Abstract
Current drug therapy for myeloproliferative neoplasms, including essential thrombocythemia (ET) and polycythemia vera (PV), is neither curative nor has it been shown to prolong survival. Fortunately, prognosis in ET and PV is relatively good, with median survivals in younger patients estimated at 33 and 24 years, respectively. Therefore, when it comes to treatment in ET or PV, less is more and one should avoid exposing patients to new drugs that have not been shown to be disease-modifying, and whose long-term consequences are suspect (e.g., ruxolitinib). Furthermore, the main indication for treatment in ET and PV is to prevent thrombosis and, in that regard, none of the newer drugs have been shown to be superior to the time-tested older drugs (e.g., hydroxyurea). We currently consider three major risk factors for thrombosis (history of thrombosis, JAK2/MPL mutations, and advanced age), in order to group ET patients into four risk categories: “very low risk” (absence of all three risk factors); “low risk” (presence of JAK2/MPL mutations); “intermediate-risk” (presence of advanced age); and “high-risk” (presence of thrombosis history or presence of both JAK2/MPL mutations and advanced age). Herein, we provide a point-of-care treatment algorithm that is risk-adapted and based on evidence and decades of experience.
Similar content being viewed by others
Introduction
The term myeloproliferative neoplasms (MPN) typically refers to essential thrombocythemia (ET), polycythemia vera (PV), and primary myelofibrosis (PMF)1; in addition, some patients with ET or PV might in time progress into a PMF-like post-ET or post-PV myelofibrosis2. As a group, ET, PV, and PMF share three mutually exclusive “driver” mutations, including JAK2, CALR, and MPL3. The most frequent driver mutation is JAK2V617F, found in ~99% of patients with PV, 55% ET, and 65% PMF4. The driver mutation distributions in ET and PMF are similar with 50–65% of the patients being JAK2V617F mutated, 15–30% being CALR mutated, and 4–8% being MPL mutated4, while 10–20% of the patients might not express any one of the three mutations (i.e., are triple-negative)4.
World Health Organization (WHO)-consistent diagnosis of ET requires a platelet count of ≥450 × 10(9)/L, presence of one of the three aforementioned driver mutations or in their absence the exclusion of other causes of thrombocytosis (reactive and clonal), and bone marrow morphologic assessment, especially for distinguishing ET from prefibrotic PMF and “masked” PV5,6. In addition to clonal thrombocytosis, a variable proportion of patients with ET might display mild splenomegaly, leukocytosis, microvascular symptoms, thrombotic and bleeding complications, increased occurrence of first trimester miscarriage, and time-dependent risk of leukemic transformation or fibrotic progression7.
Survival in patients with any one of the three JAK2 mutation-enriched MPN is significantly shorter than that of the sex- and age-adjusted control population, with median estimates of 20 years for ET, 14 years for PV, and 6 years for PMF8. Causes of death include leukemic transformation, with 15-year estimates of ~2.1–5.3% for ET, 5.5–18.7% for PV, and more than 20% for PMF9. Fibrotic progression rates in ET and PV, during a similar time interval, are estimated at 4–11% and 6–14%, respectively9. To date, drug therapy has not been shown to modify the natural history of these diseases, prevent leukemic or fibrotic progression or prolong survival10. Current indication for drug therapy in ET and PV is to prevent thrombotic complications, especially in high-risk patients7. In the current review, we provide a risk-adapted treatment algorithm in ET that can be used in daily practice.
Risk-adapted treatment algorithm in essential thrombocythemia
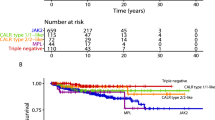
Survival and its prognostic determinants
Life expectancy in ET is only mildly compromised with median survival for patients younger than 60 years of age approaching 33 years8. In addition to age, other clinical risk factors for survival in ET include leukocytosis and thrombosis history11. On the other hand, neither abnormal karyotype (detected in ~7% of patients)12 nor driver mutational status13 in ET has been shown to affect overall or leukemia-free survival; however, JAK2/MPL-mutated patients are significantly more thrombosis prone while MPL-mutated cases might be at a higher risk for fibrotic progression13,14,15.
A recent targeted sequencing study revealed that mutations or DNA variants, other than JAK2, CALR, or MPL, are found in ~53% of patients with ET with the most frequent being TET2 (16%), ASXL1 (11%), DNMT3A (6%), and SF3B1 (5%)16. The particular study identified SH2B3, SF3B1, U2AF1, TP53, IDH2, and EZH2 mutations as risk factors for overall, myelofibrosis-free or leukemia-free survival; at least one of these mutations was seen in ~15% of the patients and median survival of patients with and without adverse mutations were 9 and 22 years, respectively. Furthermore, the effect on survival from these adverse mutations was not accounted for by current clinically devised prognostic models and the observations were validated in an external cohort of patients16. Most recently, serum lactate dehydrogenase (LDH) level in ET was shown to correlate with shortened survival, suggesting its value as a biologically more accurate measure of myeloproliferation (as opposed to leukocytosis) and possible surrogate for occult prefibrotic PMF17.
Taking the above discussion into consideration, it is important to identify the risk factor-free subset of ET patients, since their survival might not be significantly different from the age- and sex-matched control population; such patients are represented by morphologic confirmation of WHO-defined ET (as opposed to prefibrotic PMF), younger age, absence of thrombosis history, absence of leukocytosis, normal LDH, and absence of MPL or other adverse mutations, as outlined above. On the other hand, the presence of risk factors for survival is currently not used to dictate treatment, since specific therapy in ET has not been shown to affect survival. Accordingly, although advised after securing insurance coverage and patient permission, we do not believe it is currently crucial to obtain next-generation sequencing (NGS) in ET. In other words, at the present time, identification of survival risk factors in ET is used to counsel patients and disease-monitoring purposes and not for treatment decisions.
Thrombosis and its prognostic determinants
Current treatment in ET is primarily indicated for the purposes of preventing thrombotic complications, which might occur in 10–20% of patients. In this regard, the two-tiered traditional risk stratification considers two risk parameters: age >60 years and history of thrombosis. Accordingly, patients with either one of these two risk factors were classified as “traditional high-risk” and the absence of both risk factors defined the “traditional low-risk” groups. More recently, however, several studies have identified the presence of JAK2/MPL mutations as another independent risk factor for thrombosis in ET18,19. More specifically, risk factors for arterial thrombosis included thrombosis history, age >60 years, presence of JAK2V617F, leukocytosis, and CV risk factors and for venous thrombosis male gender19, while a lower risk of thrombosis was shown in patients with extreme thrombocytosis19 and in those with CALR mutations20,21.
Contemporary risk stratification
Thrombosis data from 1019 patients with WHO-defined ET was recently re-analyzed18; among the “traditional low-risk” group, annual thrombosis rate was the lowest in patients who lacked both JAK2/MPL mutations and CV risk factors (0.44%), non-significantly higher in JAK2-unmutated patients with CV risk factors (1.05%) and significantly higher in JAK2-mutated patients with (2.57%) or without (1.59%) CV risk factors; there was no significant difference between JAK2-mutated “traditional low-risk” patients with or without CV risk factors. In the “traditional high-risk” group, the particular study18 identified thrombosis history as being significantly more detrimental than advanced age and also showed that the adverse effect of JAK2 mutations was more apparent in patients whose high-risk status was determined by advanced age while its additional effect on patients with thrombosis history was limited; these observations from the revised international prognostic scoring system for essential thrombocythemia thrombosis were recently validated by another study22.
Based on the above, we currently consider four risk groups in ET: “very low-risk group” is defined by the absence of all three independent risk factors for thrombosis, including history of thrombosis, JAK2/MPL mutations, and advanced age; “low-risk” group is defined by the presence of JAK2/MPL mutations in otherwise younger patients without history of thrombosis; “intermediate-risk” group refers to JAK2/MPL unmutated older patients without thrombosis history; and “high-risk” group is defined by either presence of thrombosis history or presence of JAK2/MPL mutation in an older patient (Fig. 1).
Risk-adapted therapy: “very low-risk” disease
At present, there is no evidence from prospective controlled studies to guide treatment recommendations for each one of the above-mentioned four risk categories in ET. Until such information becomes available, it is reasonable to simply observe patients with “very low-risk” disease without CV risk factors and consider once-daily aspirin therapy only in the presence of CV risk factors (Fig. 1). In other words, aspirin therapy in “very low-risk” ET should not be automatic, especially considering the fact that a substantial proportion of such patients display acquired von Willebrand syndrome (AVWS) with increased bleeding diathesis23; this particular complication is more likely to occur in the presence of extreme thrombocytosis24. Furthermore, other studies have suggested the value of aspirin therapy in reducing the risk of arterial thrombosis in low-risk ET associated with CV risk factors, but not otherwise25. Because patients with “very low-risk” ET are either CALR mutated or triple-negative, they usually display extreme thrombocytosis, which does not require specific treatment per se, regardless of how high the platelet count might be, as long as patient remains asymptomatic. On the other hand, if such patients with extreme thrombocytosis develop symptoms or bleeding complications, it is reasonable to use a cytoreductive agent, with a goal of keeping the platelet count commensurate with the resolution of the particular symptom.
Risk-adapted therapy: “low-risk” disease
In “low-risk” ET (i.e., young JAK2/MPL-mutated without thrombosis history), the aforementioned recent studies have disclosed a residual risk of thrombosis despite management according to traditional treatment guidelines18,26. Therefore, it is reasonable to consider further optimization of aspirin therapy in such patients by following “twice-daily” rather than “once-daily” schedule, especially in the presence of CV risk factors26. The rationale for twice-daily aspirin dosing in “low-risk” JAK2/MPL-mutated ET patients is primarily based on emerging data on the inadequacy of once-daily aspirin dosing for 24-h optimal suppression of thromboxane-A2 synthesis, in the presence of high platelet turnover, and demonstration of superior biological efficacy in ET with twice-daily dosing27,28.
Risk-adapted therapy: “intermediate-risk” disease
Recent studies have suggested that “advanced age,” by itself, was a weak risk factor for thrombosis and may not be as detrimental as thrombosis history18,26. These observations have led us to split the “traditionally high-risk” ET category into “intermediate risk,” defined by the presence of advanced age without history of thrombosis or JAK2/MPL mutations, and “high risk,” defined by presence of thrombosis history or presence of both advanced age and JAK2/MPL mutations. Such distinction is therapeutically relevant since it provides the option of avoiding cytoreductive therapy in JAK2/MPL unmutated older patients without history of thrombosis or CV risk factors (Fig. 1); in one of the aforementioned studies18, the annual risk of thrombosis in such patients was 1.44%, compared to 4.17% in the presence of both JAK2 mutations and CV risk factors (p = 0.01), and was similar to that of “low-risk” patients (1.59–2.57%). Accordingly, we do not believe that it is mandatory to use cytoreductive therapy in such patients (Fig. 1).
Risk-adapted therapy: “high-risk” disease
Decades ago, “high-risk” disease in ET was defined by the presence of one of three clinical parameters: history of thrombosis, advanced age, and long duration of thrombocytosis29. Subsequently, in a randomized study using hydroxyurea for high-risk disease, patients with platelet count >1500 × 10(9)/L were excluded because it was felt that such patients required treatment because of increased bleeding diathesis30. Over the years, it has become evident that extreme thrombocytosis in ET did not, by itself, increase thrombosis risk and might actually be associated with a reduced risk of arterial thrombosis19,31. Also, the bleeding diathesis associated with extreme thrombocytosis has been linked to AVWS24, which might occur both in the presence and absence of extreme thrombocytosis23, and is effectively screened for and managed appropriately. Therefore, platelet count per se should no longer be used for risk stratification in ET.
Regardless, management of “traditionally high-risk” ET has been primarily guided by results of a randomized study of hydroxyurea vs no cytoreductive treatment, in high-risk patients, with the goal of keeping the platelet count below 600 × 10(9)/L30; the study showed a statistically significant benefit for hydroxyurea therapy (thrombosis rate of 3.6 vs 24%). Since then, unsuccessful attempts have been made to improve upon hydroxyurea treatment in ET32,33. Accordingly, hydroxyurea, combined with once-daily aspirin therapy34, remains the standard of care for contemporarily classified “high-risk” patients (Fig. 1). However, there is room for improvement in our conventional treatment approach18,26 and we underscore the need to maximize anti-thrombotic activity, by shortening the aspirin dosing schedule to every 12 h, for patients with history of arterial thrombosis, and securing long-term systemic anticoagulation, in patients with history of venous thrombosis (Fig. 1). In addition, it is reasonable to continue with once-daily aspirin therapy, along with systemic anticoagulation, in patients who are at risk for arterial thrombosis (Fig. 1). In this regard, there is evidence for the additional value of aspirin therapy in the prevention of recurrent venous thrombosis35,36.
Treatment options for hydroxyurea intolerant or refractory patients
There are currently four drugs to consider as second-line therapy in ET: pegylated interferon-α (IFN-α), busulfan, anagrelide, and pipobroman. Among these, our current choice for second-line therapy is pegylated IFN-α (starting dose 90 mcg SC weekly). Pegylated IFN-α treatment in ET has been shown to be relatively safe and effective, and has been associated with both clinical (70–80%) and molecular (10–20%) remissions in some patients, especially in the presence of CALR mutations37,38; however, the relevance of the latter observation, in terms of meaningful health outcome, remains uncertain. Busulfan (starting dose 2–4 mg/day) is a reasonable alternative drug for second-line therapy in ET and it too has been shown to be safe and effective as well as induce molecular remissions in both ET and PV39,40; in hydroxyurea intolerant or refractory patients with ET or PV, the drug was shown to induce durable hematologic response in the majority of patients and molecular response in a minority41,42,43. In addressing the ongoing concern regarding drug leukemogenicity, a large international study of over 1500 patients with PV found no evidence that implicated busulfan, IFN-α, or hydroxyurea, while confirming the particular association with pipobroman44. In a noteworthy vote of confidence regarding busulfan use in MPN, a prominent hematologist underscored the fact that busulfan displayed less DNA/RNA binding, compared to other alkylating agents, no inter- or intra-strand DNA binding and no immunosuppression45.
Anagrelide has been evaluated, in controlled studies, for its efficacy and safety as first-line therapy for ET32,33; the results of these studies suggested that anagrelide was not inferior to hydroxyurea in one study33, but might have been harmful to patients in the second study32. In the latter study, patients receiving anagrelide experienced higher incidences of arterial thrombosis, bleeding complications, and fibrotic progression. Similarly, non-controlled studies have suggested that more than a quarter of patients receiving anagrelide therapy become anemic while a lesser percentage experience renal insufficiency and cardiac complications including arrhythmia and cardiomyopathy46,47,48,49,50. Therefore, we currently consider anagrelide therapy only after failure of all other drug options, including hydroxyurea, IFN-α, and busulfan. Finally, despite some uncontrolled reports of safety and efficacy51,52,53, we currently do not recommend pipobroman treatment in ET, because of controlled evidence for leukemogenicity, seen in patients with PV54.
Management during pregnancy
Current treatment recommendations in young women wishing to be pregnant or are pregnant include once-daily aspirin for “very low-risk” or “low-risk” disease and pegylated IFN-α for high-risk disease55. Both aspirin and IFN-α therapy have been shown to be safe for use during pregnancy and might be associated with lower miscarriage rates in women with ET55,56,57. The additional value of other measures, including platelet apheresis or low molecular weight heparin, is unclear and not recommended58.
Conclusions
The most important first step in the management of ET is to confirm the accuracy of the diagnosis and make sure that other myeloid neoplasms, which might mimic ET in their presentation (e.g., prefibrotic PMF, masked polycythemia vera, chronic myeloid leukemia, refractory anemia with ring sideroblasts, and thrombocytosis), are excluded. Most patients with WHO-defined ET can expect a normal life expectancy with very low risk of leukemic transformation or fibrotic progression and a diagnosis of ET should not deter one from continuing with normal life activities, including sports, air travel, and pregnancy. Patients with ET should be informed about their driver mutational status and its prognostic and therapeutic implications. In this regard, aspirin therapy is very important for JAK2-mutated patients, because of their increased risk for arterial thrombosis. MPL mutations are infrequent in ET (~3%) and their presence raises the possibility of occult prefibrotic PMF or an increased risk of fibrotic progression. Observation alone remains a viable treatment option for “very low-risk” patients with ET while all other patients might benefit from aspirin therapy, in a once- or twice-daily schedule. In addition, cytoreductive treatment is strongly encouraged in patients with thrombosis history, and our first- and second-line drugs of choice in this regard are hydroxyurea and pegylated IFN-α, respectively. On the other hand, we no longer insist on the use of cytoreductive therapy in older patients without previous vascular events, provided they are JAK2/MPL unmutated.
References
Arber, D. A. et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 127, 2391–2405 (2016).
Barosi, G. et al. Proposed criteria for the diagnosis of post-polycythemia vera and post-essential thrombocythemia myelofibrosis: a consensus statement from the International Working Group for Myelofibrosis Research and Treatment. Leukemia 22, 437–438 (2008).
Tefferi, A. Myeloproliferative neoplasms: a decade of discoveries and treatment advances. Am. J. Hematol. 91, 50–58 (2016).
Tefferi, A. & Pardanani, A. Myeloproliferative neoplasms: a contemporary review. JAMA Oncol. 1, 97–105 (2015).
Barbui, T. et al. The 2016 revision of WHO classification of myeloproliferative neoplasms: clinical and molecular advances. Blood Rev. 30, 453–459 (2016).
Kvasnicka H. M. et al. European LeukemiaNet study on the reproducibility of bone marrow features in masked polycythemia vera and differentiation from essential thrombocythemia. Am. J. Hematol. 92, 1062–1067 (2017).
Tefferi, A. & Barbui, T. Polycythemia vera and essential thrombocythemia: 2017 update on diagnosis, risk-stratification, and management. Am. J. Hematol. 92, 94–108 (2017).
Tefferi, A. et al. Long-term survival and blast transformation in molecularly annotated essential thrombocythemia, polycythemia vera, and myelofibrosis. Blood 124, 2507–2513 (2014). quiz 2615.
Cerquozzi, S. & Tefferi, A. Blast transformation and fibrotic progression in polycythemia vera and essential thrombocythemia: a literature review of incidence and risk factors. Blood Cancer J. 5, e366 (2015).
Cervantes, F. & Pereira, A. Does ruxolitinib prolong the survival of patients with myelofibrosis? Blood 129, 832–837 (2017).
Passamonti, F. et al. A prognostic model to predict survival in 867 World Health Organization-defined essential thrombocythemia at diagnosis: a study by the International Working Group on Myelofibrosis Research and Treatment. Blood 120, 1197–1201 (2012).
Gangat, N. et al. Cytogenetic abnormalities in essential thrombocythemia: prevalence and prognostic significance. Eur. J. Haematol. 83, 17–21 (2009).
Elala, Y. C. et al. Calreticulin variant stratified driver mutational status and prognosis in essential thrombocythemia. Am. J. Hematol. 91, 503–506 (2016).
Haider, M., Elala, Y. C., Gangat, N., Hanson, C. A. & Tefferi, A. MPL mutations and palpable splenomegaly are independent risk factors for fibrotic progression in essential thrombocythemia. Blood Cancer J. 6, e487 (2016).
Tefferi, A. et al. Calreticulin mutations and long-term survival in essential thrombocythemia. Leukemia 28, 2300–2303 (2014).
Tefferi, A. et al. Targeted deep sequencing in polycythemia vera and essential thrombocythemia. Blood Adv. 1, 21–30 (2016).
Mudireddy, M. et al. The prognostic relevance of serum lactate dehydrogenase and mild bone marrow reticulin fibrosis in essential thrombocythemia. Am. J. Hematol. 92, 454–459 (2017).
Barbui, T. et al. Practice-relevant revision of IPSET-thrombosis based on 1019 patients with WHO-defined essential thrombocythemia. Blood Cancer J. 5, e369 (2015).
Carobbio, A. et al. Risk factors for arterial and venous thrombosis in WHO-defined essential thrombocythemia: an international study of 891 patients. Blood 117, 5857–5859 (2011).
Finazzi, G. et al. Calreticulin mutation does not modify the IPSET score for predicting the risk of thrombosis among 1150 patients with essential thrombocythemia. Blood 124, 2611–2612 (2014).
Rotunno, G. et al. Impact of calreticulin mutations on clinical and hematological phenotype and outcome in essential thrombocythemia. Blood 123, 1552–1555 (2014).
Haider, M. et al. Validation of the revised International Prognostic Score of Thrombosis for Essential Thrombocythemia (IPSET-thrombosis) in 585 Mayo Clinic patients. Am. J. Hematol. 91, 390–394 (2016).
Rottenstreich, A. et al. Factors related to the development of acquired von Willebrand syndrome in patients with essential thrombocythemia and polycythemia vera. Eur. J. Intern. Med. 41, 49–54 (2017).
Michiels, J. J. Acquired von Willebrand disease due to increasing platelet count can readily explain the paradox of thrombosis and bleeding in thrombocythemia. Clin. Appl. Thromb. Hemost. 5, 147–151 (1999).
Alvarez-Larran, A. et al Observation versus antiplatelet therapy as primary prophylaxis for thrombosis in low-risk essential thrombocythemia. Blood 116, 1205–1210 (2010).
Barbui, T. et al Development and validation of an International Prognostic Score of thrombosis in World Health Organization-essential thrombocythemia (IPSET-thrombosis). Blood 120, 5128–5133 (2012).
Dillinger, J. G. et al. Twice daily aspirin to improve biological aspirin efficacy in patients with essential thrombocythemia. Thromb. Res. 129, 91–94 (2012).
Pascale, S. et al. Aspirin-insensitive thromboxane biosynthesis in essential thrombocythemia is explained by accelerated renewal of the drug target. Blood 119, 3595–3603 (2012).
Cortelazzo, S. et al. Incidence and risk factors for thrombotic complications in a historical cohort of 100 patients with essential thrombocythemia. J. Clin. Oncol. 8, 556–562 (1990).
Cortelazzo, S. et al. Hydroxyurea for patients with essential thrombocythemia and a high risk of thrombosis. N. Engl. J. Med. 332, 1132–1136 (1995).
Latagliata, R. et al. High platelet count at diagnosis is a protective factor for thrombosis in patients with essential thrombocythemia. Thromb. Res. 156, 168–171 (2017).
Harrison, C. N. et al. Hydroxyurea compared with anagrelide in high-risk essential thrombocythemia. N. Engl. J. Med. 353, 33–45 (2005).
Gisslinger, H. et al. Anagrelide compared with hydroxyurea in WHO-classified essential thrombocythemia: the ANAHYDRET Study, a randomized controlled trial. Blood 121, 1720–1728 (2013).
Alvarez-Larran, A. et al. Cytoreduction plus low-dose aspirin versus cytoreduction alone as primary prophylaxis of thrombosis in patients with high-risk essential thrombocythaemia: an observational study. Br. J. Haematol. 161, 865–871 (2013).
Becattini, C. et al. Aspirin for preventing the recurrence of venous thromboembolism. N. Engl. J. Med. 366, 1959–1967 (2012).
Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy--III: reduction in venous thrombosis and pulmonary embolism by antiplatelet prophylaxis among surgical and medical patients. BMJ. 308, 235–246 (1994).
Verger, E. et al. Clinical and molecular response to interferon-alpha therapy in essential thrombocythemia patients with CALR mutations. Blood 126, 2585–2591 (2015).
Quintas-Cardama, A. et al. Molecular analysis of patients with polycythemia vera or essential thrombocythemia receiving pegylated interferon alpha-2a. Blood 122, 893–901 (2013).
Shvidel, L. et al. Busulphan is safe and efficient treatment in elderly patients with essential thrombocythemia. Leukemia 21, 2071–2072 (2007).
Kuriakose, E. T. et al. JAK2V617F allele burden is reduced by busulfan therapy: a new observation using an old drug. Haematologica 98, e135–e137 (2013).
Alvarez-Larran, A. et al. Busulfan in patients with polycythemia vera or essential thrombocythemia refractory or intolerant to hydroxyurea. Ann. Hematol. 93, 2037–2043 (2014).
Begna, K. et al. Busulfan for the treatment of myeloproliferative neoplasms: the Mayo Clinic experience. Blood Cancer J. 6, e427 (2016).
Douglas, G. et al. Busulfan is effective second-line therapy for older patients with Philadelphia-negative myeloproliferative neoplasms intolerant of or unresponsive to hydroxyurea. Leuk. Lymphoma 58, 89–95 (2017).
Tefferi, A. et al. Survival and prognosis among 1545 patients with contemporary polycythemia vera: an international study. Leukemia 27, 1874–1881 (2013).
Brodsky, I. Busulfan versus hydroxyurea in the treatment of polycythemia vera (PV) and essential thrombocythemia (ET). Am. J. Clin. Oncol. 21, 105–106 (1998).
Mela Osorio, M. J. et al. Long-term follow-up of essential thrombocythemia patients treated with anagrelide: subgroup analysis according to JAK2/CALR/MPL mutational status. Eur. J. Haematol. 96, 435–442 (2016).
Storen, E. C. & Tefferi, A. Long-term use of anagrelide in young patients with essential thrombocythemia. Blood 97, 863–866 (2001).
Jurgens, D. J., Moreno-Aspitia, A. & Tefferi, A. Anagrelide-associated cardiomyopathy in polycythemia vera and essential thrombocythemia. Haematologica 89, 1394–1395 (2004).
Mazzucconi, M. G. et al. A long-term study of young patients with essential thrombocythemia treated with anagrelide. Haematologica 89, 1306–1313 (2004).
Engel, P. J., Johnson, H., Baughman, R. P. & Richards, A. I. High-output heart failure associated with anagrelide therapy for essential thrombocytosis. Ann. Intern. Med. 143, 311–313 (2005).
Passamonti, F. et al. Long-term follow-up of young patients with essential thrombocythemia treated with pipobroman. Ann. Hematol. 83, 495–497 (2004).
Mazzucconi, M. G. et al. Pipobroman therapy of essential thrombocythemia. Scand. J. Haematol. 37, 306–309 (1986).
De Sanctis, V. et al. Long-term evaluation of 164 patients with essential thrombocythaemia treated with pipobroman: occurrence of leukaemic evolution. Br. J. Haematol. 123, 517–521 (2003).
Kiladjian, J. J., Chevret, S., Dosquet, C., Chomienne, C. & Rain, J. D. Treatment of polycythemia vera with hydroxyurea and pipobroman: final results of a randomized trial initiated in 1980. J. Clin. Oncol. 29, 3907–3913 (2011).
Tefferi, A. & Passamonti, F. Essential thrombocythemia and pregnancy: Observations from recent studies and management recommendations. Am. J. Hematol. 84, 629–630 (2009).
Gangat, N., Wolanskyj, A. P., Schwager, S. & Tefferi, A. Predictors of pregnancy outcome in essential thrombocythemia: a single institution study of 63 pregnancies. Eur. J. Haematol. 82, 350–353 (2009).
Beauverd, Y. et al. Pegylated interferon alpha-2a for essential thrombocythemia during pregnancy: outcome and safety. A case series. Haematologica 101, e182–e184 (2016).
Valera, M. C., Parant, O., Vayssiere, C., Arnal, J. F. & Payrastre, B. Essential thrombocythemia and pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 158, 141–147 (2011).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tefferi, A., Vannucchi, A.M. & Barbui, T. Essential thrombocythemia treatment algorithm 2018. Blood Cancer Journal 8, 2 (2018). https://doi.org/10.1038/s41408-017-0041-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-017-0041-8
This article is cited by
-
ROP-ET: a prospective phase III trial investigating the efficacy and safety of ropeginterferon alfa-2b in essential thrombocythemia patients with limited treatment options
Annals of Hematology (2024)
-
A case of JAK2 V617F positive essential thrombocythemia successfully controlled by imatinib mesylate
Annals of Hematology (2022)
-
Management Issues and Controversies in Low-Risk Patients with Essential Thrombocythemia and Polycythemia Vera
Current Hematologic Malignancy Reports (2021)
-
Comparison of the effects between MPL and JAK2V617F on thrombosis and peripheral blood cell counts in patients with essential thrombocythemia: a meta-analysis
Annals of Hematology (2021)
-
Cerebrovascular manifestations in hematological diseases: an update
Journal of Neurology (2021)