Abstract
Background
Prostate cancer (PCa) diagnosis relies on biopsies, with transrectal ultrasound (TRUS) biopsies being common. Fusion biopsy (FB) offers improved diagnostic accuracy, but the pain and anxiety experienced by patients during biopsies is often overlooked. This study aims to compare pain and anxiety levels between standard TRUS-guided biopsy (STB) and systematic plus MRI/US fusion biopsy (STB + FB).
Materials and methods
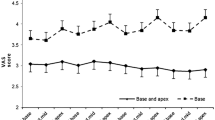
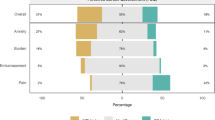
The study involved adult men undergoing biopsies, receiving identical peri-procedural care, including 2% lidocaine jelly in the rectum and subsequent 1% lidocaine injections (10cc per side) into the prostate-seminal vesicle junction and prostatic apical areas bilaterally. The biopsy technique was chosen based on clinical and imaging findings. Pre- and post-biopsy anxiety levels were assessed using the State-Trait Anxiety Inventory (STAI) questionnaire, categorized as mild (20–37), moderate (38–44), or severe (45–80). Post-biopsy pain was evaluated on a numerical rating scale, ranging from 0 to 10.
Results
Of the 165 patients, 99 underwent STB, and 66 underwent STB + FB. No significant differences were observed in age, race, prostate-specific antigen, prostate volume, or prior biopsies between the groups. The STB + FB group had more biopsy cores taken (16.2 vs. 12, p = 0.001) and a longer procedure time (23 vs. 10 min, p = 0.001). STB biopsy patients experienced lower post-procedural anxiety compared to STB + FB, with a mean difference of −7 (p = 0.001, d = 0.92). In the STB + FB group, 89% experienced severe post-procedural anxiety compared to 59% in STB (p = 0.002). There was no significant difference in post-procedural pain (p = 0.7). Patients with prior biopsies had significantly higher STAI(S) anxiety scores (p = 0.005), and the number of prior biopsies correlated with anxiety severity (p = 0.04) in STB + FB group.
Conclusion
In summary, STB + FB group demonstrated higher post-procedural anxiety levels than the STB group, with no difference in pain levels. Additionally, patients with a history of repeat biopsies were more likely to exhibit higher STAI(S) anxiety scores.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request and with permission of Duke Health.
References
Descotes J-L. Diagnosis of prostate cancer. Asian J Urol. 2019;6:129–36.
Chesnut GT, Zareba P, Sjoberg DD, Mamoor M, Carlsson S, Lee T, et al. Patient-reported pain, discomfort, and anxiety during magnetic resonance imaging-targeted prostate biopsy. Can Urol Assoc J. 2020;14:E202–e8.
Garcia-Reyes K, Passoni NM, Palmeri ML, Kauffman CR, Choudhury KR, Polascik TJ, et al. Detection of prostate cancer with multiparametric MRI (mpMRI): effect of dedicated reader education on accuracy and confidence of index and anterior cancer diagnosis. Abdom Imaging. 2015;40:134–42.
Ahdoot M, Wilbur AR, Reese SE, Lebastchi AH, Mehralivand S, Gomella PT, et al. MRI-targeted, systematic, and combined biopsy for prostate cancer diagnosis. N Engl J Med. 2020;382:917–28.
Elkhoury FF, Felker ER, Kwan L, Sisk AE, Delfin M, Natarajan S, et al. Comparison of targeted vs systematic prostate biopsy in men who are biopsy naive: the prospective assessment of image registration in the diagnosis of prostate cancer (PAIREDCAP) study. JAMA Surg. 2019;154:811–8.
Dorfinger J, Ponholzer A, Stolzlechner M, Lenart S, Baltzer P, Toepker M. MRI/ultrasound fusion biopsy of the prostate compared to systematic prostate biopsy - Effectiveness and accuracy of a combined approach in daily clinical practice. Eur J Radio. 2022;154:110432.
Spielberger C. State-trait anxiety inventory: bibliography. In: Palo Alto, editor. 2nd edn. CA: Consulting Psychologists Press; 1989.
Langley GB, Sheppeard H. The visual analogue scale: its use in pain measurement. Rheumatol Int. 1985;5:145–8.
Kayikcioglu O, Bilgin S, Seymenoglu G, Deveci A. State and trait anxiety scores of patients receiving intravitreal injections. Biomed Hub. 2017;2:1–5.
Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978;37:378–81.
Boonstra AM, Stewart RE, Köke AJ, Oosterwijk RF, Swaan JL, Schreurs KM, et al. Cut-off points for mild, moderate, and severe pain on the numeric rating scale for pain in patients with chronic musculoskeletal pain: variability and influence of sex and catastrophizing. Front Psychol. 2016;7:1466.
Assel M, Sjoberg D, Elders A, Wang X, Huo D, Botchway A, et al. Guidelines for reporting of statistics for clinical research in urology. J Urol. 2019;201:595–604.
Hodge KK, McNeal JE, Terris MK, Stamey TA. Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J Urol. 1989;142:71–4.
Loeb S, Carter HB, Berndt SI, Ricker W, Schaeffer EM. Complications after prostate biopsy: data from SEER-Medicare. J Urol. 2011;186:1830–4.
Anastasiadis E, van der Meulen J, Emberton M. Hospital admissions after transrectal ultrasound-guided biopsy of the prostate in men diagnosed with prostate cancer: a database analysis in England. Int J Urol. 2015;22:181–6.
Sharp L, Morgan E, Drummond FJ, Gavin A. The psychological impact of prostate biopsy: prevalence and predictors of procedure-related distress. Psychooncology. 2018;27:500–7.
Holtz JN, Tay KJ, Polascik TJ, Gupta RT. Integration of multiparametric MRI into active surveillance of prostate cancer. Future Oncol. 2016;12:2513–29.
Sonmez G, Tombul ST, Demirtas T, Demirtas A. Risk factors associated with pain in fusion prostate biopsy. Prostate Int. 2020;8:185–9.
Cebeci O, Ozkan A. An evaluation of factors affecting pain during transrectal ultrasonographic prostate biopsy: a real-life scenario in a retrospective cohort study. PeerJ. 2021;9:e12144.
Demirtaş A, Sönmez G, Tombul ŞT, Demirtaş T. Comparison of pain levels in fusion prostate biopsy and standard TRUS-Guided biopsy. Int Braz J Urol. 2020;46:557–62.
Arsov C, Rabenalt R, Blondin D, Quentin M, Hiester A, Godehardt E, et al. Prospective randomized trial comparing magnetic resonance imaging (MRI)-guided in-bore biopsy to MRI-ultrasound fusion and transrectal ultrasound-guided prostate biopsy in patients with prior negative biopsies. Eur Urol. 2015;68:713–20.
Krausewitz P, Schmeller H, Luetkens J, Dabir D, Ellinger J, Ritter M, et al. Prospective analysis of pain expectancy and experience during MR-fusion prostate biopsy: does reality match patients’ expectancy? World J Urol. 2022;40:2239–44.
Tsivian M, Qi P, Kimura M, Chen VH, Chen SH, Gan TJ, et al. The effect of noise-cancelling headphones or music on pain perception and anxiety in men undergoing transrectal prostate biopsy. Urology. 2012;79:32–6.
Author information
Authors and Affiliations
Contributions
SD: investigation, formal analysis, writing—original draft. ESA: investigation, formal analysis, writing-original draft. SK: investigation, writing-review & editing. MM: writing-review & editing. TT: writing-review & editing. AA: resources, writing-review & editing. ZM: data curation; writing-review & editing. TJP: conceptualization, methodology, validation and supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Duke Health institutional review board approved study, protocol no. Pro00100268 with the waiver of consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Deivasigamani, S., Adams, E.S., Kotamarti, S. et al. Comparison of procedural anxiety and pain associated with conventional transrectal ultrasound prostate biopsy to magnetic resonance imaging-ultrasound fusion-guided biopsy: a prospective cohort trial. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00760-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00760-5
This article is cited by
-
Best of 2023 in Prostate Cancer and Prostatic Diseases
Prostate Cancer and Prostatic Diseases (2024)