Abstract
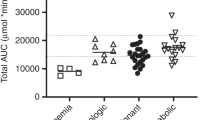
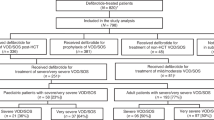
Veno-occlusive disease (VOD) is a severe adverse reaction to busulfan-containing regimens used in the preparation of children for hematopoietic stem cell transplantation (HSCT). We conducted a retrospective analysis of data to examine determinants of VOD in children who received IV busulfan for HSCT conditioning. Busulfan PK parameters as well as various indices (maximal concentration—Cmax, area under the concentration-time curve—AUC) were estimated using a validated Bayesian approach. The influence of available PK, demographic, and clinical variables on the incidence of VOD was evaluated by using logistic regression and classification and regression tree (CART) analyses. Among the 293 patients included, the mean age was 6.5 years and the mean actual body weight was 26.3 kg. The incidence of VOD was 25.6%. Busulfan Cmax as well as weight <9 kg or age <3 years were identified as independent predictors of VOD in logistic regression analysis. CART analysis identified busulfan Cmax over the entire regimen as the strongest predictor of VOD. This study suggests that busulfan-associated VOD is in part a concentration-dependent reaction. In addition, the youngest children showed the highest risk of VOD. These findings may have important implications for busulfan dosing and therapeutic drug monitoring practice in HSCT children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Santos GW, Tutschka PJ, Brookmeyer R, Saral R, Beschorner WE, Bias WB, et al. Marrow transplantation for acute nonlymphocytic leukemia after treatment with busulfan and cyclophosphamide. N Engl J Med. 1983;309:1347–53.
Schuler US, Renner UD, Kroschinsky F, Johne C, Jenke A, Naumann R, et al. Intravenous busulphan for conditioning before autologous or allogeneic human blood stem cell transplantation. Br J Haematol. 2001;114:944–50.
Cohen A, Békássy AN, Gaiero A, Faraci M, Zecca S, Tichelli A, et al. Endocrinological late complications after hematopoietic SCT in children. Bone Marrow Transplant. 2008;41:S43–48.
Faraci M, Békássy AN, De Fazio V, Tichelli A, Dini G. EBMT Paediatric and Late Effects Working Parties. Non-endocrine late complications in children after allogeneic haematopoietic SCT. Bone Marrow Transplant. 2008;41:S49–57.
McCune JS, Gooley T, Gibbs JP, Sanders JE, Petersdorf EW, Appelbaum FR, et al. Busulfan concentration and graft rejection in pediatric patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant. 2002;30:167–73.
Slattery JT, Sanders JE, Buckner CD, Schaffer RL, Lambert KW, Langer FP, et al. Graft-rejection and toxicity following bone marrow transplantation in relation to busulfan pharmacokinetics. Bone Marrow Transplant. 1995;16:31–42.
Bartelink IH, Lalmohamed A, van Reij EML, Dvorak CC, Savic RM, Zwaveling J, et al. Association of busulfan exposure with survival and toxicity after haemopoietic cell transplantation in children and young adults: a multicentre, retrospective cohort analysis. Lancet Haematol. 2016;3:e526–36.
Kumar S, DeLeve LD, Kamath PS, Tefferi A. Hepatic veno-occlusive disease (sinusoidal obstruction syndrome) after hematopoietic stem cell transplantation. Mayo Clin Proc. 2003;78:589–98.
Coppell JA, Richardson PG, Soiffer R, Martin PL, Kernan NA, Chen A, et al. Hepatic veno-occlusive disease following stem cell transplantation: incidence, clinical course, and outcome. Biol Blood Marrow Transplant. 2010;16:157–68.
Corbacioglu S, Cesaro S, Faraci M, Valteau-Couanet D, Gruhn B, Rovelli A, et al. Defibrotide for prophylaxis of hepatic veno-occlusive disease in paediatric haemopoietic stem-cell transplantation: an open-label, phase 3, randomised controlled trial. Lancet. 2012;379:1301–9.
Dix SP, Wingard JR, Mullins RE, Jerkunica I, Davidson TG, Gilmore CE, et al. Association of busulfan area under the curve with veno-occlusive disease following BMT. Bone Marrow Transplant. 1996;17:225–30.
Grochow LB, Jones RJ, Brundrett RB, Braine HG, Chen TL, Saral R, et al. Pharmacokinetics of busulfan: correlation with veno-occlusive disease in patients undergoing bone marrow transplantation. Cancer Chemother Pharmacol. 1989;25:55–61.
McCune JS et al. Plasma concentration monitoring of busulfan: does it improve clinical outcome? Clin Pharmacokinet 2000; 39:155–65. https://www.ncbi.nlm.nih.gov/pubmed/?term=Plasma+concentration+monitoring+of+busulfan%3A+does+it+improve+clinical+outcome%3F+Clin+Pharmacokinet.+2000 . Accessed 28 Sep 2017.
Bartelink IH, Bredius RGM, Belitser SV, Suttorp MM, Bierings M, Knibbe CAJ, et al. Association between busulfan exposure and outcome in children receiving intravenous busulfan before hematologic stem cell transplantation. Biol Blood Marrow Transplant. 2009;15:231–41.
Vassal G, Michel G, Espérou H, Gentet JC, Valteau-Couanet D, Doz F, et al. Prospective validation of a novel IV busulfan fixed dosing for paediatric patients to improve therapeutic AUC targeting without drug monitoring. Cancer Chemother Pharmacol. 2008;61:113–23.
Geddes M, Kangarloo SB, Naveed F, Quinlan D, Chaudhry MA, Stewart D, et al. High busulfan exposure is associated with worse outcomes in a daily i.v. busulfan and fludarabine allogeneic transplant regimen. Biol Blood Marrow Transplant. 2008;14:220–8.
Michel G, Valteau-Couanet D, Gentet J-C, Esperou H, Socié G, Méchinaud F, et al. Weight-based strategy of dose administration in children using intravenous busulfan: clinical and pharmacokinetic results. Pediatr Blood Cancer. 2012;58:90–97.
Neely M, Philippe M, Rushing T, Fu X, van Guilder M, Bayard D, et al. Accurately achieving target busulfan exposure in children and adolescents with very limited sampling and the BestDose software. Ther Drug Monit. 2016;38:332–42.
Neely MN, van Guilder MG, Yamada WM, Schumitzky A, Jelliffe RW. Accurate detection of outliers and subpopulations with Pmetrics, a nonparametric and parametric pharmacometric modeling and simulation package for R. Ther Drug Monit. 2012;34:467–76.
Philippe M, Neely M, Bertrand Y, Bleyzac N, Goutelle S. A nonparametric method to optimize initial drug dosing and attainment of a target exposure interval: concepts and application to busulfan in pediatrics. Clin Pharmacokinet. 2017;56:435–47.
McDonald GB, Hinds MS, Fisher LD, Schoch HG, Wolford JL, Banaji M, et al. Veno-occlusive disease of the liver and multiorgan failure after bone marrow transplantation: a cohort study of 355 patients. Ann Intern Med. 1993;118:255–67.
Bearman SI. The syndrome of hepatic veno-occlusive disease after marrow transplantation. Blood. 1995;85:3005–20.
R Development Core Team (2005). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0. http://www.R-project.org.
Malär R, Sjöö F, Rentsch K, Hassan M, Güngör T. Therapeutic drug monitoring is essential for intravenous busulfan therapy in pediatric hematopoietic stem cell recipients. Pediatr Transplant. 2011;15:580–8.
Tesfaye H, Branova R, Klapkova E, Prusa R, Janeckova D, Riha P, et al. The importance of therapeutic drug monitoring (TDM) for parenteral busulfan dosing in conditioning regimen for hematopoietic stem cell transplantation (HSCT) in children. Ann Transplant. 2014;19:214–24.
Schechter T, Finkelstein Y, Doyle J, Verjee Z, Moretti M, Koren G, et al. Pharmacokinetic disposition and clinical outcomes in infants and children receiving intravenous busulfan for allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2007;13:307–14.
Okamoto Y, Nagatoshi Y, Kosaka Y, Kikuchi A, Kato S, Kigasawa H, et al. Prospective pharmacokinetic study of intravenous busulfan in hematopoietic stem cell transplantation in 25 children. Pediatr Transplant. 2014;18:294–301.
Ansari M, Théoret Y, Rezgui MA, Peters C, Mezziani S, Desjean C, et al. Association between busulfan exposure and outcome in children receiving intravenous busulfan before hematopoietic stem cell transplantation. Ther Drug Monit. 2014;36:93–99.
Wolf MB, Baynes JW. The anti-cancer drug, doxorubicin, causes oxidant stress-induced endothelial dysfunction. Biochim Biophys Acta. 2006;1760:267–71.
Mercanoglu F, Turkmen A, Kocaman O, Pinarbasi B, Dursun M, Selcukbiricik F, et al. Endothelial dysfunction in renal transplant patients is closely related to serum cyclosporine levels. Transplant Proc. 2004;36:1357–60.
Russell JA, Tran HT, Quinlan D, Chaudhry A, Duggan P, Brown C, et al. Once-daily intravenous busulfan given with fludarabine as conditioning for allogeneic stem cell transplantation: study of pharmacokinetics and early clinical outcomes. Biol Blood Marrow Transplant. 2002;8:468–76.
Andersson BS, de Lima M, Thall PF, Wang X, Couriel D, Korbling M, et al. Once daily i.v. busulfan and fludarabine (i.v. Bu-Flu) compares favorably with i.v. busulfan and cyclophosphamide (i.v. BuCy2) as pretransplant conditioning therapy in AML/MDS. Biol Blood Marrow Transplant. 2008;14:672–84.
Chae YS, Sohn SK, Kim JG, Cho YY, Moon JH, Shin HJ, et al. New myeloablative conditioning regimen with fludarabine and busulfan for allogeneic stem cell transplantation: comparison with BuCy2. Bone Marrow Transplant. 2007;40:541–7.
Liu H, Zhai X, Song Z, Sun J, Xiao Y, Nie D, et al. Busulfan plus fludarabine as a myeloablative conditioning regimen compared with busulfan plus cyclophosphamide for acute myeloid leukemia in first complete remission undergoing allogeneic hematopoietic stem cell transplantation: a prospective and multicenter study. J Hematol Oncol. 2013;6:15.
Nguyen L, Fuller D, Lennon S, Leger F, Puozzo CIV. busulfan in pediatrics: a novel dosing to improve safety/efficacy for hematopoietic progenitor cell transplantation recipients. Bone Marrow Transplant. 2004;33:979–87.
Ryu S-G, Lee J-H, Choi S-J, Lee J-H, Lee Y-S, Seol M, et al. Randomized comparison of four-times-daily versus once-daily intravenous busulfan in conditioning therapy for hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2007;13:1095–105.
de Lima M, Couriel D, Thall PF, Wang X, Madden T, Jones R, et al. Once-daily intravenous busulfan and fludarabine: clinical and pharmacokinetic results of a myeloablative, reduced-toxicity conditioning regimen for allogeneic stem cell transplantation in AML and MDS. Blood. 2004;104:857–64.
Russell JA, Savoie ML, Balogh A, Turner AR, Larratt L, Chaudhry MA, et al. Allogeneic transplantation for adult acute leukemia in first and second remission with a novel regimen incorporating daily intravenous busulfan, fludarabine, 400 CGY total-body irradiation, and thymoglobulin. Biol Blood Marrow Transplant. 2007;13:814–21.
Pidala J, Kim J, Anasetti C, Kharfan-Dabaja MA, Field T, Perkins J, et al. Targeted i.v. BU and fludarabine (t-i.v. BU/Flu) provides effective control of AML in adults with reduced toxicity. Bone Marrow Transplant. 2011;46:641–9.
Perkins JB, Kim J, Anasetti C, Fernandez HF, Perez LE, Ayala E, et al. Maximally tolerated busulfan systemic exposure in combination with fludarabine as conditioning before allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2012;18:1099–107.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15:1628–33.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transplant. 2009;15:367–9.
Bartelink IH, Bredius RGM, Ververs TT, Raphael MF, Kesteren C, van, Bierings M, et al. Once-daily intravenous busulfan with therapeutic drug monitoring compared to conventional oral busulfan improves survival and engraftment in children undergoing allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2008;14:88–98.
González-Vicent M, Molina B, Pérez A, Díaz MA. Once-daily intravenous busulfan for 47 pediatric patients undergoing autologous hematopoietic stem cell transplantation: A Single Center Study. J Pediatr Hematol Oncol. 2012;34:180.
Zwaveling J, den Hartigh J, Lankester AC, Guchelaar H-J, Egeler RM, Bredius RG, et al. Once-daily intravenous busulfan in children prior to stem cell transplantation: study of pharmacokinetics and early clinical outcomes. Anticancer Drugs. 2006;17:1099–105.
Copelan EA, Bechtel TP, Avalos BR, Elder PJ, Ezzone SA, Scholl MD, et al. Busulfan levels are influenced by prior treatment and are associated with hepatic veno-occlusive disease and early mortality but not with delayed complications following marrow transplantation. Bone Marrow Transplant. 2001;27:1121–4.
Acknowledgements
MP, SG, MN, and NB designed the research study. MP and TR collected the data. MP, SG, and TR analyzed the data. MP and SG wrote the paper. TR, MN, and NB critically revised the manuscript. All authors approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Philippe, M., Neely, M., Rushing, T. et al. Maximal concentration of intravenous busulfan as a determinant of veno-occlusive disease: a pharmacokinetic-pharmacodynamic analysis in 293 hematopoietic stem cell transplanted children. Bone Marrow Transplant 54, 448–457 (2019). https://doi.org/10.1038/s41409-018-0281-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-018-0281-7
This article is cited by
-
Outcomes of haploidentical bone marrow transplantation in infant acute leukemia: a single center experience
Bone Marrow Transplantation (2024)
-
Evaluation of different pharmacokinetically guided IV busulfan exposure ranges on adult patient outcomes after hematopoietic stem cell transplantation
Annals of Hematology (2023)
-
Population Pharmacokinetic Model of Intravenous Busulfan in Hematopoietic Cell Transplantation: Systematic Review and Comparative Simulations
Clinical Pharmacokinetics (2023)
-
Clinical outcomes of individualized busulfan-dosing in hematopoietic stem cell transplantation in Chinese children undergoing with therapeutic drug monitoring
Bone Marrow Transplantation (2022)
-
Impact of busulfan pharmacokinetics on outcome in adult patients receiving an allogeneic hematopoietic cell transplantation
Bone Marrow Transplantation (2022)