Abstract
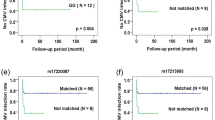
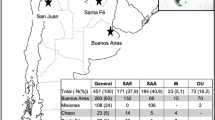
Allele-level HLA compatibility in cord blood transplantation, together with noninherited maternal antigen or NIMA matching, have been associated with better transplant outcomes. The aim of this work is to develop a cost-efficient high-resolution HLA typing strategy based on next-generation sequencing to improve the quality of the Barcelona Cord Blood Bank’s inventory, and to investigate the impact of high-resolution HLA typing and NIMA determination on the preferential selection of cord blood for transplantation. In this line, the developed strategy was validated and the HLA-A, -B, -C, -DRB1, and -DQB1 genes of 5000 cord blood units and 2500 of their associated maternal samples were typed. Subsequently, three study groups of 2012 units each were monitored for up to 2 years: (1) units with high-resolution and maternal HLA typing, (2) units with high-resolution but not maternal typing, and (3) units typed at low-resolution for class I and only high-resolution for HLA-DRB1. Despite a trend toward a greater selection of units with high-resolution typing, no significant impact of these variables was observed. These results highlight the need for evidence-based and globally accepted criteria for cord blood selection, together with the necessity to improve the accessibility of clinicians to donor registry’s data.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Hough R, Danby R, Russell N, Marks D, Veys P, Shaw B, et al. Recommendations for a standard UK approach to incorporating umbilical cord blood into clinical transplantation practice: an update on cord blood unit selection, donor selection algorithms and conditioning protocols. Br J Haematol. 2016;172:360–70.
Kim YJ, Broxmeyer HE. Immune regulatory cells in umbilical cord blood and their potential roles in transplantation tolerance. Crit Rev Oncol Hematol. 2011;79:112–26.
Delaney M, Ballen KK. The role of HLA in umbilical cord blood transplantation. Best Pract Res Clin Haematol. 2010;23:179–87.
Rocha V, Gluckman E, Eurocord-Netcord registry and European Blood and Marrow Transplant group. Improving outcomes of cord blood transplantation: HLA matching, cell dose and other graft- and transplantation-related factors. Br J Haematol. 2009;147:262–74.
Eapen M, Klein JP, Ruggeri A, Spellman S, Lee SJ, Anasetti C, et al. Impact of allele-level HLA matching on outcomes after myeloablative single unit umbilical cord blood transplantation for hematologic malignancy. Blood. 2014;123:133–40.
Mallhi KK, Smith AR, DeFor TE, Lund TC, Orchard PJ, Miller WP. Allele-level HLA matching impacts key outcomes following umbilical cord blood transplantation for inherited metabolic disorders. Biol Blood Marrow Transplant. 2017;23:119–25.
Armstrong AE, Smyth E, Helenowski IB, Tse WT, Duerst RE, Schneiderman J, et al. The impact of high-resolution HLA-A, HLA-B, HLA-C, and HLA-DRB1 on transplant-related outcomes in single-unit umbilical cord blood transplantation in pediatric patients. J Pediatr Hematol Oncol. 2017;39:26–32.
Oran B, Cao K, Saliba RM, Rezvani K, de Lima M, Ahmed S, et al. Better allele-level matching improves transplant-related mortality after double cord blood transplantation. Haematologica. 2015;100:1361–70.
Eapen M, Wang T, Veys PA, Boelens JJ, St Martin A, Spellman S, et al. Allele-level HLA matching for umbilical cord blood transplantation for non-malignant diseases in children: a retrospective analysis. Lancet Haematol. 2017;4:e325–33.
Rocha V. Umbilical cord blood cells from unrelated donor as an alternative source of hematopoietic stem cells for transplantation in children and adults. Semin Hematol. 2016;53:237–45.
Mold JE, Michaëlsson J, Burt TD, Muench MO, Beckerman KP, Busch MP, et al. Maternal alloantigens promote the development of tolerogenic fetal regulatory T cells in utero. Science. 2008;322:1562–5.
Eikmans M, van Halteren AGS, van Besien K, van Rood JJ, Drabbels JJ, Claas FH. Naturally acquired microchimerism: implications for transplantation outcome and novel methodologies for detection. Chimerism. 2014;5:24–39.
Dutta P, Burlingham WJ. Microchimerism: tolerance vs. sensitization. Curr Opin Organ Transplant. 2011;16:359–65.
van Rood JJ, Stevens CE, Smits J, Carrier C, Carpenter C, Scaradavou A. Reexposure of cord blood to noninherited maternal HLA antigens improves transplant outcome in hematological malignancies. Proc Natl Acad Sci USA. 2009;106:19952–7.
Rocha V, Spellman S, Zhang M-J, Ruggeri A, Purtill D, Brady C, et al. Effect of HLA-matching recipients to donor noninherited maternal antigens on outcomes after mismatched umbilical cord blood transplantation for hematologic malignancy. Biol Blood Marrow Transplant. 2012;18:1890–6.
Van der Zanden HG, Van Rood JJ, Oudshoorn M, Bakker JN, Melis A, Brand A, et al. Noninherited maternal antigens identify acceptable HLA mismatches: benefit to patients and cost-effectiveness for cord blood banks. Biol Blood Marrow Transplant. 2014;20:1791–5.
Powley L, Brown C, Melis A, Li Y, Parkes G, Navarrete CV. Consideration of noninherited maternal Ags as permissible HLA mismatches in cord blood donor selection. Bone Marrow Transpl. 2016;51:675–9.
Kwok J, Guo M, Yang W, Ip P, Lee CK, Lu L, et al. Simulation of non-inherited maternal antigens acceptable HLA mismatches to increase the chance of matched cord blood units: Hong Kong’s experience. Hum Immunol. 2018;79:539–44.
De Santis D, Dinauer D, Duke J, Erlich HA, Holcomb CL, Lind C, et al. 16(th) IHIW: Review of HLA typing by NGS. Int J Immunogenet. 2013;40:72–6.
Gabriel C, Fürst D, Faé I, Wenda S, Zollikofer C, Mytilineos J, et al. HLA typing by next-generation sequencing - getting closer to reality. Tissue Antigens. 2014;83:65–75.
Lange V, Böhme I, Hofmann J, Lang K, Sauter J, Schöne B, et al. Cost-efficient high-throughput HLA typing by MiSeq amplicon sequencing. BMC Genom. 2014;15:63.
Danzer M, Niklas N, Stabentheiner S, Hofer K, Pröll J, Stückler C, et al. Rapid, scalable and highly automated HLA genotyping using next-generation sequencing: a transition from research to diagnostics. BMC Genom. 2013;14:221.
Ehrenberg PK, Geretz A, Baldwin KM, Apps R, Polonis VR, Robb ML, et al. High-throughput multiplex HLA genotyping by next-generation sequencing using multi-locus individual tagging. BMC Genom. 2014;15:864.
Ozaki Y, Suzuki S, Kashiwase K, Shigenari A, Okudaira Y, Ito S, et al. Cost-efficient multiplex PCR for routine genotyping of up to nine classical HLA loci in a single analytical run of multiple samples by next generation sequencing. BMC Genom. 2015;16:318.
Enrich E, Campos E, Martorell L, Herrero MJ, Vidal F, Querol S, et al. HLA-A, -B, -C, -DRB1, and -DQB1 allele and haplotype frequencies: an analysis of umbilical cord blood units at the Barcelona Cord Blood Bank. HLA. 2019;94:347–59.
Passweg JR, Baldomero H, Bader P, Bonini C, Cesaro S, Dreger P, et al. Hematopoietic SCT in Europe 2013: recent trends in the use of alternative donors showing more haploidentical donors but fewer cord blood transplants. Bone Marrow Transpl. 2015;50:476–82.
Liu JH, Kanakry CG, Luznik L. Have haploidentical ransplants replaced umbilical cord transplants for acute leukemias? Curr Opin Hematol. 2018;25:103–11.
Passweg JR, Baldomero H, Bader P, Bonini C, Duarte RF, Dufour C, et al. Use of haploidentical stem cell transplantation continues to increase: the 2015 European Society for Blood and Marrow Transplant activity survey report. Bone Marrow Transpl. 2017;52:811–7.
Eapen M, Rubinstein P, Zhang M-J, Stevens C, Kurtzberg J, Scaradavou A, et al. Outcomes of transplantation of unrelated donor umbilical cord blood and bone marrow in children with acute leukaemia: a comparison study. Lancet. 2007;369:1947–54.
Brunstein CG, Gutman JA, Weisdorf DJ, Woolfrey AE, DeFor TE, Gooley TA, et al. Allogeneic hematopoietic cell transplantation for hematologic malignancy: relative risks and benefits of double umbilical cord blood. Blood. 2010;116:4693–9.
Atsuta Y, Morishima Y, Suzuki R, Nagamura-Inoue T, Taniguchi S, Takahashi S, et al. Comparison of unrelated cord blood transplantation and HLA-mismatched unrelated bone marrow transplantation for adults with leukemia. Biol Blood Marrow Transplant. 2012;18:780–7.
Keating AK, Langenhorst J, Wagner JE, Page KM, Veys P, Wynn RF, et al. The influence of stem cell source on transplant outcomes for pediatric patients with acute myeloid leukemia. Blood Adv. 2019;3:1118–28.
Lou X, Zhao C, Chen H. Unrelated donor umbilical cord blood transplant versus unrelated hematopoietic stem cell transplant in patients with acute leukemia: a meta-analysis and systematic review. Blood Rev. 2018;3:192–202.
Lin X, Torrabadella M, Amat L, Gómez S, Azqueta C, Sánchez M, et al. Estimated fetal weight percentile as a tool to predict collection of cord blood units with higher cellular content: implications for prenatal selection of cord blood donors. Transfusion. 2018;58:1732–38.
Purtill D, Smith K, Devlin S, Meagher R, Tonon J, Lubin M, et al. Dominant unit CD34+ cell dose predicts engraftment after double-unit cord blood transplantation and is influenced by bank practice. Blood. 2014;124:2905–12.
Dehn J, Spellman S, Hurley CK, Shaw BE, Barker JN, Burns LJ, et al. Selection of unrelated donors and cord blood units for hematopoietic cell transplantation: guidelines from the NMDP/CIBMTR. Blood. 2019;134:924–34.
de Koning C, Admiraal R, Nierkens S, Boelens JJ. Immune reconstitution and outcomes after conditioning with anti-thymocyte-globulin in unrelated cord blood transplantation; the good, the bad, and the ugly. Stem Cell Investig. 2017;4:38.
Castillo N, García-Cadenas I, Barba P, Canals C, Díaz-Heredia C, Martino R, et al. Early and long-term impaired T lymphocyte immune reconstitution after cord blood transplantation with antithymocyte globulin. Biol Blood Marrow Transplant. 2017;23:491–7.
Huang X, Guo B, Capitano M, Broxmeyer HE. Past, present, and future efforts to enhance the efficacy of cord blood hematopoietic cell transplantation. F1000Res. 2019;8:1833.
Acknowledgements
We would like to thank all the people who made this study possible, in particular Laura Mongay, Pepi Caro, and Carina Lera for their help with HLA typing, and Iris García-Martínez for her help with interpreting the results of the statistical analysis. Also to Jesus Maroto and Silvia Tuset for his collaboration with CB data, and Alejandro Madrigal for his help in the scientific review. Finally, we would like to thank the donors, the members of the Concordia Program, the technicians from the CB Bank and the transplant centers that answered our questionnaires. No specific funding was obtained to perform this study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The complete design of the study, together with the use of the CB samples analyzed in this work was approved by the Vall d’Hebron University Hospital’s ethics committee (PR(AG)59/2017). According to “Plan Nacional de Sangre de Cordón Umbilical”, developed in Spain in 2006, all donors signed an informed consent for CBU donation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Enrich, E., Vidal, F., Corrales, I. et al. Improving cord blood typing with next-generation sequencing: impact of allele-level HLA and NIMA determination on their selection for transplantation. Bone Marrow Transplant 55, 1623–1631 (2020). https://doi.org/10.1038/s41409-020-0890-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-0890-9