Abstract
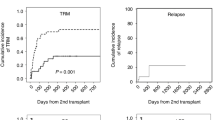
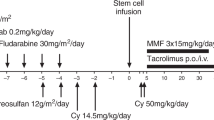
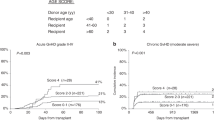
We report the outcome of 19 patients who experienced primary graft failure (PrGF) after a haploidentical (HAPLO), unmanipulated bone marrow transplant. The median age of patients was 52 years; the conditioning regimen of the first HAPLO transplant was either full dose total body irradiation (TBI) or fludarabine, busulfan, and thiotepa (TBF); PTCY was given to all patients together with cyclosporine and mycophenolate. All 19 patients with PrGF received a second HAPLO graft, at a median interval of 42 days (34–82) after HSCT, using the Baltimore protocol and G-CSF mobilized PB from the same (n = 13) or another HAPLO family donor (n = 6). GvHD prophylaxis was again PTCY-based; 14/19 patients had trilineage recovery (74%) and 1-year survival was 66%. Engraftment at second HAPLO was seen in 7/8 patient with, and in 5/7 patients without donor-specific antibodies (DSA). In a multivariate logistic regression analysis on the original group of 503 patients, there was a trend for a reduced dose of busulfan, to increase the risk of PrGF (p = 0.1). In conclusion, patients with PrGF following a HAPLO transplant, can be rescued with a second early HAPLO transplant, using the same or a different donor.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Passweg JR, Baldomero H, Bader P, Bonini C, Duarte RF, Dufour C, et al. Use of haploidentical stem cell transplantation continues to increase: the 2015 European Society for Blood and Marrow Transplant activity survey report. Bone Marrow Transpl. 2017;52:811–7.
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transpl. 2008;14:641–50.
Lu DP, Dong L, Wu T, Huang XJ, Zhang MJ, Han W, et al. Conditioning including antithymocyte globulin followed by unmanipulated HLA-mismatched/haploidentical blood and marrow transplantation can achieve comparable outcomes with HLA-identical sibling transplantation. Blood. 2006;107:3065–73.
Locatelli F, Bauquet A, Palumbo, Moretta F, Bertaina A. Negative depletion of α/β+ T cells and of CD19+ B lymphocytes: a novel frontier to optimize the effect of innate immunity in HLA-mismatched hematopoietic stem cell transplantation. Immunol Lett. 2013;155:21–3.
Wang Y, Chang YJ, Xu LP, Liu KY, Liu DH, Zhang XH, et al. Who is the best donor for a related HLA haplotype-mismatched transplant? Blood. 2014;124(Aug):843–50. 7
McCurdy SR, Kanakry JA, Showel MM, Tsai HL, Bolaños-Meade J, Rosner GL, et al. Risk-stratified outcomes of nonmyeloablative HLA-haploidentical BMT with high-dose posttransplantation cyclophosphamide. Blood. 2015;125:3024–31.
Ozdemir ZN, Bozdağ SC. Graft failure after allogeneic hematopoietic stem cell transplantation. Transfus Apheresis Sci. 2018;57:163–7.
Olsson RF, Logan BR, Chaudhury S, Zhu X, Akpek G, Bolwell BJ, et al. Primary graft failure after myeloablative allogeneic hematopoietic cell transplantation for hematologic malignancies. Leukemia. 2015;29:1754–62.
Stasia A, Ghiso A, Galaverna F, Raiola AM, Gualandi F, Luchetti S, et al. CD34 selected cells for the treatment of poor graft function after allogeneic stem cell transplantation. Biol Blood Marrow Transpl. 2014;20:1440–3.
Nakamura H, Gress RE. Graft rejection by cytolytic T cells. Specificity of the effector mechanism in the rejection of allogeneic marrow. Transplantation. 1990;49:453–8.
Kernan NA, Flomenberg N, Dupont B, O’Reilly RJ. Graft rejection in recipients of T-cell-depleted HLA- non identical marrow transplants for leukemia. Identification of host-derived antidonor allocytotoxic T lymphocytes. Transplantation. 1987;43:842–7.
Ciurea SO, Thall PF, Milton DR, Barnes TH, Kongtim P, Carmazzi Y, et al. Complement-binding donor-specific anti-HLA antibodies and risk of primary graft failure in hematopoietic stem cell transplantation. Biol Blood Marrow Transpl. 2015;21:1392–8.
Ciurea SO, de Lima M, Cano, Korbling M, Giralt S, Shpall EJ, et al. High risk of graft failure in patients with anti-HLA antibodies undergoing haploidentical stem-cell transplantation. Transplantation. 2009;88:1019–24. 27
Yoshihara S, Maruya E, Taniguchi K, Kaida K, Kato R, Inoue T, et al. Risk and prevention of graft failure in patients with preexisting donor-specific HLA antibodies undergoing unmanipulated haploidentical SCT. Bone Marrow Transpl. 2012;47:508–15.
Chang YJ, Zhao XY, Xu LP, Zhang XH, Wang Y, Han W, et al. Donor-specific anti-human leukocyte antigen antibodies were associated with primary graft failure after unmanipulated haploidentical blood and marrow transplantation: a prospective study with randomly assigned training and validation sets. J Hematol Oncol. 2015;10:84.
Takanashi M, Atsuta Y, Fujiwara K, Kodo H, Kai S, Sato H, et al. The impact of anti-HLA antibodies on unrelated cord blood transplantations. Blood. 2010;116:2839–46.
Ruggeri A, Rocha V, Masson E, Labopin M, Cunha R, Absi L, et al. Impact of donor-specific anti-HLA antibodies on graft failure and survival after reduced intensity conditioning-unrelated cord blood transplantation: a Eurocord, Société Francophone d’Histocompatibilité et d’Immunogénétique (SFHI) and Société Française de Greffe de Moelle et de Thérapie Cellulaire (SFGM-TC) analysis. Haematologica. 2013;98:1154–60.
Bramanti S, Calafiore V, Longhi E, Mariotti J, Crespiatico L, Sarina B, et al. Donor-specific anti-HLA antibodies in haploidentical stem cell transplantation with post-transplantation cyclophosphamide: risk of graft failure, poor graft function, and impact on outcomes. Biol Blood Marrow Transpl. 2019;25:1395–46.
Prata PH, Resche-Rigon M, Blaise D, Socié G, Rohrlich PS, Milpied N, et al. Outcomes of salvage haploidentical transplant with post-transplant cyclophosphamide for rescuing graft failure patients: a report on behalf of the francophone society of bone marrow transplantation and cellular therapy. Biol Blood Marrow Transpl. 2019;25:1798–802.
Raiola AM, Dominietto A, Ghiso A, Di Grazia C, Lamparelli T, Gualandi F, et al. Unmanipulated haploidentical bone marrow transplantation and posttransplantation cyclophosphamide for hematologic malignancies after myeloablative conditioning. Biol Blood Marrow Transpl. 2013;19:117–22.
Lion T, Watzinger F, Preuner S, Kreyenberg H, Tilanus M, de Weger R, et al. The EuroChimerism concept for a standardized approach to chimerism analysis after allogeneic stem cell transplantation. Leukemia. 2012;26:1821–8.
Fuchs EJ. HLA-haploidentical blood or marrow transplantation with high-dose, post-transplantation cyclophosphamide. Bone Marrow Transpl. 2015;50 Suppl 2:S31–6.
Ferrà C, Sanz J, Díaz-Pérez MA, Morgades M, Gayoso M, Cabrera JR, et al. Outcome of graft failure after allogeneic stem cell transplant: study of 89 patients. Leuk Lymphoma. 2015;56:656–62.
Ruggeri A, Labopin M, Bacigalupo A, Gülbas 4, Koc Y, Blaise D, et al. Bone marrow versus mobilized peripheral blood stem cells, in haploidentical transplants, using post-transplant cyclophosphamide. Cancer. 2018;124:1428–37.
Bashey A, Zhang MJ, McCurdy SR, St Martin A, Argall T, Anasetti C, et al. Mobilized peripheral blood stem cells versus unstimulated bone marrow as a graft source for T-cell–replete haploidentical donor transplantation using post-transplant cyclophosphamide. J Clin Oncol. 2017;35:3002–9.
Remberger M, Watz E, Ringdén O, Mattsson J, Shanwell A, Wikman A. Major ABO blood group mismatch increases the risk for graft failure after unrelated donor hematopoietic stem cell transplantation. Biol Blood Marrow Transpl. 2007;13:675–82.
Canaani J, Savani BN, Labopin M, Huang XJ, Ciceri F, Arcese W, et al. Impact of ABO incompatibility on patients’ outcome after haploidentical hematopoietic stem cell transplantation for acute myeloid leukemia—a report from the Acute Leukemia Working Party of the EBMT. Haematologica. 2017;102:1066–74.
Rondón G, Saliba RM, Khouri I, Giralt S, Chan K, Jabbour E, et al. Long-term follow-up of patients who experienced graft failure postallogeneic progenitor cell transplantation. Results of a single institution analysis. Biol Blood Marrow Transpl. 2008;14:859–66.
Acknowledgements
This study was supported by AIRC, Milano, Grant to AB.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Giammarco, S., Raiola, A.M., Di Grazia, C. et al. Second haploidentical stem cell transplantation for primary graft failure. Bone Marrow Transplant 56, 1291–1296 (2021). https://doi.org/10.1038/s41409-020-01183-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-01183-9
This article is cited by
-
Graft failure after allogeneic hematopoietic stem cell transplantation in pediatric patients with acute leukemia: autologous reconstitution or second transplant?
Stem Cell Research & Therapy (2024)
-
Donor specific antibodies (DSA): the only risk factor for primary graft failure?
Bone Marrow Transplantation (2024)
-
Second haploidentical bone marrow transplantation with antithymocyte antibody-containing conditioning regimen for graft failure in eight patients with severe aplastic anemia
Scientific Reports (2024)
-
Salvage haploidentical transplantation for graft failure after first haploidentical allogeneic stem cell transplantation: an updated experience
Bone Marrow Transplantation (2024)
-
Effects of donor-specific antibodies on engraftment and long-term survival after allogeneic hematopoietic stem cell transplantation—A systematic review and meta-analysis
Bone Marrow Transplantation (2023)