobulin®in children receiving allogeneic-hematopoietic cell transplantation: towards improved survival through individualized dosing. Clin Pharmacokinet. 2015;54:435–46.
Oostenbrink LVE, Jol-van der Zijde CM, Kielsen K, Jansen-Hoogendijk AM, Ifversen M, Müller KG, et al. Differential elimination of anti-thymocyte globulin of fresenius and genzyme impacts T-cell reconstitution after hematopoietic stem cell transplantation. Front Immunol. 2019;10:1–11.
Jol-van der Zijde CM, Bredius RGM, Jansen-Hoogendijk AM, Raaijmakers S, Egeler RM, Lankester AC, et al. IgG antibodies to ATG early after pediatric hematopoietic SCT increase the risk of acute GVHD. Bone Marrow Transpl. 2012;47:360–8.
Bolaños-Meade J, Brodsky RA. Blood and marrow transplantation for sickle cell disease: Overcoming barriers to success. Curr Opin Oncol. 2009;21:158–61.
Bolaños-Meade J, Cooke KR, Gamper CJ, Ali SA, Ambinder RF, Borrello IM, et al. Effect of increased dose of total body irradiation on graft failure associated with HLA-haploidentical transplantation in patients with severe haemoglobinopathies: a prospective clinical trial. Lancet Haematol. 2019;6:e183–e193.
Osumi T, Yoshimura S, Sako M, Uchiyama T, Ishikawa T, Kawai T, et al. A prospective study of allogeneic hematopoietic stem cell transplantation with post-transplantation cyclophosphamide and anti-thymoglobulin from HLA-mismatched related donors for non-malignant diseases. Biol Blood Marrow Transpl. 2020;26:e286–e291.
Klein OR, Buddenbaum J, Tucker N, Chen AR, Gamper CJ, Loeb D, et al. Nonmyeloablative haploidentical bone marrow transplantation with post-transplantation cyclophosphamide for pediatric and young adult patients with high-risk hematologic malignancies. Biol Blood Marrow Transpl. 2017;23:325–32.
Laberko A, Sultanova E, Gutovskaya E, Shipitsina I, Shelikhova L, Kurnikova E, et al. Mismatched related vs matched unrelated donors in TCRαβ/CD19-depleted HSCT for primary immunodeficiencies. Blood. 2019;134:1755–63.
Bertaina A, Merli P, Rutella S, Pagliara D, Bernardo ME, Masetti R, et al. HLA-haploidentical stem cell transplantation after removal of αβ+ T and B cells in children with nonmalignant disorders. Blood. 2014;124:822–6.
Mallhi KK, Srikanthan MA, Baker KK, Frangoul HA, Torgerson TR, Petrovic A, et al. HLA-haploidentical hematopoietic cell transplantation for treatment of non-malignant diseases using nonmyeloablative conditioning and post-transplant cyclophosphamide. Biol Blood Marrow Transpl. 2020;26:1332–41.
Wang Y, Wu DP, Liu QF, Xu LP, Liu KY, Zhang XH, et al. Low-dose post-transplant cyclophosphamide and anti-thymocyte globulin as an effective strategy for GVHD prevention in haploidentical patients. J Hematol Oncol. 2019;12:1–9.
Bosch M, Dhadda M, Hoegh-Petersen M, Liu Y, Hagel LM, Podgorny P, et al. Immune reconstitution after anti-thymocyte globulin-conditioned hematopoietic cell transplantation. Cytotherapy. 2012;14:1258–75.
Willemsen L, Jol-van der Zijde CM, Admiraal R, Putter H, Jansen-Hoogendijk AM, Ostaijen-ten Dam MM, et al. Impact of serotherapy on immune reconstitution and survival outcomes after stem cell transplantations in children: thymoglobulin versus alemtuzumab. Biol Blood Marrow Transpl. 2015;21:473–82.
Battipaglia G, Labopin M, Kröger N, Vitek A, Afanasyev B, Hilgendorf I, et al. Posttransplant cyclophosphamide vs antithymocyte globulin in HLA-mismatched unrelated donor transplantation. Blood. 2019;134:892–9.
Nakamae H, Fujii K, Nanno S, Okamura H, Nakane T, Koh H, et al. A prospective observational study of immune reconstitution following transplantation with post-transplant reduced-dose cyclophosphamide from HLA-haploidentical donors. Transpl Int. 2019;32:1322–32.
Russo A, Oliveira G, Berglund S, Greco R, Gambacorta V, Cieri N, et al. NK cell recovery after haploidentical HSCT with posttransplant cyclophosphamide: Dynamics and clinical implications. Blood. 2018;131:247–62.
de la Fuente J, Dhedin N, Koyama T, Bernaudin F, Kuentz M, Karnik L, et al. Haploidentical bone marrow transplantation with post-transplantation cyclophosphamide plus thiotepa improves donor engraftment in patients with sickle cell anemia: results of an international learning collaborative. Biol Blood Marrow Transpl. 2019;25:1197–209.
Acknowledgements
The authors would like to thank the nurses of the Stem Cell Transplant Units for their care of patients and assistance in obtaining patient samples. We acknowledge Gina van der Graaf for her help with measuring total and active ATG.
Funding
The work described in this project is funded in part by Neovii Biotech (Rapperswil, Switzerland). Neovii Biotech has not been involved in data generation, analysis, interpretation nor in the manuscript writing process.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Oostenbrink, L.V.E., Pool, E.S., Jol-van der Zijde, C.M. et al. Successful mismatched hematopoietic stem cell transplantation for pediatric hemoglobinopathy by using ATG and post-transplant cyclophosphamide. Bone Marrow Transplant 56, 2203–2211 (2021). https://doi.org/10.1038/s41409-021-01302-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01302-0
This article is cited by
-
Comparison of haploidentical transplantation and single cord blood transplantation for myelofibrosis
Bone Marrow Transplantation (2024)
-
Excellent outcome of stem cell transplantation for sickle cell disease
Annals of Hematology (2023)
-
Indications for haematopoietic cell transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe, 2022
Bone Marrow Transplantation (2022)