Abstract
Background
Although active surveillance is the preferred management for low-risk prostate cancer (PCa), some men remain at risk of overtreatment with definitive local therapy. We hypothesized that baseline characteristics may be associated with overtreatment and represent a potential source of health disparities. We therefore examined the associations of patient and disease characteristics with the surgical overtreatment of low-risk PCa.
Methods
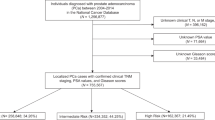
We identified men aged 45–75 years with cT1 cN0 cM0 prostate adenocarcinoma with biopsy Gleason score 6 and PSA < 10 ng/ml from 2010–2016 in the National Cancer Database (NCDB) and who underwent radical prostatectomy (RP). We evaluated the associations of baseline characteristics with clinically insignificant PCa (iPCa) at RP (i.e., “overtreatment”), defined as organ-confined (i.e., pT2) Gleason 3 + 3 disease, using multivariable logistic regression.
Results
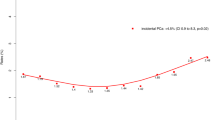
We identified 36,088 men with low-risk PCa who underwent RP. The unadjusted rate of iPCa decreased during the study period, from 54.7% in 2010 to 40.0% in 2016. In multivariable analyses adjusting for baseline characteristics, older age (OR 0.98, 95% CI 0.97–0.98), later year of diagnosis (OR 0.62, 95% CI 0.57–0.67 for 2016 vs. 2010), Black race (OR 0.85, 95% CI 0.79–0.91), treatment at an academic/research program (OR 0.82, 95% CI 0.73–0.91), higher PSA (OR 0.91, 95% CI 0.90–0.92), and higher number of positive biopsy cores (OR 0.87, 95% CI 0.86–0.88) were independently associated with a lower risk of overtreatment (iPCa) at RP. Conversely, a greater number of biopsy cores sampled (OR 1.01, 95% CI 1.01–1.02) was independently associated with an increased risk of overtreatment (iPCa) at RP.
Conclusions
We observed an ~27% reduction in rates of overtreatment of men with low-risk PCa over the study period. Several patient, disease, and structural characteristics are associated with detection of iPCa at RP and can inform the management of men with low-risk PCa to reduce potential overtreatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from American College of Surgeons through a data request.
References
Chen RC, Rumble RB, Loblaw DA, Finelli A, Ehdaie B, Cooperberg MR, et al. Active surveillance for the management of localized prostate cancer (Cancer Care Ontario Guideline): American Society of Clinical Oncology Clinical Practice Guideline Endorsement. J Clin Oncol. 2016;34:2182–90. https://doi.org/10.1200/JCO.2015.65.7759.
Sanda MG, Cadeddu JA, Kirkby E, Chen RC, Crispino T, Fontanarosa J, et al. Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part I: risk stratification, shared decision making, and care options. J Urol. 2018;199:683–90. https://doi.org/10.1016/j.juro.2017.11.095.
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017;71:618–29. https://doi.org/10.1016/j.eururo.2016.08.003.
Mohler JL. The 2010 NCCN clinical practice guidelines in oncology on prostate cancer. J Natl Compr Canc Netw. 2010;8:145. https://doi.org/10.6004/jnccn.2010.0010.
Mahal BA, Butler S, Franco I, Spratt DE, Rebbeck TR, D’Amico AV, et al. Use of active surveillance or watchful waiting for low-risk prostate cancer and management trends across risk groups in the United States, 2010-2015. JAMA. 2019;321:704–6. https://doi.org/10.1001/jama.2018.19941.
Pooli A, Salmasi A, Faiena I, Lenis AT, Johnson DC, Lebacle C, et al. Variation in surgical treatment patterns for patients with prostate cancer in the United States: do patients in academic hospitals fare better? Urol Oncol Semin Orig Investig. 2019;37:63–70. https://doi.org/10.1016/j.urolonc.2018.10.018.
Sundi D, Ross AE, Humphreys EB, Han M, Partin AW, Carter HB, et al. African American men with very low-risk prostate cancer exhibit adverse oncologic outcomes after radical prostatectomy: should active surveillance still be an option for them? J Clin Oncol J Am Soc Clin Oncol. 2013;31:2991–7. https://doi.org/10.1200/JCO.2012.47.0302.
Katz JE, Chinea FM, Patel VN, Balise RR, Venkatramani V, Gonzalgo ML, et al. Disparities in Hispanic/Latino and non-Hispanic Black men with low-risk prostate cancer and eligible for active surveillance: a population-based study. Prostate Cancer Prostatic Dis. 2018;21:533–8. https://doi.org/10.1038/s41391-018-0057-6.
Deka R, Parsons JK, Simpson DR, Riviere P, Nalawade V, Vitzthum LK, et al. African-American men with low-risk prostate cancer treated with radical prostatectomy in an equal-access health care system: implications for active surveillance. Prostate Cancer Prostatic Dis. 2020;23:581–8. https://doi.org/10.1038/s41391-020-0230-6.
Maurice MJ, Sundi D, Schaeffer EM, Abouassaly R. Risk of pathological upgrading and up staging among men with low risk prostate cancer varies by race: results from the National Cancer Database. J Urol. 2017;197:627–31. https://doi.org/10.1016/j.juro.2016.08.095.
Faisal FA, Sundi D, Cooper JL, Humphreys EB, Partin AW, Han M, et al. Racial disparities in oncologic outcomes after radical prostatectomy: long-term follow-up. Urology. 2014;84:1434–41. https://doi.org/10.1016/j.urology.2014.08.039.
Dinizo M, Shih W, Kwon YS, Eun D, Reese A, Giusto L, et al. Multi-institution analysis of racial disparity among African-American men eligible for prostate cancer active surveillance. Oncotarget. 2018;9:21359–65. https://doi.org/10.18632/oncotarget.25103.
Jalloh M, Myers F, Cowan JE, Carroll PR, Cooperberg MR. Racial variation in prostate cancer upgrading and upstaging among men with low-risk clinical characteristics. Eur Urol. 2015;67:451–7. https://doi.org/10.1016/j.eururo.2014.03.026.
Moyer VA. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157:120–34. https://doi.org/10.7326/0003-4819-157-2-201207170-00459.
Halpern JA, Shoag JE, Artis AS, Ballman KV, Sedrakyan A, Hershman DL, et al. National trends in prostate biopsy and radical prostatectomy volumes following the US Preventive Services Task Force guidelines against prostate-specific antigen screening. JAMA Surg. 2017;152:192–8. https://doi.org/10.1001/jamasurg.2016.3987.
Jemal A, Culp MB, Ma J, Islami F, Fedewa SA. Prostate cancer incidence 5 years after US Preventive Services Task Force recommendations against screening. J Natl Cancer Inst. 2021;113:64–71. https://doi.org/10.1093/jnci/djaa068.
Deka R, Courtney PT, Parsons JK, Nelson TJ, Nalawade V, Luterstein E, et al. Association between African American race and clinical outcomes in men treated for low-risk prostate cancer with active surveillance. JAMA. 2020;324:1747–54. https://doi.org/10.1001/jama.2020.17020.
Vigneswaran HT, Mittelstaedt L, Crippa A, Eklund M, Vidal A, Freedland SJ, et al. Progression on active surveillance for prostate cancer in Black men: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2022;25:165–73. https://doi.org/10.1038/s41391-021-00425-1.
Iremashvili V, Soloway MS, Rosenberg DL, Manoharan M. Clinical and demographic characteristics associated with prostate cancer progression in patients on active surveillance. J Urol. 2012;187:1594–9. https://doi.org/10.1016/j.juro.2011.12.082.
Sundi D, Faisal FA, Trock BJ, Landis PK, Fen Z, Ross AE, et al. Reclassification rates are higher among African American men than Caucasians on active surveillance. Urology. 2015;85:155–60. https://doi.org/10.1016/j.urology.2014.08.014.
Tosoian JJ, Mamawala M, Epstein JI, Landis P, Macura KJ, Simopoulos DN, et al. Active surveillance of grade group 1 prostate cancer: long-term outcomes from a large prospective cohort. Eur Urol. 2020;77:675–82. https://doi.org/10.1016/j.eururo.2019.12.017.
Ritch CR, Morrison BF, Hruby G, Coard KC, Mayhew R, Aiken W, et al. Pathological outcome and biochemical recurrence-free survival after radical prostatectomy in African-American, Afro-Caribbean (Jamaican) and Caucasian-American men: an international comparison. BJU Int. 2013;111:E186–90. https://doi.org/10.1111/j.1464-410X.2012.11540.x.
Mahal BA, Alshalalfa M, Spratt DE, Davicioni E, Zhao SG, Feng FY, et al. Prostate cancer genomic-risk differences between African-American and White men across Gleason scores. Eur Urol. 2019;75:1038–40. https://doi.org/10.1016/j.eururo.2019.01.010.
Krimphove MJ, Cole AP, Fletcher SA, Harmouch SS, Berg S, Lipsitz SR, et al. Evaluation of the contribution of demographics, access to health care, treatment, and tumor characteristics to racial differences in survival of advanced prostate cancer. Prostate Cancer Prostatic Dis. 2019;22:125–36. https://doi.org/10.1038/s41391-018-0083-4.
Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet. 2017;389:815–22. https://doi.org/10.1016/S0140-6736(16)32401-1.
Shungu N, Diaz VA, Perkins S, Kulshreshtha A. Physician attitudes and self-reported practices toward prostate cancer screening in Black and White men. Fam Med. 2022;54:30–7. https://doi.org/10.22454/FamMed.2022.474827.
Leapman MS, Freedland SJ, Aronson WJ, Kane CJ, Terris MK, Walker K, et al. Pathological and biochemical outcomes among African-American and Caucasian men with low risk prostate cancer in the SEARCH database: implications for active surveillance candidacy. J Urol. 2016;196:1408–14. https://doi.org/10.1016/j.juro.2016.06.086.
Schreiber D, Chhabra A, Rineer J, Weedon J, Schwartz D. A population-based study of men with low-volume low-risk prostate cancer: does African-American race predict for more aggressive disease? Clin Genitourin Cancer. 2015;13:e259–64. https://doi.org/10.1016/j.clgc.2015.02.006.
Al Awamlh BAH, Patel N, Ma X, Calaway A, Ponsky L, Hu JC, et al. Variation in the Use of active surveillance for low-risk prostate cancer across US census regions. Front Oncol. 2021;11. https://www.frontiersin.org/articles/10.3389/fonc.2021.644885.
Washington SL III, Jeong CW, Lonergan PE, Herlemann A, Gomez SL, Carroll PR, et al. Regional variation in active surveillance for low-risk prostate cancer in the US. JAMA Netw Open. 2020;3:e2031349. https://doi.org/10.1001/jamanetworkopen.2020.31349.
Cooperberg MR, Meeks W, Fang R, Gaylis FD, Catalona WJ, Makarov DV. Time trends and variation in the use of active surveillance for management of low-risk prostate cancer in the US. JAMA Netw Open. 2023;6:e231439.
Author information
Authors and Affiliations
Contributions
Desmond: study conception/design, interpretation of statistical analyses, manuscript preparation/revision. Kaul: study conception/design, conducting statistical analyses, manuscript preparation/revision. Fleishman: study conception/design, manuscript revision. Korets: study conception/design, manuscript revision. Chang: study conception/design, manuscript revision. Wagner: study conception/design, manuscript revision. Kim: study conception/design, manuscript revision. Aghdam: study conception/design, manuscript revision. Olumi: study conception/design, manuscript revision. Gershman: study conception/design, interpretation of statistical analyses, manuscript preparation/revision, supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests. The National Cancer Data Base (NCDB) is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The CoC’s NCDB and the hospitals participating in the CoC NCDB are the source of the de-identified data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Desmond, C., Kaul, S., Fleishman, A. et al. The association of patient and disease characteristics with the overtreatment of low-risk prostate cancer from 2010 to 2016. Prostate Cancer Prostatic Dis (2024). https://doi.org/10.1038/s41391-024-00822-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-024-00822-2