Abstract
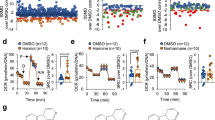
Tricyclic antidepressants (TCAs) are widely used to treat depression and anxiety-related mood disorders. But evidence shows that TCAs elevate blood glucose levels and inhibit insulin secretion, suggesting that TCAs are a risk factor, particularly for individuals with diabetes. Curcumin is a bioactive molecule from the rhizome of the Curcuma longa plant, which has shown both antidepressant and anti-diabetic activities. In the present study, we investigated the protective effect of curcumin against desipramine-induced apoptosis in β cells and the underlying molecular mechanisms. In the mouse forced swimming test (FST), we found that lower doses of desipramine (5 and 10 mg/kg) or curcumin (2.5 mg/kg) alone did not affect the immobility time, whereas combined treatment with curcumin (2.5 mg/kg) and desipramine (5, 10 mg/kg) significantly decreased the immobility time. Furthermore, desipramine dose-dependently inhibited insulin secretion and elevated blood glucose levels, whereas the combined treatment normalized insulin secretion and blood glucose levels. In RIN-m5F pancreatic β-cells, desipramine (10 μM) significantly reduced the cell viability, whereas desipramine combined with curcumin dose-dependently prevented the desipramine-induced impairment in glucose-induced insulin release, most effectively with curcumin (1 and 10 μM). We demonstrated that desipramine treatment promoted the cleavage and activation of Caspase 3 in RIN-m5F cells. Curcumin treatment inhibited desipramine-induced apoptosis, increased mitochondrial membrane potential and Bcl-2/Bax ratio. Desipramine increased the generation of reactive oxygen species, which was reversed by curcumin treatment. Curcumin also inhibited the translocation of forkhead box protein O1 (FOXO1) from the cytoplasm to the nucleus and suppressed the binding of A-kinase anchor protein 150 (AKAP150) to protein phosphatase 2B (PP2B, known as calcineurin) that was induced by desipramine. These results suggest that curcumin protects RIN-m5F pancreatic β-cells against desipramine-induced apoptosis by inhibiting the phosphoinositide 3-kinase/AKT/FOXO1 pathway and the AKAP150/PKA/PP2B interaction. This study suggests that curcumin may have therapeutic potential as an adjunct to antidepressant treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Smith K. Mental health: a world of depression. Nature. 2014;515:181.
Zhang Y, Liu C, Zhao Y, Zhang X, Li B, Cui R. The effects of calorie restriction in depression and potential mechanisms. Curr Neuropharmacol. 2015;13:536–42.
McCarron RM, Shapiro B, Rawles J, Luo J. Depression. Ann Intern Med. 2021;174:ITC65–80.
Kapoor R, Peyear TA, Koeppe RE 2nd, Andersen OS. Antidepressants are modifiers of lipid bilayer properties. J Gen Physiol. 2019;151:342–56.
Arias HR, Vázquez-Gómez E, Hernández-Abrego A, Gallino S, Feuerbach D, Ortells MO, et al. Tricyclic antidepressants inhibit hippocampal α7* and α9α10 nicotinic acetylcholine receptors by different mechanisms. Int J Biochem Cell Biol. 2018;100:1–10.
Chockalingam R, Gott BM, Conway CR. Tricyclic antidepressants and monoamine oxidase inhibitors: are they too old for a new look? Handb Exp Pharmacol. 2019;250:37–48.
Arroll B, Macgillivray S, Ogston S, Reid I, Sullivan F, Williams B, et al. Efficacy and tolerability of tricyclic antidepressants and SSRIs compared with placebo for treatment of depression in primary care: a meta-analysis. Ann Fam Med. 2005;3:449–56.
Brown LC, Majumdar SR, Johnson JA. Type of antidepressant therapy and risk of type 2 diabetes in people with depression. Diabetes Res Clin Pract. 2008;79:61–7.
Fang YJ, Wu TY, Lai JN, Lin CL, Tien N, Lim YP. Association between depression, antidepression medications, and the risk of developing type 2 diabetes mellitus: a nationwide population-based retrospective cohort study in Taiwan. Biomed Res Int. 2021;2021:8857230.
Barnard K, Peveler RC, Holt RI. Antidepressant medication as a risk factor for type 2 diabetes and impaired glucose regulation: systematic review. Diabetes Care. 2013;36:3337–45.
Tafet GE, Nemeroff CB. Pharmacological treatment of anxiety disorders: the role of the HPA axis. Front Psychiatry. 2020;11:443.
Deuschle M. Effects of antidepressants on glucose metabolism and diabetes mellitus type 2 in adults. Curr Opin Psychiatry. 2013;26:60–5.
McIntyre RS, Soczynska JK, Konarski JZ, Kennedy SH. The effect of antidepressants on glucose homeostasis and insulin sensitivity: synthesis and mechanisms. Expert Opin Drug Saf. 2006;5:157–68.
Kotha RR, Luthria DL. Curcumin: biological, pharmaceutical, nutraceutical, and analytical aspects. Molecules. 2019;24:2930.
Al-Karawi D, Al Mamoori DA, Tayyar Y. The role of curcumin administration in patients with major depressive disorder: mini meta-analysis of clinical trials. Phytother Res. 2016;30:175–83.
Lopresti AL, Hood SD, Drummond PD. Multiple antidepressant potential modes of action of curcumin: a review of its anti-inflammatory, monoaminergic, antioxidant, immune-modulating and neuroprotective effects. J Psychopharmacol. 2012;26:1512–24.
Pivari F, Mingione A, Brasacchio C, Soldati L. Curcumin and type 2 diabetes mellitus: prevention and treatment. Nutrients. 2019;11:1837.
Wu LY, Chen CW, Chen LK, Chou HY, Chang CL, Juan CC. Curcumin attenuates adipogenesis by inducing preadipocyte apoptosis and inhibiting adipocyte differentiation. Nutrients. 2019;11:2307.
Mokgalaboni K, Ntamo Y, Ziqubu K, Nyambuya TM, Nkambule BB, Mazibuko-Mbeje SE, et al. Curcumin supplementation improves biomarkers of oxidative stress and inflammation in conditions of obesity, type 2 diabetes and NAFLD: updating the status of clinical evidence. Food Funct. 2021;12:12235–49.
Chuengsamarn S, Rattanamongkolgul S, Luechapudiporn R, Phisalaphong C, Jirawatnotai S. Curcumin extract for prevention of type 2 diabetes. Diabetes Care. 2012;35:2121–7.
Zaheri Z, Fahremand F, Rezvani ME, Karimollah A, Moradi A. Curcumin exerts beneficial role on insulin resistance through modulation of SOCS3 and Rac-1 pathways in type 2 diabetic rats. J Funct Foods. 2019;60. https://doi.org/10.1016/j.jff.2019.103430.
Asadi S, Gholami MS, Siassi F, Qorbani M, Sotoudeh G. Beneficial effects of nano-curcumin supplement on depression and anxiety in diabetic patients with peripheral neuropathy: a randomized, double-blind, placebo-controlled clinical trial. Phytother Res. 2020;34:896–903.
Xu Y, Ku BS, Yao HY, Lin YH, Ma X, Zhang YH, et al. The effects of curcumin on depressive-like behaviors in mice. Eur J Pharmacol. 2005;518:40–6.
Hao F, Kang J, Cao Y, Fan S, Yang H, An Y, et al. Curcumin attenuates palmitate-induced apoptosis in MIN6 pancreatic β-cells through PI3K/Akt/FoxO1 and mitochondrial survival pathways. Apoptosis. 2015;20:1420–32.
Bogdanova OV, Kanekar S, D’Anci KE, Renshaw PF. Factors influencing behavior in the forced swim test. Physiol Behav. 2013;118:227–39.
Lee JW, Chen H, Pullikotil P, Quon MJ. Protein kinase A-alpha directly phosphorylates FoxO1 in vascular endothelial cells to regulate expression of vascular cellular adhesion molecule-1 mRNA. J Biol Chem. 2011;286:6423–32.
Teo AK, Kulkarni RN. Setting sail for glucose homeostasis with the AKAP150-PP2B-anchor. EMBO J. 2012;31:3956–7.
Hinke SA, Navedo MF, Ulman A, Whiting JL, Nygren PJ, Tian G, et al. Anchored phosphatases modulate glucose homeostasis. EMBO J. 2012;31:3991–4004.
Khatlani T, Pradhan S, Da Q, Gushiken FC, Bergeron AL, Langlois KW, et al. The β isoform of the catalytic subunit of protein phosphatase 2B restrains platelet function by suppressing outside-in αII b β3 integrin signaling. J Thromb Haemost. 2014;12:2089–101.
Lester LB, Faux MC, Nauert JB, Scott JD. Targeted protein kinase A and PP-2B regulate insulin secretion through reversible phosphorylation. Endocrinology. 2001;142:1218–27.
Zhang B, Sun P, Shen C, Liu X, Sun J, Li D, et al. Role and mechanism of PI3K/AKT/FoxO1/PDX-1 signaling pathway in functional changes of pancreatic islets in rats after severe burns. Life Sci. 2020;258:118145.
Kikuchi O, Kobayashi M, Amano K, Sasaki T, Kitazumi T, Kim HJ, et al. FoxO1 gain of function in the pancreas causes glucose intolerance, polycystic pancreas, and islet hypervascularization. PLoS One. 2012;7:e32249.
Kitamura T. The role of FOXO1 in β-cell failure and type 2 diabetes mellitus. Nat Rev Endocrinol. 2013;9:615–23.
Wang RH, Xu X, Kim HS, Xiao Z, Deng CX. SIRT1 deacetylates FOXA2 and is critical for Pdx1 transcription and β-cell formation. Int J Biol Sci. 2013;9:934–46.
Kitamura T, Nakae J, Kitamura Y, Kido Y, Biggs WH 3rd, Wright CV, et al. The forkhead transcription factor Foxo1 links insulin signaling to Pdx1 regulation of pancreatic beta cell growth. J Clin Invest. 2002;110:1839–47.
Lorberbaum DS, Sussel L. A Notch in time: spatiotemporal analysis of Notch signaling during pancreas development. Dev Cell. 2020;52:681–2.
Bartolome A, Zhu C, Sussel L, Pajvani UB. Notch signaling dynamically regulates adult β cell proliferation and maturity. J Clin Invest. 2019;129:268–80.
Ren BC, Zhang YF, Liu SS, Cheng XJ, Yang X, Cui XG, et al. Curcumin alleviates oxidative stress and inhibits apoptosis in diabetic cardiomyopathy via Sirt1-Foxo1 and PI3K-Akt signalling pathways. J Cell Mol Med. 2020;24:12355–67.
Chen JW, Kong ZL, Tsai ML, Lo CY, Ho CT, Lai CS. Tetrahydrocurcumin ameliorates free fatty acid-induced hepatic steatosis and improves insulin resistance in HepG2 cells. J Food Drug Anal. 2018;26:1075–85.
Yang H, Yang L. Targeting cAMP/PKA pathway for glycemic control and type 2 diabetes therapy. J Mol Endocrinol. 2016;57:R93–108.
Dyla M, Kjaergaard M. Intrinsic disorder in protein kinase A anchoring proteins signaling complexes. Prog Mol Biol Transl Sci. 2021;183:271–94.
Lester LB, Langeberg LK, Scott JD. Anchoring of protein kinase A facilitates hormone-mediated insulin secretion. Proc Natl Acad Sci USA. 1997;94:14942–7.
Gold MG. Swimming regulations for protein kinase A catalytic subunit. Biochem Soc Trans. 2019;47:1355–66.
Creamer TP. Calcineurin. Cell Commun Signal. 2020;18:137.
Ni Q, Ganesan A, Aye-Han NN, Gao X, Allen MD, Levchenko A, et al. Signaling diversity of PKA achieved via a Ca2+-cAMP-PKA oscillatory circuit. Nat Chem Biol. 2011;7:34–40.
Moita MA, Lamprecht R, Nader K, LeDoux JE. A-kinase anchoring proteins in amygdala are involved in auditory fear memory. Nat Neurosci. 2002;5:837–8.
Antoine MH, Gall D, Schiffmann SN, Lebrun P. Tricyclic antidepressant imipramine reduces the insulin secretory rate in islet cells of Wistar albino rats through a calcium antagonistic action. Diabetologia. 2004;47:909–16.
Lee JY, Lee S, Choi JH, Na K. ι-Carrageenan nanocomposites for enhanced stability and oral bioavailability of curcumin. Biomater Res. 2021;25:32.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 92168120, 81974506, 81673486 and 81373405 to Lu Tie, No. 82073878, 81020108031 and 81874318 to Xue-jun Li), and the Beijing Natural Science Foundation (No. Z200019 and 7172119) to Lu Tie.
Author information
Authors and Affiliations
Contributions
The work presented was performed in collaboration by all authors. MH, JYC, and YH designed and performed the experiments, analyzed the data, and wrote the manuscript. KC, FH, JSK, and YP performed the experiments. LT and XJL designed the research and supervised the study. MH, JYC, YH, LT, and XJL revised the concept, designed the research, supervised the study, and wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, M., Cai, Jy., He, Y. et al. Protective effects of curcumin on desipramine-induced islet β-cell damage via AKAP150/PKA/PP2B complex. Acta Pharmacol Sin 45, 327–338 (2024). https://doi.org/10.1038/s41401-023-01176-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-023-01176-6