Abstract
There were several studies about the psychiatric and mental health issues related to the severe adult respiratory syndrome (SARS) outbreak in 2003, however, the association between SARS and the overall risk of psychiatric disorders and suicides has, as yet, to be studied in Taiwan. The aim of this study is to examine as to whether SARS is associated with the risk of psychiatric disorders and suicide. A total of 285 patients with SARS and 2850 controls without SARS (1:10) matched for sex, age, insurance premium, comorbidities, residential regions, level of medical care, and index date were selected between February 25 and June 15, 2003 from the Inpatient Database Taiwan’s National Health Insurance Research Database. During the 12-year follow-up, in which 79 in the SARS cohort and 340 in the control group developed psychiatric disorders or suicide (4047.41 vs. 1535.32 per 100,000 person-years). Fine and Gray’s survival analysis revealed that the SARS cohort was associated with an increased risk of psychiatric disorders and suicide, and the adjusted subdistribution HR (sHR) was 2.805 (95% CI: 2.182–3.605, p < 0.001) for psychiatric disorders and suicide. The SARS cohort was associated with anxiety, depression, sleep disorders, posttraumatic stress disorder/acute stress disorder (PTSD/ASD), and suicide. The sensitivity analysis revealed that the SARS group was associated with anxiety, depression, sleep disorders, PTSD/ASD, and suicide after the individuals with a diagnosis of psychiatric disorders and suicide were excluded within the first year, and with anxiety, depression, and sleep disorders, while those in the first five years were excluded. In conclusion, SARS was associated with the increased risk of psychiatric disorders and suicide.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) outbreak not only causes deaths and adverse consequences on the physical health1,2, but also induces a global mental health crisis, including psychiatric morbidity and suicide, in the patients, the health care professionals, and the general population3,4,5. In the meantime, in May 2020, the COVID-19 pandemic seems not, as yet, to be ameliorated6. It is too early to reach a conclusion about the overall impact on the mental health in the country or global levels from the limited empirical data. There are several differences between COVID-19 and severe adult respiratory syndrome (SARS) in the death rates and range of transmission rates1, for example, in regard of the case numbers, SARS was just not comparable to COVID-19. Furthermore, the complexities of COVID-19, such as variety of symptoms, multiple organ involvements have not been seen in SARS. On the other hand, the severe sequela in SARS patients, especially the lung fibrosis, may be not common in COVID-196,7. However, they are similar in several ways: First, they were caused by two similar, but different, coronaviruses. Second, the infections have caused the large-scale influences in society8,9. Since the understanding of the mental health issues are urgent, we believe that we could learn some experiences from the SARS-related mental health issues, including the psychiatric disorders and suicide.
An outbreak of SARS caused by a novel coronavirus severely affected Taiwan in 200310, and the first confirmed diagnosis of SARS was on February 25, 2003, and the last diagnosis on June 15, 2003. Through this endemic outbreak, there were 346 patients diagnosed with SARS and 37 died among these patients7 and there were also SARS outbreaks in China, Singapore, and Toronto, Canada, at about the same time7. There were several studies about the psychiatric and mental health issues related to this SARS outbreak. One report from Taiwan of about 10 cases has found that most of the psychiatric diagnoses in the consultation services were adjustments disorder, organic hallucinosis, and organic manic disorder during the acute phase treatment11. In a Hong Kong study, the post-SARS cumulative incidence of psychiatric disorders was 58.9% in a cohort with 90 patients, and the prevalence of psychiatric disorders at 30 months after the SARS was 33.3%, in which one-fourth of the patients had post-traumatic stress disorder (PTSD), and 15.6% had a depressive disorder12. One meta-analysis, combining the studies about SARS, Middle East Respiratory Syndrome (MERS), and COVID-19, has indicated that, in the post-illness stage, the point prevalence of PTSD was 32.2% (95% Confidence Interval [CI]: 23.7–42.0), that of depression was 14·9% (95% CI: 12.1–18.2), and that of anxiety disorders was 14.8% (95% CI 11.1–19.4)13. Other studies about SARS-related mental health issues were conducted in the doctors14, nurses14,15,16, and overall hospital workers17. In addition, even though several studies have warned of a potential rise of suicides in the COVID-1918,19, there were limited reports on the topic of post-SARS suicides20,21. Therefore, a nationwide, population-based, long-term study on the topic for psychiatric disorders and suicides for the patients with SARS is yet to be conducted.
Apart from the psychosocial stressors related to SARS or COVID-1922,23, the cytokine storms and other immunological factors might also contribute to the post-infection psychiatric morbidity24. In addition, the long-term adverse health outcomes for the SARS survivors could also be a risk factor for the psychiatric morbidity25. Therefore, we hypothesized that SARS is associated with an increased risk in the development of psychiatric disorders and suicide, and we conducted this nationwide, population-based, cohort study so as to investigate the association between SARS and the psychiatric disorders and suicide, using the National Health Insurance Research Database (NHIRD), a claims database retrieved from the whole population of Taiwan.
Methods
Data sources
The National health insurance (NHI) Program is a mandatory and universal health insurance program in Taiwan, which has been has been operative since 1995, that covered contracts with 97% of the medical providers with approximately 23 million beneficiaries, or more than 99% of the population26. The details of this program were documented in several previous studies27,28,29,30,31,32,33,34,35,36,37. The NHIRD contains comprehensive and detailed data regarding the total outpatients and inpatients. An Inpatient Dataset in 2000–2015 was selected from the NHIRD, with individual diagnoses coded by the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM).
Ethics
This study was conducted in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki). The Institutional Review Board of the Tri-Service General Hospital approved this study and waived the need of individual consents since all the identification data were encrypted in the NHIRD (IRB: TSGHIRB No. B-109–14).
Study design and sampled participants
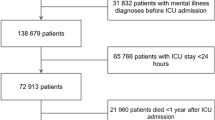
This is a retrospective matched-cohort research using the Inpatient Dataset between January 1, 2000, and December 31, 2015. Each patient with SARS was required to receive a diagnosis in an inpatient setting with the ICD codes as 480.8 and 480.9. A 1:10 sex-matched, age-matched, insurance premium-matched, comorbidities-matched, location-matched, level of care-matched, and index date-matched controls were randomly selected for each patient with SARS. The exclusion criteria for the cohorts were with unknown sex and individuals diagnosed with psychiatric disorders or pneumonia and influenza (ICD-9-CM codes: 480–488) before the index date. The index date was defined as the time when the individuals were first diagnosed as SARS within the one-year study period (Fig. 1).
Outcomes
All of the SARS participants and controls were followed from the index date until the onset of psychiatric disorders, including anxiety disorders, depression, bipolar disorders, sleep disorders, PTSD, eating disorders, substance use related disorder, dementia, psychotic disorders, and suicide, death, withdrawal from the NHI program, or the end of 2015. The ICD codes of psychiatric disorders and suicide are as listed in Table S1. In Taiwan, the clinical diagnosis of psychiatric disorders must conform to the criteria from the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV), or the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV-TR) and confirmed by a board-certificated psychiatrist.
Covariates
The covariates include sociodemographic characteristics and comorbidities. Sociodemographic characteristics included sex, age (18–44, 45–64, ≧65 years), education (<12 years; ≧12 years), monthly insured premiums, urbanization levels, regions of residence, and levels of medical care. The monthly insured premiums have been divided into three categories in New Taiwan Dollars [NT$]: <18,000, 18,000–34,999, ≥35,000. The urbanization level was defined by population and certain indicators of the city’s level of development. Level 1 urbanization was defined as having a population greater than 1,250,000 people. Level 2 urbanization was defined as having a population between 500,000 and 1,250,000. Urbanization levels 3 and 4 were defined as having a population between 150,000 and 500,000 and less than 150,000, respectively38. The Charlson comorbidity index (CCI) is one of the most widely used comorbidity indexs39,40, which consists of 22 conditions41, including myocardial infarction, congestive heart failure, peripheral vascular disease, dementia, cerebrovascular disease, chronic lung disease, connective tissue disease, ulcer, chronic liver disease, diabetes, hemiplegia, moderate or severe kidney disease, diabetes with end organ damage, tumor, leukemia, lymphoma, moderate or severe liver disease, malignant tumor, metastasis, and acquired immune deficiency syndrome (AIDS). We used the CCI to quantify the comorbidities since it could predict the in-hospital mortality or outcome in patients with severe adults respiratory infection (SARI) and other infections42,43,44.
Statistical analysis
The SPSS software version 22 (SPSS Inc., Chicago, Illinois, USA) was used to conduct the statistical analyses. The Pearson chi-square test was used for the analysis of the categorical data. Continuous variables presented as the mean (±SD), were analyzed using the two-sample t test. To investigate the risk of psychiatric disorders and suicide for patients with and without SARS, the Fine and Gray’s model was used to conduct the competing risk analysis to calculate the subdistribution hazard ratios (sHRs) and 95% confidence intervals (CIs), adjusting for sociodemographic characteristics, and comorbidities. The Value-added module, including the Competing Risks Survival Analysis, in the SPSS was used to conduct Fine and Gray’s survival analysis (https://www.asiaanalytics.com.tw/en/product/p-asia-analytics-2.jsp). The Kaplan–Meier method was used to determine the difference in the risk of psychiatric disorders and suicide for the patients with SARS and the control cohorts using the log-rank test. A p value < 0.05 was considered statistically significant.
Results
Study cohort characteristics
Table 1 shows the sex, age, education, monthly insured premiums, urbanization levels, regions of residence, comorbidities, and levels of medical care in the patients with or without SARS. When compared to the controls, patients with SARS have had no significant difference in the covariates.
Kaplan–Meier curves for the cumulative incidence of psychiatric disorders in patients with psychiatric disorders and suicide
In total, 285 patients were diagnosed with SARS during the study period. During the follow-up period, 79 in the SARS group (N = 285) and 340 in the control group (N = 2850) developed psychiatric disorders or suicide (4047.41 vs. 1535.32 per 100,000 person-years). Figure 2 reveals that the difference between the two cohorts in the psychiatric disorders and suicide were significant (long-rank test, p < 0.001).
Years from SARS to psychiatric disorders and suicide
The mean time from the index date to the diagnosis of psychiatric disorders and suicide after diagnosis was 3.54 (SD = 3.26) years. The mean years to the developed psychiatric disorders and suicide in patients with SARS were 3.42 (SD = 2.80) years, which was earlier than patients without SARS (3.57 [SD = 3.36] years) (Table S2).
Subdistribution hazard ratio analysis of psychiatric disorders and suicide in the patients with SARS
Table 2 shows the factors of SARS, using Fine and Gray’s survival analysis, of the factors associated with the risk of psychiatric disorders and suicide. The crude sHR was 2.785 (95% CI: 2.136–3.527, p < 0.001), and after adjusting for sex, age, education, monthly insured premiums, urbanization levels, regions of residence, comorbidities, and levels of medical care, the adjusted sHR was 2.805 (95% CI: 2.182–3.605, p < 0.001) for psychiatric disorders and suicide. SARS patients aged 45–64 years, ≧65 years, with the CCI score ≧2, and care from the medical centers and regional hospitals, were associated with an increased risk for psychiatric disorders and suicide. Male patients with SARS were associated with a decreased risk for psychiatric disorders and suicide, in comparison to the female patients.
Subgroup analysis of psychiatric disorders and suicide in the SARS cohort and controls
Table S3 shows that the SARS cohort was associated with a higher risk of psychiatric disorders than the control group, regardless of sex, age, marital status, education years, comorbidities, monthly insured premiums, residences, urbanization, and levels of care, with one exception being the insured premiums of ≧NT$ 35,000.
Sensitivity test for analysis of the risk of psychiatric disorders and suicide in the patients with SARS
Patients with SARS were associated with an increased risk in overall psychiatric disorders, anxiety disorders, depressive disorders, sleep disorders, PTSD, and suicide, when compared to the control group. The sHR’s of these psychiatric disorders were: anxiety disorder 3.172 (95% CI:2.471–4.089, p < 0.001), depressive disorder 3.165 (95% CI:2.465–4.077, p < 0.001), sleep disorder 2.411 (95% CI:1.098–3.172, p = 0.001), PTSD/ASD 60.360 (95% CI:49.121–77.602, p < 0.001), and suicide 4.382 (95% CI:3.401–5.513, p < 0.001). The sensitivity analysis revealed that the SARS cohort was associated with anxiety, depression, sleep disorders, PTSD/ASD, and suicide after the individuals with a diagnosis of psychiatric disorders and suicide were excluded within the first year, and with anxiety, depression, and sleep disorders, while those in the first five years were excluded (Table 3).
Discussion
In this study, we have several noteworthy findings: First, the SARS cohort had a 2.8-fold increased risk of overall psychiatric disorders when compared to the control cohort. Compared with previous reports about the association between SARS and psychiatric disorders, such as a case series11, or a smaller sample size study12, this study was based on a nationwide, population-based claims database, with a larger sample size, in a long-duration follow-up. Even though one meta-analysis, combining SARS, MERS, and COVID-19 studies, has been comprised of 1991 cases of acute phase SARS13, this study has a longer follow-up for the risk of developing psychiatric disorders. To the best of our knowledge, this is the first study on the association between SARS and increased risk in developing psychiatric disorders and suicide, in a 12-year follow-up, from a nationwide, population-based database.
Second, we investigated the risk of different psychiatric diagnoses in the SARS patients, and we found that SARS was associated with anxiety, depression, sleep disorders, PTSD/ASD, and suicide, which is similar to the findings of the association between severe coronavirus infections and PTSD12,13, anxiety13, and depressive disorders12,13. However, we found that the risk of psychiatric disorders could be increased even in a long term follow-up of 12 years, not just a shorter term of up to 30-month of follow-up12, in this study.
Third, to resolve the influences of protopathic bias, we conducted the sensitivity analysis: the SARS cohort was associated with anxiety, depression, sleep disorders, PTSD/ASD, and suicide after the individuals with a diagnosis of psychiatric disorders and suicide were excluded within the first year, and with anxiety, depression, and sleep disorders, while those in the first five years were excluded. By conducting this analysis, we could avoid the protopathic bias, that arises when the initiation of the exposure occurs in response to an undiagnosed disease under study outcome45.
Fourth, in this study, we could also point out that the risk of development of PSTD was not beyond the first five years. In addition, the mean years to developed psychiatric disorders and suicide in patients with SARS were 3.42 (SD = 2.80) years. Therefore, this finding could serve as an important reminder for the clinicians caring the SARS survivors in monitoring their mental conditions in the first 3–4 years, especially for PTSD/ASD. Furthermore, we found that the SARS cohort was at a particularly high risk of PTSD/ASD: the SARS cohort had a 60-fold increased risk of PTSD/ASD and a 50-fold increased risk of PTSD/ASD even after excluding the psychiatric disorders within the first year. This finding is similar to several studies on the topic of the association between severe coronavirus infections and PTSD, up to one-third to one-fourth of the patients of the severe coronavirus infections12,13.
Fifth, suicide after the SARS outbreak was a critical issue, and previous studies on this topic have investigated the potential increased suicide risk in the elderly20,46 and the ED visitors21, during and after the SARS outbreak. This study might be the first study about the suicides of the SARS survivors. As aforementioned, the association between SARS and suicide was statistically significant even after excluding suicide within the first year, but not significant after excluding suicide within the first five years. Therefore, the careful evaluation in the suicide risk is important in the following years after SARS.
The underlying mechanisms for the risk of psychiatric disorders remained unclear. One of the possible reasons for the increased risk of psychiatric disorders and suicide might well be related to the psychological impact for the patients, general stress, and the negative psychological effects are increased in the SARS patients, particularly among the infected health care workers47,48, such as stress from the quarantine and isolation, fear of uncertainty and death, impaired health after severe viral infections, economic burden after SARS, and even negative feelings for the SARS-related information48,49,50.
Furthermore, one previous study found that the elevated levels of the monocyte chemoattractant protein-1 (MCP-1), transforming growth factor beta-1 (TGFβ-1), interleukin-1 beta (IL-1 β), and interleukin-6 (IL-6) in the SARS-CoV-infected angiotensin-converting enzyme 2 (ACE2+) Cells in the SARS patients51. The increased levels of these cytokine might not only result in acute lung injury, but also be associated with psychiatric disorders, such as depressive disorders, bipolar, or anxiety disorders52,53. In this study, patients aged 45–64 years or ≧65 years, and a higher CCI score of ≧2, and the level of care from the medical centers and regional hospitals, were associated with the risk of psychiatric disorders and suicide. This finding hints that patients with older ages, and more severe physical morbidities in the SARS patients, could also contribute to the risk of psychiatric disorders. Nonetheless, further studies are needed to investigate the underlying mechanisms for the development of psychiatric disorders in the SARS survivors.
Strengths of this study
This study has several strengths: First, we used the LHID, which has a large sample size in this study. Second, SARS was diagnosed by the serology test and being a notifiable disease it needed to be reported to the Health authority in Taiwan (https://www.cdc.gov.tw/En), Third, we have conducted a long-term follow-up of 12 years of the development of psychiatric disorders after the SARS outbreak in 2003. This could serve as a lesson for us to learn from SARS when facing the challenge of psychiatric disorders from COVID-19: The mental health issues in COVID-19 might not be only from the acute-phase of delirium54,55, depression, and acute trauma-related psychiatric disorders such as ASD or acute PTSD56. A long-term follow-up of psychiatric disorders for COVID-19 survivors would be important.
Limitations of this study
This study has several limitations that warrant consideration. First, similar to previous studies using the NHIRD on infectious, parasitic, or inflammatory diseases57,58,59,60,61, since the severity, weakness severity, laboratory parameters, or lung function examinations in SARS patients were not recorded in the NHIRD. Second, other factors, such as genetic, psychosocial, and environmental factors, were not included in the dataset. Third, ascertainment bias is possible if the patients who were treated for SARS were more medically attentive so that they also sought treatment for psychiatric conditions. Fourth, this study contained only small number of cases, and thus there are very few numbers of PTSD and suicide, which all happened within five years after SARS. Furthermore, for other psychiatric cases, nearly one third of the cases happened within one year, and up to two thirds reported with five years both in the SARS and control cohorts, only one occurred after ten years in SARS group (Table 2). Considering the new occurrence of psychiatric disorders, the difference was not so significant between two cohorts after nine years in the study period. Therefore, most of the attention should be paid to psychiatric disorders that developed within ten years of the onset of SARS. After all, the small numbers of SARS cases limit the generalization of the SARS experiences to the diagnosis and treatment of psychiatric consequences of COVID-19 treatment. Finally, the NHIRD does not contain the information for the SARS patients’ family members and the health workers who take care of them. We need further studies to investigate the post-SARS psychiatric morbidity in the long-term follow-up.
Conclusion
This study found that SARS was associated with the increased risk of psychiatric disorders and suicide in a long-term follow-up study of 12 years. This is also a reminder for the clinicians that psychiatric morbidity is an important issue in the patients with severe coronavirus infections, such as COVID-19.
Data availability
Data are available from the National Health Insurance Research Database (NHIRD) published by the Taiwan National Health Insurance (NHI) Administration. Due to legal restrictions imposed by the government of Taiwan in relation to the “Personal Information Protection Act”, data cannot be made publicly available. Requests for data can be sent as a formal proposal to the NHIRD (https://dep.mohw.gov.tw/dos/np-2497-113.html).
References
Baloch, S., Baloch, M. A., Zheng, T. & Pei, X. The Coronavirus Disease 2019 (COVID-19) Pandemic. Tohoku J. Exp. Med. 250, 271–278 (2020).
Taiwan Centers for Disease Control. COVID-19. 2020, (2020).
Franic, T. & Dodig-Curkovic, K. Covid-19, Child and adolescent mental health-croatian (in)experience. Irish J. Psychol. Med. 21, 1–4, https://doi.org/10.1017/ipm.2020.55. Epub ahead of print. (2020).
McKay, D., Yang, H., Elhai, J. & Asmundson, G. J. G. Anxiety regarding contracting COVID-19 related to interoceptive anxiety sensations: the moderating role of disgust propensity and sensitivity. J. Anxiety Disord. 73, 102233 (2020).
Pappa, S. et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immunity (2020).
World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. 2020, (2020).
World Health Organization. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. 2020, (2003).
Qiu, W., Chu, C., Mao, A. & Wu, J. The impacts on health, society, and economy of SARS and H7N9 outbreaks in China: a case comparison study. J. Environ. Public Health 2018, 2710185 (2018).
Chakraborty, I. & Maity, P. COVID-19 outbreak: migration, effects on society, global environment and prevention. Sci. Total Environ. 728, 138882 (2020).
Taiwan Centers for Disease Control. Severe Acute Respiratory Symdrome (SARS). (2020).
Cheng, S. K., Tsang, J. S., Ku, K. H., Wong, C. W. & Ng, Y. K. Psychiatric complications in patients with severe acute respiratory syndrome (SARS) during the acute treatment phase: a series of 10 cases. Br. J. Psychiatry. 184, 359–360 (2004).
Mak, I. W., Chu, C. M., Pan, P. C., Yiu, M. G. & Chan, V. L. Long-term psychiatric morbidities among SARS survivors. Gen. Hospital Psychiatry 31, 318–326 (2009).
Rogers, J. P. et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 7, 611–627 (2020).
Tham, K. Y. et al. Psychiatric morbidity among emergency department doctors and nurses after the SARS outbreak. Ann. Acad. Med., Singap. 33, S78–S79 (2004).
Lee, S. H. et al. Facing SARS: psychological impacts on SARS team nurses and psychiatric services in a Taiwan general hospital. Gen. Hospital Psychiatry 27, 352–358 (2005).
Su, T. P. et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J. Psychiatr. Res. 41, 119–130 (2007).
Lancee, W. J., Maunder, R. G. & Goldbloom, D. S. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr. Serv. 59, 91–95 (2008).
Devitt, P. Can We Expect an Increased Suicide Rate Due to Covid-19? Irish J. Psychol. Med. 1–15 (2020).
Hughes, H., Macken, M., Butler, J. & Synnott, K. Uncomfortably numb: suicide and the psychological undercurrent of COVID-19. Irish J. Psychol. Med. 1–7 (2020).
Chan, S. M., Chiu, F. K., Lam, C. W., Leung, P. Y. & Conwell, Y. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int. J. Geriatr. Psychiatry 21, 113–118 (2006).
Huang, C. C. et al. Impact of severe acute respiratory syndrome (SARS) outbreaks on the use of emergency department medical resources. J. Chin. Med. Assoc. 68, 254–259 (2005).
Lee, D. T. et al. Factors associated with psychosis among patients with severe acute respiratory syndrome: a case-control study. Clin. Infect. Dis. 39, 1247–1249 (2004).
Phua, D. H., Tang, H. K. & Tham, K. Y. Coping responses of emergency physicians and nurses to the 2003 severe acute respiratory syndrome outbreak. Academic Emerg. Med. 12, 322–328 (2005).
Serrano-Castro, P. J. et al. Impact of SARS-CoV-2 infection on neurodegenerative and neuropsychiatric diseases: a delayed pandemic? Neurología (English Edition) (2020).
Maunder, R. G. et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 12, 1924–1932 (2006).
Ho Chan, W. S. Taiwan’s healthcare report 2010. EPMA J. 1, 563–585 (2010).
Chien, W. C. et al. Is weight control surgery associated with increased risk of newly onset psychiatric disorders? A population-based, matched cohort study in Taiwan. J. Med. Sci. 37, 137 (2017).
Chen, T. Y. et al. Sex and age differences in the association between anxiety disorders and narcolepsy: a nationwide population-based case control study. J. Affect. Disord. 264, 130–137 (2020).
Lin, C. H. et al. Increased risk of dementia in patients with genital warts: a nationwide cohort study in Taiwan. J. Dermatol. 47, 503–511 (2020).
Lin, Y. C. et al. Stimulants associated with reduced risk of hospitalization for motor vehicle accident injury in patients with obstructive sleep apnea-a nationwide cohort study. BMC Pulm. Med. 20, 28 (2020).
Liu, Y. P. et al. Are Anticholinergic medications associated with increased risk of dementia and behavioral and psychological symptoms of dementia? A nationwide 15-year follow-up cohort study in Taiwan. Front. Pharmacol. 11, 30 (2020).
Wan, F. J., Chien, W. C., Chung, C. H., Yang, Y. J. & Tzeng, N. S. Association between traumatic spinal cord injury and affective and other psychiatric disorders-A nationwide cohort study and effects of rehabilitation therapies. J. Affect. Disord. 265, 381–388 (2020).
Wang, D. S. et al. Association between child abuse exposure and the risk of psychiatric disorders: a nationwide cohort study in Taiwan. Child Abus. Negl. 101, 104362 (2020).
Yang, C. C. et al. No association between human immunodeficiency virus infections and dementia: a nationwide cohort study In Taiwan. Neuropsychiatr. Dis. Treat. 15, 3155–3166 (2019).
Yeh, T. C. et al. Psychiatric disorders after traumatic brain injury: a nationwide population-based cohort study and the effects of rehabilitation therapies. Arch. Phys. Med. Rehabilitat. 101, 822–831 (2020).
Kao, L. C. et al. The newly diagnosed amnestic disorders and dementia: a nationwide, cohort study in Taiwan. Taiwan. J. Psychiatry 32, 18–28 (2018).
Chiou, Y. E. et al. New users of herbal medicine containing aristolochic acids and the risk of dementia in the elderly-a nationwide, population-based study in Taiwan. Neuropsy. Dis. Treat. 16, 1493–1504, https://doi.org/10.2147/NDTS250659 (2020).
Chang, C. Y. et al. Increased risk of major depression in the three years following a femoral neck fracture–a national population-based follow-up study. PLoS ONE 9, e89867 (2014).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 40, 373–383 (1987).
de Groot, V., Beckerman, H., Lankhorst, G. J. & Bouter, L. M. How to measure comorbidity. a critical review of available methods. J. Clin. Epidemiol. 56, 221–229 (2003).
Charlson, M., Szatrowski, T. P., Peterson, J. & Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 47, 1245–1251 (1994).
Ternavasio-de la Vega, H. G. et al. The updated Charlson comorbidity index is a useful predictor of mortality in patients with Staphylococcus aureus bacteraemia. Epidemiol. Infect. 146, 2122–2130 (2018).
Baiomi, A. et al. Charlson Comorbidity Index (CCI): an independent predictor of outcomes in Clostridium difficile Infection (CDI): 2743. Am. J. Gastroenterol. 113, S1525 (2018).
Setter, W. et al. 2209 Charlson comorbidity index scores and in-hospital prognosis in severe acute respiratory infections patients. Open Forum Infect. Dis. 6, S753–S753 (2019).
Horwitz, R. I. & Feinstein, A. R. The problem of “protopathic bias” in case-control studies. Am. J. Med. 68, 255–258 (1980).
Cheung, Y. T., Chau, P. H. & Yip, P. S. A revisit on older adults suicides and Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong. Int. J. Geriatr. Psychiatry 23, 1231–1238 (2008).
Chua, S. E. et al. Stress and psychological impact on SARS patients during the outbreak. Can. J. Psychiatry Rev. Canadienne de. Psychiatr. 49, 385–390 (2004).
Tsang, H. W., Scudds, R. J. & Chan, E. Y. Psychosocial impact of SARS. Emerg. Infect. Dis. 10, 1326–1327 (2004).
Sim, K. & Chua, H. C. The psychological impact of SARS: a matter of heart and mind. CMAJ 170, 811–812 (2004).
Sin, S. S. & Huak, C. Y. Psychological impact of the SARS outbreak on a Singaporean rehabilitation department. Int. J. Ther. Rehab. 11, 417–424 (2004).
He, L. et al. Expression of elevated levels of pro-inflammatory cytokines in SARS-CoV-infected ACE2+ cells in SARS patients: relation to the acute lung injury and pathogenesis of SARS. J. Pathol. 210, 288–297 (2006).
Kohler, C. A. et al. Peripheral alterations in cytokine and chemokine levels after antidepressant drug treatment for major depressive disorder: systematic review and meta-analysis. Mol. Neurobiol. 55, 4195–4206 (2017).
Rosenblat, J. D. & McIntyre, R. S. Bipolar disorder and immune dysfunction: epidemiological findings, proposed pathophysiology and clinical implications. Brain Sci 7, 144 (2017).
Ahmad, I. & Rathore, F. A. Neurological manifestations and complications of COVID-19: a literature review. J. Clin. Neurosci. 77, 8–12, https://doi.org/10.1016/j.jocn.2020.05.017 (2020). Epub 2020 May 6.
Kotfis, K. et al. COVID-19: ICU delirium management during SARS-CoV-2 pandemic. Crit. Care 24, 176 (2020).
Troyer, E. A., Kohn, J. N. & Hong, S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav. Immunity. S0889-1591(0820)30489-X (2020).
Tzeng, N. S. et al. Anti-herpetic medications and reduced risk of dementia in patients with herpes simplex virus infections-a nationwide, population-based cohort study in Taiwan. NeuroTherapeut. 15, 417–429 (2018).
Hsu, R. J. et al. The association between scabies and myasthenia gravis: a nationwide population-based cohort study. J. Clin. Neurosci. 45, 115–120 (2017).
Lin, C. Y. et al. Increased risk of bipolar disorder in patients with scabies: a nationwide population-based matched-cohort study. Psychiatry Res. 257, 14–20 (2017).
Tzeng, N. S. et al. Increased risk of psychiatric disorders in allergic diseases: a nationwide, population-based, cohort study. Front. Psychiatry 9, 133 (2018).
Tzeng, N. S. et al. Are chronic periodontitis and gingivitis associated with dementia? A nationwide, retrospective, matched-cohort study in Taiwan. Neuroepidemiology 47, 82–93 (2016).
Acknowledgements
The authors would like to thank the Medical Affairs Bureau, the Ministry of Defense of Taiwan (MAB-107-084), and the Tri-Service General Hospital Research Foundation (TSGH-C108-003, TSGHC108-027, TSGH-C108-151, and TSGH-B-109-010). These funding agencies did not influence the study design, data collection and analysis, decision to publish, or preparation of the manuscript. We also appreciate Taiwan’s Health and Welfare Data Science Center and Ministry of Health and Welfare (HWDC, MOHW) for providing the National Health Research Database.
Author information
Authors and Affiliations
Contributions
N.-S.T., C.-H.C., C.-C.C., H.-A.C., Y.-C.K., S.-Y.C., and W.-C.C. contributed to the interpretation of the data/critical revision of the manuscript. All authors have no significant financial interest/other relationship to disclose.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tzeng, NS., Chung, CH., Chang, CC. et al. What could we learn from SARS when facing the mental health issues related to the COVID-19 outbreak? A nationwide cohort study in Taiwan. Transl Psychiatry 10, 339 (2020). https://doi.org/10.1038/s41398-020-01021-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-020-01021-y
This article is cited by
-
Evaluation of healthcare-related factors influencing mental health of Taiwanese citizens among different age groups
Scientific Reports (2024)
-
Psychıatrıc dısorders among chıldren and adolescents suffered from COVID-19 ınfectıon
Middle East Current Psychiatry (2023)
-
Risk and protective factors associated with mental health status in an Italian sample of students during the fourth wave of COVID-19 pandemic
Child and Adolescent Psychiatry and Mental Health (2023)
-
COVID-19-associated PTSD in the elderly—lessons learned for the next global pandemic
Middle East Current Psychiatry (2021)