Abstract
Study Design
We investigated whether overnight ES is a feasible method to activate gluteal, quadriceps, and hamstrings muscles in a two-week experiment. Electrical stimulation (ES) induced muscle contractions have proven positive effects on risk factors for developing pressure ulcers in people with a spinal cord injury (SCI). Therefore prolonged overnight ES-induced muscle activation is interesting, but has never been studied.
Objective
To study feasibility of ES-induced leg muscle activation. In eight participants with motor complete SCI gluteal, hamstrings and quadriceps muscles were activated with a 2-weeks overnight stimulation protocol, 8 h per night, using specially developed ES-shorts.
Setting
The Netherlands.
Methods
Muscle fatigue was determined with a muscle contraction sensor. Questionnaires on sleep quality (SQ) and the ES-shorts usability were taken.
Results
After 8 h of activation muscles still contracted, although fatigue occurred, and mean contraction size was lower at the end of a cycle (p = 0.03). SQ (0–100) after intervention was 75, and 66 after 4 weeks without overnight ES (p = 0.04) indicating ES improves sleep quality. The usability of the ES-shorts was good.
Conclusions
This study shows that overnight ES-induced muscle activation using ES-shorts in SCI is a new, feasible method that does not interfere with sleep. The nightly use of the ES-shorts might be considered as an important part of the daily routine in SCI.
Similar content being viewed by others
Introduction
People with spinal cord injury (SCI) face several secondary physical problems such as pressure ulcers (PUs) [1]. PUs occur in up to ~80% of all people with SCI [2, 3]. PUs, in particular deep tissue injury at the buttocks, or more specifically at the ischial tuberosities, increase the incidence of re-hospitalization and disability and cause a great decrease in quality of life [4]. As a result, ~25% of the total health care costs in individuals with SCI can be attributed to PUs [5]. Thus, it is of utmost importance to prevent PUs to maintain quality of life in persons with SCI and reduce costs.
Continuous pressure under the buttocks, caused by inactivity and insufficient weight shifting when sitting, muscle atrophy, loss of sensation, ischemia, and decreased subcutaneous oxygenation in the gluteal muscle are important factors contributing to reduced tissue viability and breakdown due to pressure and shear forces [6,7,8,9,10,11,12]. Measures to prevent PUs, such as wheelchair cushions and instructions to lift and shift weight frequently [13], are insufficient as these wounds still occur. Electrical stimulation (ES) induced contractions of paralyzed gluteal and hamstrings muscles have been found to decrease seating pressure, increase muscle mass [14, 15], and enhance blood flow [16,17,18,19]. Therefore, ES seems to be a promising prophylactic aid in PU management.
Although studies on effects of ES have shown positive results, these studies have not translated into widespread clinical practice. It is interesting to study if ES can be made easier to use in daily medical care. If ES could be made more practical to use, this might not only facilitate ES use in clinical practice, but also enable more high-quality studies to follow. A practical solution to the application problem of how to use ES was recently presented in a study by Smit et al. [20] showing the effects of ES on short-term interface pressure using electrical-stimulation shorts (ES-shorts®) [20, 21]. The electrodes are integrated into the shorts and automatically align over the skin; therefore, the gluteal and hamstring muscles are non-invasively activated. Participants in the latter study indicated that they were satisfied with the ES-shorts and were willing to use the shorts in the future if positive effects were found.
The ES-shorts have not yet been tested for extended stimulation protocols, lasting longer than 3 h, and only acute effects have been studied. One possible problem might be that muscles will stop contracting after prolonged ES-induced activation, due to loss of adequate contact between electrodes and skin or due to muscle fatigue. In addition the use of loose electrodes or ES shorts while sitting demands additional transfers which is undesirable as transfers generate high pressure on the gleno-humeral joint, possibly resulting in shoulder complaints or injuries [22]. ES shorts are also difficult to wear under clothes in a wheelchair; therefore, we believed the ES-shorts would be easier to use overnight. In the present study we investigated whether overnight ES is a feasible method to activate the gluteal, quadriceps and hamstrings muscles. The aims of this feasibility study were:
-
(1)
To evaluate whether ES still results in muscle contractions after 8 h.
-
(2)
To study if overnight ES-induced leg muscle activation disturbs sleep.
-
(3)
To evaluate if the specially designed ES-shorts are user friendly and can be safely used in bed.
We hypothesized based on our previous studies and experience with the ES-shorts [20, 21], that overnight ES-induced muscle activation, with use of the ES-shorts, is a user-friendly, feasible method that does not interfere with sleep, and that muscle activation is possible for an 8-h period if sufficient rest in between the activation periods is allowed.
Methods
Participants
Eight persons with SCI having a motor complete lesion (ASIA Impairment Scale A or B) and aged between 30 and 57 years participated in this study which was approved by the local medical ethics committee. Characteristics of these individuals are shown in Table 1. One physician evaluated all the participants to confirm gluteal and hamstring muscles, skin under the buttocks, and spinal reflexes were intact. Previous (plastic) surgery under the buttock area was not a criterion for exclusion. Individuals with flaccid paralysis, areflexia, a history of severe autonomic dysreflexia, current PUs under the ischial tuberosities, severe cognitive or communicative disorders, or intolerance for ES were excluded. All participants provided written informed consent.
Study design
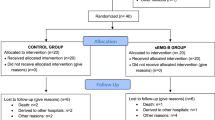
One week before the intervention, participants were fitted with customized ES-shorts® (Axiobionics, Ann Arbor, MI, USA). Instructions were provided through demonstration and an instruction booklet on how to use and maintain the ES-shorts, and on how to determine if the muscles contracted as a reaction on the electrical stimulation. The individual stimulation protocol was then determined. Participants followed a two-week, seven nights-a-week, ES protocol at home. The stimulation program automatically ended eight hours after starting; however, participants were allowed and able to stop the ES before the stimulation protocol completed if necessary. Prior to the 2 week protocol, muscle strength was measured. Directly after the ES intervention, two questionnaires on sleep quality and one on usability were administered. Four weeks after the ES intervention ended, these questionnaires were again administered to measure sleep quality without overnight ES. See Fig. 1 for the time schedule of this study.
Electrical stimulation with the ES shorts
A portable electrical stimulator (Neuro Pro 8 channel, Axiobionics, Ann Arbor, MI, USA) connected with the custom-made ES Shorts was used to apply ES, delivered at a standard constant voltage of 150 V. Using 35 Hz bi-phasic impulse frequencies, a tetanic contraction of the gluteal, quadriceps and hamstring muscles of both legs was induced with a square pulse form with one second slope up and one down. The current amplitude resulting in the best muscle activation was determined for each individual participant by increasing the amplitude in steps of 10 mA to the maximum tolerated, without discomfort or excessive or painful muscle contractions. The electrical stimulator only activated if there was electrode-to-skin contact and contact between electrodes and stimulator. The stimulator’s settings were kept constant during the two weeks. The stimulator was connected to the ES-shorts with 1.5-meter long electrical wires, allowing the participant to place the stimulator next to his or her bed, for example on the bed table, while wearing the ES-shorts in bed.
The ES-shorts used in this study were made of partially elastical lycra material with velcro flaps. When these flaps are untied the shorts can be fully folded open. The person putting the shorts on can lay down and connect the flaps to close the shorts around the waist and legs. See Fig. 2 for the ES-garment (ES-Shorts + stimulator + wires). The shorts contain flat-embedded surface electrodes with (0.5 cm) small soft attachable pockets filled with hydrophilic granules (Soil Moist Granules®, JRM Cleveland Inc., Ohio USA).
Participants were instructed to moisturize these pockets under a water tap for 10 s and then attach them to the marked places inside the open folded shorts. The stimulators were programmed to deliver 8 h of ES, with 1-h stimulation cycles. Each cycle consisted of 30 min with 36 contractions, 10 s on and 40 s off (1:4 s duty cycle) according to Smit et al. [20, 23], followed by 30 min of rest. This cycle was repeated until 8 h of stimulation and rest were completed.
Feasibility of the overnight muscle activation
Feasibility was tested in three ways: 1. muscle contraction size and fatigue, 2. sleep quality, and 3. the usability of the ES shorts with stimulator and wires when used in bed overnight.
Muscle contraction size and fatigue
Whether the ES-shorts were effective in inducing contractions for 8 h was determined by questioning the participants what they noticed after 8 h of muscle activation, and by continuous measurement of muscle contraction sizes. For this purpose, a Futek load cell (LSB200, 25 lb, JR S-beam load cell, Futek Inc., California, USA) was fixed around the participant’s upper left leg, using a Velcro strap with elastic ends. The device was calibrated prior to each use. When leg muscles contract, the leg circumference increases as the muscle shortens and thickens, resulting in more strain on the load cell and subsequently a higher output (arbitrary units in Volt). The difference between the output during a contraction and during rest is indicative of changes in muscle cross section and muscular strength.
Occurrence of muscle fatigue was determined in two ways. Firstly, relative contraction size was measured for each participant over the first two contraction cycles (of each 36 contractions; in total 2 h). Average contraction size over the first three and the last three contractions was calculated for both stimulation cycles. Fatigue was defined as a significant decrease of this muscle contraction size, by comparing both the last 3 contractions of one cycle to the first 3 ones of the next, after 30 min of rest. Recovery was calculated as the difference in relative contraction size at the end of cycle one and the average contraction size at the begin of the next cycle. All participants were also asked whether contractions of activated muscles in their paralyzed legs were still visible at the end of the night.
Sleep quality
A Sleep Quality Visual Analogue Scale (SQ-VAS) [22] and the Pittsburgh Sleeping Questionnaire Index (PSQI) [24], both validated instruments, were administered at the end of the intervention and 4 weeks after. The SQ-VAS consists of 3 questions on sleep quality and the PSQI has 9 questions [25, 26]. The PSQI items are summed into a single number indicating sleep quality is either good or bad, with a cutoff point of 3. A lower score indicates good sleep, three or higher: bad sleep quality.
ES-shorts usability
All participants filled out a custom questionnaire containing 8 questions about the overnight stimulation and the ES-shorts at the end of the intervention period (Table 2 and Fig. 3). Answers were given on a 5-point Likert scale ranging from 1 ‘I totally disagree’ to 5 ‘I totally agree’.
Statistical analysis
Two repeated measures ANOVAs were used to determine differences in muscle contraction sizes between cycles. First, the difference in average muscle contraction sizes of the first and the second cycle (2 within-subject levels) of the first night was determined. Secondly, the average of the final 3 contractions of the first cycle to the first 3 of the next cycle were compared (2 within-subjects levels). Average contraction size of the first three contractions (of the first cycle) was set as 100%.
To analyze the (SQ-VAS and PSQI-) questionnaires, paired Student’s t-tests were used to examine differences between the answers directly after the intervention and after 4 weeks without overnight ES. The frequencies of answers on the questionnaire on the ES-shorts usability were described. All data are presented as mean ± standard deviation (SD), except the results of the PSQI which were described as median. Statistical significance was set a priori at a p-value ≤ 0.05. All data were analyzed using the statistical package IBM SPSS for IBM Mac software (SPSS Inc., version 20, Chicago, IL, USA).
Results
None of the participants developed skin problems due to the electrodes or the stimulation, or had complaints of autonomic dysreflexia during the overnight ES-induced muscle activation. None of the participants had problems or complains about unexpected muscle contractions (or spasms), nor problems with (handling) the wires. Some participants reported unexpected positive findings like decreasing of inflammation around Ischial tuberosities area, increased ability to sit throughout the day without pain, improved wound healing, and improved bowel function.
Muscle contractions
In three participants, contractions could not be reliably measured. One participant had visible contractions but extreme atrophied legs, with hardly any muscle volume left. Two participants had spasms due to the induced muscle activation, causing their contraction data to be unreliable. In five participants mean contraction in the first cycle was significantly larger as compared to the second cycle (p = 0.03), with average relative contractions being 76.7% (±14.1) in the first cycle, and 66.9% (±27.2) in the second. Contractions at the begin of the second cycle were 79,5% (±18.7) and significantly larger compared to contractions at the end of the first cycle, 63.7% (±21.7) (p = 0.00), indicating muscle fatigue and recovery after 30 min of rest. Finally, contractions were detected at the end of cycle one and two 63.7 (±21.72) and 57.3% (±23.7) respectively, and muscle contractions could still be detected at the end of 8 h of muscle activation according to all participants. In Fig. 4, a typical example of two contraction cycles of one participant is shown.
Sleep quality
Result of the PSQI questionnaire revealed poor sleep quality in three participants directly after the intervention, and poor sleep quality in four participants in follow-up. The group participants scored the general sleep quality as poor, median 4 [2,3,4,5,6,7] during intervention and poor 5 [1,2,3,4,5,6,7,8,9,10] during the month without the intervention.
Results of SQ-VAS are presented in Fig. 4. Sleep quality after 2 weeks of ES was 11.6% (significantly) better compared to 4 weeks follow-up without ES (week 6): 66 to 75 [0–100] (p = 0.04). Scores for tired versus fit did not (significantly) differ between week 2 or 6, indicating (feelings of) fitness did not alter due to ES-induced muscle activation. Score for ES disturbance of the night’s sleep was 82 (0–100), in favor of not disturbing the night’s sleep.
ES-shorts usability
Results of the usability questionnaire are presented in Fig. 3. Seven of 8 participants (87.5%) needed help to put the ES shorts on. Seven (of 8) participants (87.5%) reported that ES is totally not painful. All (100%) stated ES did not prevent them from falling asleep. Seven participants (87.5%) found stimulation and contraction of the muscles pleasant, 1 responded neutral. Seven participants (87.5%) as well indicated they were willing to use the ES shorts in the future if effects are proven positive, 1 responded neutral.
Discussion
This pilot study showed the feasibility of overnight ES in people with an SCI. None of the participants stopped with the intervention during the 2 weeks due to adverse events.
Using the ES-shorts, muscle contractions decreased during the stimulation cycles, which is most likely due to fatigue of fast fatigue type 2 muscle fibers [27,28,29,30,31]. After SCI, composition of muscle fibers in muscles below the lesion level shifts towards fast fatigue muscle fibers [32,33,34,35,36,37]. As a result, contraction size is likely to decrease over time after repetitive contractions. Although contractions decreased during stimulation, contractions were still detected at the end of stimulation cycles, indicating that (type 1 and type 2a) muscle fibers were active throughout the stimulation period. In addition, muscles recovered in between stimulation cycles, as contraction size after 30 min of rest, at the beginning of the second cycle were significantly larger than at the end of first cycle.
This study also showed that overnight ES-induced muscle activation, in people with SCI does not disturb sleep. Most (7 of 8) participants even indicated they would like to continue overnight use of the ES-shorts in the future, as they believed their quality of sleep improved. We believe improvements seen in sleep duration and quality in our participants are related to the increased muscle activity, the related physiological changes and to the catabolic process caused by the muscle activation. It might be a result of the physiological muscle breakdown that occurs during physical activity. The body requires a deeper and more restful sleep to repair the damage. Gebhart et al. [38] showed that in 114 abled-bodied participants physical exercise contributes to better sleep quality. A 6-week moderate physical exercise, program, conducted weekly, significantly improved sleep quality, daytime mood, depressive symptoms, and vitality. Derived from PSQI sub scores, the intervention group reported increased sleep duration, shortened sleep latency, fewer awakenings after sleep onset, and overall better sleep efficiency compared to controls. The attained scores were well sustained and enhanced over a time that lasted through to the follow-up 18 weeks later. We believe these findings in the able-bodied also have implications concerning healthy lifestyle approaches for people with a SCI. In summary related to present study: ES-induced muscles contractions, as a form of physical exercise, may cause deeper sleep.
The usability of the ES garment was good. Most participants were enthusiastic about using the ES-shorts, and the wires did not hinder them in bed. All participants had placed the stimulator connected to the ES-shorts on the bed table next to their bed. The ES-shorts were specially developed, with the alignment of the electrodes directly over the skin. Seven of eight participants needed help to apply the shorts due to limited hand function or trunk stability problems. Although the size of the shorts used in our study was not perfect for everyone, muscle activation was still effective. One participant recommended the use of a thinner material than the Lycra material used, to make wearing the shorts possibly more comfortable and we believe in the future individually fitted ES shorts should be made to avoid fitting problems.
Clinical implications of this study concern the challenge to lower the incidence of pressure ulcers in SCI due to sitting. As mentioned in the introduction: ES-induced contractions of paralyzed gluteal and hamstrings muscles have been found to decrease seating pressure, while sitting in the wheelchair due to contraction induced changes in muscle shape and tone. Moreover, repeated muscle contractions also increase muscle mass [14, 15] and enhance circulation [16,17,18,19]. Therefore, ES seems to be a promising prophylactic aid in PU management. We believe that the nightly use of the ES-shorts can be an important part of the daily routine of people with SCI, in addition to routine measures to prevent PUs. The ES-shorts do not reduce IT pressure when used lying (in bed, overnight) but do generate the positive physiological effects of muscle activation and training. The 8 h of muscle activation is effective in increasing tissue oxygenation and reducing muscle atrophy of the activated muscles of the buttocks [16, 20, 21]. The sample size in this study was relatively small but large enough for this pilot study on feasibility. Participants in the present study were enthusiastic and experienced using the shorts overnight as not at all hindering. All but one intended to continue using the shorts after finishing their participation in this study.
No training effects of the intervention program were found on fatigue. Some participants stated that muscles were ‘easier to activate’ throughout the night as the intervention progressed. We believe it would be beneficial to reexamine the length of time that ES was applied [16, 39] as 2-weeks is probably too short a time for significant physiological training effects to occur in the activated muscles.
Future studies should focus on prolonged ES overnight using the effective ES-shorts and protocol used in this study. We believe a longer period of 6 weeks [40,41,42,43,44,45,46,47,48,49,50,51] should be tried and that randomized clinical trials should follow to determine the clinically relevant increase in muscle mass, blood flow and oxygenation needed to decrease the incidence of PUs via ES.
Conclusion
In this pilot study, overnight electrical stimulation of leg muscles was a safe and feasible method of inducing paralyzed leg muscle contractions in people with SCI. Usability of the ES-shorts, specially developed for this study, was good. In the continuing challenge to lower the incidence of pressure ulcers in SCI due to sitting, future studies should focus on prolonged ES overnight in order to study a possible increase in muscle volume, blood flow and muscle oxygenation, and subsequent decrease in the incidence of PUs.
References
Noreau L, Proulx P, Gagnon L, Drolet M, Laramee MT. Secondary impairments after spinal cord injury: a population-based study. Am J Phys Med Rehabil. 2000;79:526–35.
Liu LQ, Nicholson GP, Knight SL, Chelvarajah R, Gall A, Middleton FR, et al. Interface pressure and cutaneous hemoglobin and oxygenation changes under ischial tuberosities during sacral nerve root stimulation in spinal cord injury. J Rehabil Res Dev. 2006;43:553–64.
Krause JS, Vines CL, Farley TL, Sniezek J, Coker J. An exploratory study of pressure ulcers after spinal cord injury: relationship to protective behaviors and risk factors. Arch Phys Med Rehabil. 2001;82:107–13.
Gorecki C, Brown JM, Nelson EA, Briggs M, Schoonhoven L, Dealey C, et al. Impact of pressure ulcers on quality of life in older patients: a systematic review. J Am Geriatr Soc. 2009;57:1175–83.
Byrne DW, Salzberg CA. Major risk factors for pressure ulcers in the spinal cord disabled: a literature review. Spinal Cord. 1996;34:255–63.
Gefen A, Levine J. The false premise in measuring body-support interface pressures for preventing serious pressure ulcers. J Med Eng Technol. 2007;31:375–80.
Linder-Ganz E, Gefen A. Stress analyses coupled with damage laws to determine biomechanical risk factors for deep tissue injury during sitting. J Biomech Eng. 2009;131:011003.
Rajan S, McNeely MJ, Warms C, Goldstein B. Clinical assessment and management of obesity in individuals with spinal cord injury: a review. J Spinal Cord Med. 2008;31:361–72.
Elsner JJ, Gefen A. Is obesity a risk factor for deep tissue injury in patients with spinal cord injury? J Biomech. 2008;41:3322–31.
Linder-Ganz E, Shabshin N, Itzchak Y, Gefen A. Assessment of mechanical conditions in sub-dermal tissues during sitting: a combined experimental-MRI and finite element approach. J Biomech. 2007;40:1443–54.
de Groot PC, Poelkens F, Kooijman M, Hopman MT. Preserved flow-mediated dilation in the inactive legs of spinal cord-injured individuals. Am J Physiol Heart Circ Physiol. 2004;287:H374–80.
Nash MS, Montalvo BM, Applegate B. Lower extremity blood flow and responses to occlusion ischemia differ in exercise-trained and sedentary tetraplegic persons. Arch Phys Med Rehabil. 1996;77:1260–5.
Reenalda J, van Geffen P, Snoek G, Jannink M, Ijzerman M, Rietman H. Effects of dynamic sitting interventions on tissue oxygenation in individuals with spinal cord disorders. Spinal Cord. 2010;48:336–41.
Baldi JC, Jackson RD, Moraille R, Mysiw WJ. Muscle atrophy is prevented in patients with acute spinal cord injury using functional electrical stimulation. Spinal Cord. 1998;36:463–9.
Bogie KM, Wang X, Triolo RJ. Long-term prevention of pressure ulcers in high-risk patients: a single case study of the use of gluteal neuromuscular electric stimulation. Arch Phys Med Rehabil. 2006;87:585–91.
Chilibeck PD, Jeon J, Weiss C, Bell G, Burnham R. Histochemical changes in muscle of individuals with spinal cord injury following functional electrical stimulated exercise training. Spinal Cord. 1999;37:264–8.
de Groot P, Crozier J, Rakobowchuk M, Hopman M, MacDonald M. Electrical stimulation alters FMD and arterial compliance in extremely inactive legs. Med Sci Sports Exerc. 2005;37:1356–64.
Gerrits HL, de Haan A, Sargeant AJ, van Langen H, Hopman MT. Peripheral vascular changes after electrically stimulated cycle training in people with spinal cord injury. Arch Phys Med Rehabil. 2001;82:832–9.
Thijssen DH, Heesterbeek P, van Kuppevelt DJ, Duysens J, Hopman MT. Local vascular adaptations after hybrid training in spinal cord-injured subjects. Med Sci Sports Exerc. 2005;37:1112–8.
Smit CAJ, Haverkamp GLG, de Groot S, Stolwijk-Swuste JM, Janssen TWJ. Effects of electrical stimulation-induced gluteal versus gluteal and hamstring muscles activation on sitting pressure distribution in persons with a spinal cord injury. Spinal Cord. 2012;50:590–594.
van Londen A, Herwegh M, van der Zee CH, Daffertshofer A, Smit CAJ, Niezen A, et al. The effect of surface electrical stimulation of the gluteal muscles on the interface pressure in seated individuals with spinal cord injury. Arch Phys Med Rehabil. 2008;89:1724–32.
van Drongelen S, de Groot S, Veeger HE, et al. Upper extremity musculoskeletal pain during and after rehabilitation in wheelchair-using persons with a spinal cord injury. Spinal Cord 2006;44:152–9.
Smit CAJ, Legemate KJA, de Koning A, de Groot S, Stolwijk-Swuste JM, Janssen TWJ. Prolonged electrical-stimulation induced gluteal and hamstring muscle activation and sitting pressure in spinal cord injury: effect of duty cycle. J Rehabil Res Dev. 2013;50:1035–46.
Zisapel N, Nir T. Determination of the minimal clinically significant difference on a patient visual analog sleep quality scale. J Sleep Res. 2003;12:291–8.
Mondal P, Gjevre JA, Taylor-Gjevre RM, Lim HJ. Relationship between the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in a sleep laboratory referral population. Nat Sci Sleep. 2013;5:15–21.
Banerjee P, Caulfield B, Crowe L, Clark A. Prolonged electrical muscle stimulation exercise improves strength and aerobic capacity in healthy sedentary adults. J Appl Physiol. 2005;99:2307–11.
Crespo-Ruiz B, del-Ama AJ, Jiménez-Díaz FJ, Morgan J, de la Peña-González A, Gil-Agudo ÁM. Physical activity and transcutaneous oxygen pressure in men with spinal cord injury. J Rehabil Res Dev. 2012;49:913–24.
Garby L, Astrup A. The relationship between the respiratory quotient and the energy equivalent of oxygen during simultaneous glucose and lipid oxidation and lipogenesis. Acta Physiol Scand. 1987;129:443–4.
Beutler E, Waalen J. The definition of anemia: what is the lower limit of normal of the blood hemoglobin concentration? Blood. 2006;107:1747–50.
Kirshblum SC, House JG, O'Connor KC. Silent autonomic dysreflexia during a routine bowel program in persons with traumatic spinal cord injury: a preliminary study. Arch Phys Med Rehabil. 2002;83:1774–6.
Biering-Sorensen B, Kristensen IB, Kjaer M, Biering-Sorensen F. Muscle after spinal cord injury. Muscle Nerve. 2009;40:499–519.
Neumayer C, Happak W, Kern H, Gruber H. Hypertrophy and transformation of muscle fibers in paraplegic patients. Artif Organs. 1997;21:188–90.
Monroe MB, Tataranni PA, Pratley R, Manore MM, Skinner JS, Ravussin E. Lower daily energy expenditure as measured by a respiratory chamber in subjects with spinal cord injury compared with control subjects. Am J Clin Nutr. 1998;68:1223–7.
Buchholz AC, McGillivray CF, Pencharz PB. Differences in resting metabolic rate between paraplegic and able-bodied subjects are explained by differences in body composition. Am J Clin Nutr. 2003;77:371–8.
Sedlock DA, Laventure SJ. Body composition and resting energy expenditure in long term spinal cord injury. Paraplegia. 1990;28:448–54.
de Groot S, Post MW, Postma K, Sluis TA, van der Woude LH. Prospective analysis of body mass index during and up to 5 years after discharge from inpatient spinal cord injury rehabilitation. J Rehabil Med. 2010;42:922–8.
Burnham R1, Martin T, Stein R, Bell G, MacLean I, Steadward R. Skeletal muscle fibre type transformation following spinal cord injury. Spinal Cord. 1997;35:86–91.
Gebhart C, Erlacher D, Schredl M. Moderate exercise plus sleep education improves self-reported sleep quality, daytime mood, and vitality in adults with chronic sleep complaints: a waiting list-controlled trial. Sleep Disord 2011;2011:809312.
Hsu MJ, Wei SH, Chang YJ. Effect of neuromuscular electrical muscle stimulation on energy expenditure in healthy adults. Sensors (Basel). 2011;11:1932–42.
Casavola C, Paunescu LA, Fantini S, Gratton E. Blood flow and oxygen consumption with near-infrared spectroscopy and venous occlusion: spatial maps and the effect of time and pressure of inflation. J Biomed Opt. 2000;5:269–76.
Matsushita K, Homma S, Okada E. Influence of adipose tissue on muscle oxygenation measurement with an NIRS instrument. 1998;3194:159–65.
Quaresima V, Ferrari M, Franceschini MA, Hoimes ML, Fantini S. Spatial distribution of vastus lateralis blood flow and oxyhemoglobin saturation measured at the end of isometric quadriceps contraction by multichannel near-infrared spectroscopy. J Biomed Opt. 2004;9:413–20.
Schmidt W, Maassen N, Trost F, Boning D. Training induced effects on blood-volume, erythrocyte turnover and hemoglobin oxygen binding-properties. Eur J Appl Physiol Occup Physiol. 1988;57:490–8.
Cheatle TR, Potter LA, Cope M, Delpy DT, Smith PDC, Scurr JH. Near-infrared spectroscopy in peripheral vascular disease. Br J Surg. 1991;78:405–8.
Bhambhani Y, Tuchak C, Burnham R, Jeon J, Maikala R. Quadriceps muscle deoxygenation during functional electrical stimulation in adults with spinal cord injury. Spinal Cord. 2000;38:630–8.
Kooijman HM, Hopman MT, Colier WN, van der Vliet JA, Oeseburg B. Near infrared spectroscopy for noninvasive assessment of claudication. J Surg Res. 1997;72:1–7.
Kragelj R, Jarm T, Miklavcic D. Reproducibility of parameters of post occlusive reactive hyperemia measured by near infrared spectroscopy and transcutaneous oximetry. Ann Biomed Eng. 2000;28:168–73.
Yu G, Durduran T, Lech G, Zhou C, Chance B, Mohler ER 3rd, et al. Time-dependent blood flow and oxygenation in human skeletal muscles measured with noninvasive near-infrared diffuse optical spectroscopies. J Biomed Opt. 2005;10:024027.
Mayr W, Bijak M, Rafolt D, Sauermann S, Unger E, Lanmueller H. Basic design and construction of the Vienna FES implants - existing solutions and prospects for new generations of implants. Med Eng Phys. 2001;23:53–60.
Hofer C, Mayr W, Stoehr H, Unger E, Kern H. A stimulator for functional activation of denervated muscles. Artif Organs. 2002;26:276–9.
Mawson AR, Siddiqui FH, Connolly BJ, Sharp CJ, Stewart GW, Summer WR, et al. Effect of high voltage pulsed galvanic stimulation on sacral transcutaneous oxygen tension levels in the spinal cord injured. Paraplegia. 1993;31:311–9.
Acknowledgements
This manuscript was part of the thesis of the first author (CAJ Smit, MD, PhD) (January 2017). It has been previously published online as an internal publication from the VU University in Amsterdam, The Netherlands. It can therefore be found online.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study involves human subjects, and was ethically approved on 23rd of May 2013, by the local medical ethics committee ‘Slotervaart ziekenhuis/ Reade’, Amsterdam, The Netherlands. Reference number U/12.044/P1213.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Smit, C.A.J., Berenpas, F., de Groot, S. et al. Feasibility of overnight electrical stimulation-induced muscle activation in people with a spinal cord injury. A Pilot study. Spinal Cord Ser Cases 6, 5 (2020). https://doi.org/10.1038/s41394-019-0254-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-019-0254-0