Abstract
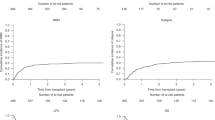
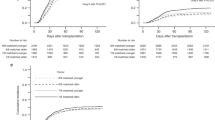
In allogeneic hematopoietic stem cell transplantation (allo-HSCT), the effects of patient and donor human leukocyte antigen (HLA) matching status on graft-versus-host disease (GVHD) have been extensively elucidated, but the effects of specific HLAs on acute GVHD remain unclear. Using data from a Japanese registry, we retrospectively analyzed 4392 patients with leukemia or myelodysplastic syndrome who received transplants from HLA-identical sibling donors to investigate the effects of HLAs on acute GVHD. From unbiased searches of HLA-A, -B, and -DR, HLA-B60 was significantly associated with an increased risk of grades II–IV acute GVHD (HR, 1.34; 95% CI, 1.13–1.59; P = 0.001). In contrast, HLA-B62 was significantly associated with a decreased risk of grades II–IV (HR, 0.73; 95% CI, 0.62–0.87; P < 0.001) and III–IV acute GVHD (HR, 0.63; 95% CI, 0.46–0.87; P = 0.005). The risk of leukemia relapse was significantly higher in HLA-B62-positive patients than in HLA-B62-negative patients (HR, 1.23; 95% CI, 1.05–1.43; P = 0.01). Both HLA-B60 and -B62 did not affect overall survival. The findings of this study may by implication suggest the possibility that the effects of specific HLAs on transplant outcomes may reflect inherent biological features, and thus consideration of specific HLAs may be helpful to predict transplant outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Sasazuki T, Juji T, Morishima Y, Kinukawa N, Kashiwabara H, Inoko H, et al. Effect of matching of class I HLA alleles on clinical outcome after transplantation of hematopoietic stem cells from an unrelated donor. Japan Marrow Donor Program. N Engl J Med. 1998;339:1177–85.
Lee SJ, Klein J, Haagenson M, Baxter-Lowe LA, Confer DL, Eapen M, et al. High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood. 2007;110:4576–83.
Morishima Y, Kashiwase K, Matsuo K, Azuma F, Morishima S, Onizuka M, et al. Biological significance of HLA locus matching in unrelated donor bone marrow transplantation. Blood. 2015;125:1189–97.
Shiina T, Hosomichi K, Inoko H, Kulski JK. The HLA genomic loci map: expression, interaction, diversity and disease. J Hum Genet. 2009;54:15–39.
Battiwalla M, Hahn T, Radovic M, Roy H, Wahab A, Duman E, et al. Human leukocyte antigen (HLA) DR15 is associated with reduced incidence of acute GVHD in HLA-matched allogeneic transplantation but does not impact chronic GVHD incidence. Blood. 2006;107:1970–3.
Stern M, Passweg J, Tiercy JM, Genitsch A, Meyer-Monard S, Heim D, et al. Human leukocyte antigen DR15 is associated with reduced relapse rate and improved survival after human leukocyte antigen-identical sibling hematopoietic stem cell transplantation. Biol Blood Marrow Transpl. 2006;12:1169–75.
Davidson JA, Tate DG, Poulton KV, Lucas GS, Yin JL, Liakopoulou EF, et al. HLA-DR15, reduced relapse rate and improved survival after HLA identical sibling hemopoietic stem cell transplantation. Biol Blood Marrow Transpl. 2007;13:493–4.
Khouri IF, Bassett R, Poindexter N, O’Brien S, Bueso-Ramos CE, Hsu Y, et al. Nonmyeloablative allogeneic stem cell transplantation in relapsed/refractory chronic lymphocytic leukemia: long-term follow-up, prognostic factors, and effect of human leukocyte histocompatibility antigen subtype on outcome. Cancer. 2011;117:4679–88.
Morishima S, Ogawa S, Matsubara A, Kawase T, Nannya Y, Kashiwase K, et al. Impact of highly conserved HLA haplotype on acute graft-versus-host disease. Blood. 2010;115:4664–70.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Cox D. Regression model and life tables. J R Stat Soc B. 1972;34:187–200.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened bythe center for international blood and marrow transplant research. Biol Blood Marrow Transpl. 2009;15:367–9.
Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18:695–706.
Horowitz MM, Gale RP, Sondel PM, Goldman JM, Kersey J, Kolb HJ, et al. Graft-versus-leukemia reactions after bone marrow transplantation. Blood 1990;75:555–62.
Weisdorf D, Hakke R, Blazar B, Miller W, McGlave P, Ramsay N, et al. Risk factors for acute graft-versus-host disease in histocompatible donor bone marrow transplantation. Transplantation. 1991;51:1197–203.
Smyth LA, Witt CS, Christiansen FT, Herrmann RP, Hollingsworth PN, Townend DC, et al. The MHC influences acute graft versus host disease in MHC matched adults undergoing allogeneic bone marrow transplantation. Bone Marrow Transpl. 1993;12:351–5.
Martin PJ, Gooley T, Anasetti C, Petersdorf EW, Hansen JA. HLAs and risk of acute graft-vs.-host disease after marrow transplantation from an HLA-identical sibling. Biol Blood Marrow Transpl. 1998;4:128–33.
Battiwalla M, Ellis K, Li P, Pavletic SZ, Akpek G, Hematti P, et al. HLA DR15 antigen status does not impact graft-versus-host disease or survival in HLA-matched sibling transplantation for hematologic malignancies. Biol Blood Marrow Transpl. 2012;18:1302–8.
Spierings E. Minor histocompatibility antigens: past, present, and future. Tissue Antigens. 2014;84:374–360.
Macdonald WA, Purcell AW, Mifsud NA, Ely LK, Williams DS, Chang L, et al. A naturally selected dimorphism within the HLA-B44 supertype alters class I structure, peptide repertoire, and T cell recognition. J Exp Med. 2003;198:679–91.
Sidney J, Peters B, Frahm N, Brander C, Sette A. HLA class I supertypes: a revised and updated classification. BMC Immunol. 2008;9:1.
Gaudieri S, Leelayuwat C, Tay GK, Townend DC, Dawkins RL. The major histocompatability complex (MHC) contains conserved polymorphic genomic sequences that are shuffled by recombination to form ethnic-specific haplotypes. J Mol Evol. 1997;45:17–23.
Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, Blumenstiel B, et al. The structure of haplotype blocks in the human genome. Science. 2002;296:2225–9.
Price P, Witt C, Allcock R, Sayer D, Garlepp M, Kok CC, et al. The genetic basis for the association of the 8.1 ancestral haplotype (A1, B8, DR3) with multiple immunopathological diseases. Immunol Rev. 1999;167:257–74.
Marsh SG, Albert ED, Bodmer WF, Bontrop RE, Dupont B, Erlich HA, et al. Nomenclature for factors of the HLA system, 2010. Tissue Antigens. 2010;75:291–455.
Ikeda N, Kojima H, Nishikawa M, Hayashi K, Futagami T, Tsujino T, et al. Determination of HLA-A, -C, -B, -DRB1 allele and haplotype frequency in Japanese population based on family study. Tissue Antigens. 2015;85:252–9.
Chowell D, Morris LGT, Grigg CM, Weber JK, Samstein RM, Makarov V, et al. Patient HLA class I genotype influences cancer response to checkpoint blockade immunotherapy. Science. 2018;359:582–7.
Cortes A, Pulit SL, Leo PJ, Pointon JJ, Robinson PC, Weisman MH, et al. Major histocompatibility complex associations of ankylosing spondylitis are complex and involve further epistasis with ERAP1. Nat Commun. 2015;6:7146.
Diaz-Pena R, Vidal-Castineira JR, Lopez-Vazquez A, Lopez-Larrea C. HLA-B*40:01 is associated with ankylosing spondylitis in HLA-B27-positive populations. J Rheumatol. 2016;43:1255–6.
Petersdorf EW, Gooley TA, Malkki M, Bacigalupo AP, Cesbron A, Du Toit E, et al. HLA-C expression levels define permissible mismatches in hematopoietic cell transplantation. Blood. 2014;124:3996–4003.
Maiers M, Gragert L, Klitz W. High-resolution HLA alleles and haplotypes in the United States population. Hum Immunol. 2007;68:779–88.
Acknowledgements
The authors thank all of the physicians and data managers who contributed valuable transplantation data to the Japan Society for Hematopoietic Cell Transplantation (JSHCT). We also thank the members of the data management committee of the JSHCT for their assistance. This work was supported by JSPS KAKENHI Grant Number 17K09934, 20K08737, and MEXT KAKENHI Grant Number 19H04811 to SM.
HLA Working Group of the Japan Society for Hematopoietic Cell Transplantation
Satoko Morishima, Yoshiko Atsuta, Kazuhiro Ikegame, Tatsuo Ichinohe, Atae Utsunomiya, Makoto Onizuka, Shunichi Kato, Takakazu Kawase, Junya Kanda, Yoshinobu Kanda, Sung-Won Kim, Takeshi Kobayashi, Yoshifusa Takatsuka, Yoshiyuki Takahashi, Junji Tanaka, Hiroya Tamaki, Masanori Tsuji, Tetsuya Nishida, Yoshinobu Maeda, Masayoshi Masuko, Ryosuke Matsuno, Makoto Murata, Yasuo Morishima, Hisayuki Yokoyama, Atsushi Wake, Nobuhiro Watanabe, Takashi Ashida, Minoko Takanashi, Takumi Hoshino, Toshio Yabe, Kana Sakamoto, Shigeo Fuji, Koichi Miyamura, Nobuyoshi Arima, Eisei Kondo, Koji Kawamura, Takahito Kawata, Kenji Kishimoto, Raine Tatara, Takeshi Hagino, Shin-Ichiro Fujiwara, Yoshimitsu Shimomura, Hirotoshi Sakaguchi, Shigeki Hirabayashi, Hiroto Ishii, Yoshiyuki Onda, Itaru Kato, Akihisa Kawajiri, Takero Shindo, Masahito Tokunaga, Atsushi Nonami, Hiroyuki Muranushi, Noriyoshi Yoshinaga, Naomi Kawashima, Souichi Shiratori, Yuma Tada, Susumu Tanoue, Masahiro Hirayama, Keiko Fukunaga, Marie Ohbiki, Fumihiro Azuma, Minoru Kaneya, Takahiro Fujino, Takaya Yamashita, Shouhei Tomori, Yuki Takeuchi, Takahiko Sato, Kaoru Morita, Norina Tanaka, Fumiya Wada, Taro Edahiro, Makoto Iwasaki, Kento Umino
Author information
Authors and Affiliations
Consortia
Contributions
SM designed the research, organized the project, performed the statistical analysis, and analyzed the data; YM analyzed and interpreted the data; TF, ND, TM, MO, TKaw, CK, YO, MT, MK, TKam, MI, JT, TI, and YA gathered and organized the data; SM and YM wrote the paper. All authors checked the final version of the paper.
Corresponding author
Ethics declarations
Conflict of interest
MK: Research Funding; Otsuka Pharmaceutical Co., Ltd., Astellas Pharma, Novartis Pharmaceuticals, Pfizer Seiyaku KK, Shionogi & Co., Ltd, Honoraria; Otsuka Pharmaceutical Co., Ltd., Astellas Pharma, Shionogi & Co., Ltd. The other authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the HLA Working Group of the Japan Society for Hematopoietic Cell Transplantation are listed below Acknowledgements.
Supplementary information
Rights and permissions
About this article
Cite this article
Morishima, S., Fukuda, T., Doki, N. et al. Individual HLAs influence immunological events in allogeneic stem cell transplantation from HLA-identical sibling donors. Bone Marrow Transplant 56, 646–654 (2021). https://doi.org/10.1038/s41409-020-01070-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-01070-3