Abstract
Introduction
To evaluate how often men with metastatic prostate cancer (mPC) receive standard of care treatment with androgen deprivation therapy (ADT).
Methods
Men aged ≥20 years with newly diagnosed mPC (stage IV) between 2010 and 2018 were identified using California Cancer Registry data. Receipt of hormonal therapy as initial cancer treatment was examined by patient/tumor characteristics at time of diagnosis. Chi-square tests and logistic regression, adjusted for covariates, were performed to assess association between receipt of hormonal therapy and patient/tumor characteristics.
Results
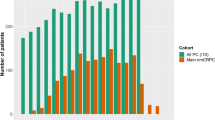
We identified 13,680 men with newly diagnosed mPC, of which 3637 had local metastasis (N1) only while 9596 had distant metastasis (M1) with or without N1 disease. 21.8 % (n = 2980) of men did not receive ADT. The highest rate of receiving ADT was among men between ages 75–84 (81.6%) and the lowest rate was in men over 85 (76.0%). Asian men had the largest proportion receiving ADT (n = 962, 81.5%) with remaining subgroups having similar proportion of men receiving ADT (76.8% to 77.2%). Once adjusted for covariates, regression results showed men with a higher Gleason score (8–10) were more likely to receive ADT (OR 2.04, 1.82–2.27, p = < 0.001) as well as men with distant sites of metastatic disease (OR 4.02, 3.62–4.46, p = < 0.001). Men residing in neighborhoods with the lowest socioeconomic status were least likely to receive ADT (OR 0.79, 0.68–0.93, p = 0.0032). No differences in receipt of ADT were observed by race/ethnicity.
Discussion
Despite significant advancements in the treatment of mPC in recent years, over one-fifth of patients did not receive ADT, which is the backbone for all new systemic therapies. This dataset might help address some of the prostate cancer care disparities in California.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity are available from the corresponding author upon reasonable request.
Change history
14 November 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41391-023-00749-0
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33. https://doi.org/10.3322/caac.21708.
Cattrini C, Castro E, Lozano R, Zanardi E, Rubagotti A, Boccardo F. et al. Current treatment options for metastatic hormone-sensitive prostate cancer. Cancers. 2019;11:1355. https://doi.org/10.3390/cancers11091355.
Huggins C, Hodges CV. Studies on prostatic cancer: I. The effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. 1941. J Urol. 2002;168:9–12. https://doi.org/10.1016/s0022-5347(05)64820-3.
Fizazi K, Tran N, Fein L, Matsubara N, Rodriguez-Antolin A, Alekseev BY. et al. Abiraterone plus prednisone in metastatic, castration-sensitive prostate cancer. N Engl J Med. 2017;377:352–60. https://doi.org/10.1056/NEJMoa1704174.
Davis ID, Martin AJ, Stockler MR, Begbie S, Chi KN, Chowdhury S. et al. Enzalutamide with standard first-line therapy in metastatic prostate cancer. N Engl J Med. 2019;381:121–31. https://doi.org/10.1056/NEJMoa1903835.
Chi KN, Agarwal N, Bjartell A, Chung BH, Pereira de Santana Domes AJ, Given R. et al. Apalutamide for metastatic, castration-sensitive prostate cancer. N Engl J Med. 2019;381:13–24. https://doi.org/10.1056/NEJMoa1903307.
Sweeney CJ, Chen YH, Carducci M, Liu G, Jarrard DF, Eisenberger M. et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med. 2015;373:737–46. https://doi.org/10.1056/NEJMoa1503747.
Freedland SJ, Sandin R, Sah J, Emir B, Mu Q, Ratiu A. et al. Treatment patterns and survival in metastatic castration‐sensitive prostate cancer in the US Veterans Health Administration. Cancer Med. 2021;10:8570–80. https://doi.org/10.1002/cam4.4372.
Swami U, Sinnott JA, Haaland B, Sayegh N, McFarland TR, Tripathi N. et al. Treatment pattern and outcomes with systemic therapy in men with metastatic prostate cancer in the real-world patients in the United States. Cancers. 2021;13:4951. https://doi.org/10.3390/cancers13194951.
Ryan CJ, Ke X, Lafeuille MH, Romdhani H, Kinkead F, Lefebvre P. et al. Management of patients with metastatic castration-sensitive prostate cancer in the real-world setting in the United States. J Urol. 2021;206:1420–9. https://doi.org/10.1097/JU.0000000000002121.
Yang J, Schupp C, Harrati A, Clarke C, Keegan T, Gomez S. Developing an area-based socioeconomic measure from American Community Survey data. Cancer Prev Inst Calif Fremont Calif. Published online 2014. https://doi.org/https://cancerregistry.ucsf.edu/sites/g/files/tkssra1781/f/wysiwyg/Yang%20et%20al.%202014_CPIC_ACS_SES_Index_Documentation_3-10-2014.pdf.
Lichtensztajn DY, Giddings BM, Morris CR, Parikh-Patel A, Kizer KW. Comorbidity index in central cancer registries: the value of hospital discharge data. Clin Epidemiol. 2017;9:601–9. https://doi.org/10.2147/CLEP.S146395.
Bluethmann SM, Wang M, Wasserman E, Chen C, Zaorsky NG, Hohl RJ. et al. Prostate cancer in Pennsylvania: the role of older age at diagnosis, aggressiveness, and environmental risk factors on treatment and mortality using data from the Pennsylvania Cancer Registry. Cancer Med. 2020;9:3623–33. https://doi.org/10.1002/cam4.3003.
Author information
Authors and Affiliations
Contributions
DJB: conceptualization, methodology, writing – original draft, writing – review & editing; AS: conceptualization, methodology, writing – original draft, writing – review & editing, supervision; DF: conceptualization, methodology, formal analysis, writing – original draft, writing – review & editing; RDC: conceptualization, methodology, writing – original draft, writing – review & editing; MPL: conceptualization, writing – review & editing; ARK: conceptualization, methodology, writing – original draft, writing – review & editing, supervision.
Corresponding author
Ethics declarations
Competing interests
ARK has the following disclosures: Stock and Other Ownership Interests: ECOM Medical. Consulting or Advisory Role: Exelixis, AstraZeneca, Bayer, Pfizer, Novartis, Genentech, Bristol Myers Squibb, EMD Serono, Immunomedics, Gilead Sciences. Speakers’ Bureau: Janssen, Astellas Medivation, Pfizer, Novartis, Sanofi, Genentech/Roche, Eisai, AstraZeneca, Bristol Myers Squibb, Amgen, Exelixis, EMD Serono, Merck, Seattle Genetics/Astellas, Myovant Sciences, Gilead Sciences, AVEO. Research Funding: Genentech, Exelixis, Janssen, AstraZeneca, Bayer, Bristol Myers Squibb, Eisai, Macrogenics, Astellas Pharma, BeyondSpring Pharmaceuticals, BioClin Therapeutics, Clovis Oncology, Bavarian Nordic, Seattle Genetics, Immunomedics, Epizyme. Travel, Accommodations, Expenses: Genentech, Prometheus, Astellas Medivation, Janssen, Eisai, Bayer, Pfizer, Novartis, Exelixis, AstraZeneca. DJB has received consulting fees from Seagen. MPL has received advisory fees from Clovis Oncology. The remaining authors (AS, DF, and RDC) have no disclosures.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The following sentence in the second paragraph of the Results section should read: “Men who were 85 years or older were least likely to receive ADT (76.0%) as opposed to men between the ages of 20-54 (78.9%). Men between ages 75-84 had the highest proportion of receipt of ADT (81.6%).” Instead of: “Men between ages 75–84 were least likely to receive ADT (81.6%) as opposed to men between the ages of 20–54 (78.9%). Men between ages 75–84 had the highest proportion of receipt of ADT among all age groups.” There is also a typographical error in Table 2. Additionally, the following sentence should read: “Specifically, men who were 85 years or older had 44% lower odds of receiving ADT (95% CI: 0.44, 0.71) and men from the lowest nSES areas had 21% lower odds of receiving ADT as the initial treatment compared to men of ages 20–54 and those from the highest nSES neighborhood, respectively.” Instead of: “Specifically, men who were 85 years or older had 44% lower odds of receiving ADT (95% CI: 0.44, 0.71) and men from the lowest nSES areas had 19% lower odds of receiving ADT as the initial treatment compared to men of ages 20–54 and those from the highest nSES neighborhood, respectively”.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Benjamin, D.J., Shrestha, A., Fellman, D. et al. Hormonal treatment for newly diagnosed metastatic prostate cancer: a population-based study from the California cancer registry. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00732-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00732-9
This article is cited by
-
Prostatectomy in oligometastatic prostate cancer: a call for high-quality evidence
Prostate Cancer and Prostatic Diseases (2024)