Abstract
Purpose
Magnetic resonance imaging (MRI) has deeply altered the prostate biopsy strategy to detect prostate cancer. However, it is still debatable whether the detection rate differs between transrectal (TR) and transperineal (TP) MRI-targeted biopsy (MRI-TB). To compare the effectiveness of these two methods for detecting both overall prostate cancer (PCa) and clinically significant PCa (csPCa), We performed a review and meta-analysis.
Methods
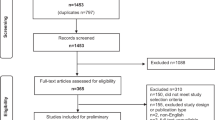
Until January 2023, we conducted a thorough search of Cochrane, Embase, Ovid, and PubMed. In total, 1482 references were identified, and 15 records were finally included. For PCa and csPCa discovered by TP and TR MRI-TB, we combined the relative sensitivity (RR) with 95% confidence intervals (CI). The RR between the TP and TR routes was established.
Results
Our study included 8826 patients in total and revealed that TP MRI-TB detected more PCa (RR 1.25 [95% CI 1.12, 1.39], p < 0.0001). In patients who underwent TP MRI-TB and TR MRI-TB at the same time or separately, TP MRI-TB had a greater detection rate of csPCa in per-patient analysis (one cohort (RR 1.33 [95% CI 1.09, 1.63], p = 0.005); two cohorts (RR 1.37 [95% CI 1.16, 1.61], p = 0.0002)). However, the detection rate of csPCa between the TP route and the TR route was comparable in per-lesion analysis (RR 0.91 [95% CI 0.76, 1.08], p = 0.28). Additionally, in the prostate’s anterior region, we found that TP MRI-TB detected more csPCa (per-lesion (RR 1.52 [95% CI 1.04, 2.23], p = 0.03); per-patient (RR 2.55 [95% CI 1.56, 4.16], p = 0.0002)).
Conclusion
According to this comprehensive study, TP MRI-TB is more effective than TR MRI-TB at detecting PCa and csPCa. Significant results persisted for detecting csPCa located in the anterior zone. The results need to be taken carefully notwithstanding the heterogeneity among the included studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA: a cancer J clinicians. 2019;69:7–34.
Steele CB, Li J, Huang B, Weir HK. Prostate cancer survival in the United States by race and stage (2001-2009): Findings from the CONCORD-2 study. Cancer. 2017;123:5160–77.
Siegel RL, Miller KD, Jemal A Cancer statistics, 2020. (2020);70:7-30.
Hilton WM, Padalecki SS, Ankerst DP, Leach RJ, Thompson IM. Temporal changes in the clinical approach to diagnosing prostate cancer. J Natl Cancer Inst Monogr. 2012;2012:162–8.
Borofsky S, George AK, Gaur S, Bernardo M, Greer MD, Mertan FV, et al. What Are We Missing? False-Negative Cancers at Multiparametric MR Imaging of the Prostate. Radiology. 2018;286:186–95.
Coakley FV, Oto A, Alexander LF, Allen BC, Davis BJ, Froemming AT, et al. ACR appropriateness criteria(®) prostate cancer-pretreatment detection, surveillance, and staging. J Am Coll Radiology: JACR. 2017;14:S245–s57.
Le JD, Tan N, Shkolyar E, Lu DY, Kwan L, Marks LS, et al. Multifocality and prostate cancer detection by multiparametric magnetic resonance imaging: correlation with whole-mount histopathology. Eur Urol. 2015;67:569–76.
AsTRALDI AJUCR. Diagnosis of cancer of the prostate: biopsy by rectal route. 1937;41:421.
Hodge KK, McNeal JE, Stamey TA. Ultrasound guided transrectal core biopsies of the palpably abnormal prostate. J Urol. 1989;142:66–70.
Moe A, Hayne D. Transrectal ultrasound biopsy of the prostate: does it still have a role in prostate cancer diagnosis? Transl Androl Urol. 2020;9:3018–24.
Bruyère F, Malavaud S, Bertrand P, Decock A, Cariou G, Doublet JD, et al. Prosbiotate: a multicenter, prospective analysis of infectious complications after prostate biopsy. J Urol. 2015;193:145–50.
Carignan A, Roussy JF, Lapointe V, Valiquette L, Sabbagh R, Pépin J. Increasing risk of infectious complications after transrectal ultrasound-guided prostate biopsies: time to reassess antimicrobial prophylaxis? Eur Urol. 2012;62:453–9.
Thomson A, Li M, Grummet J, Sengupta S. Transperineal prostate biopsy: a review of technique. Transl Androl Urol. 2020;9:3009–17.
Stefanova V, Buckley R, Flax S, Spevack L, Hajek D, Tunis A, et al. Transperineal prostate biopsies using local anesthesia: experience with 1,287 patients. prostate cancer detection rate, complications and patient tolerability. J Urol. 2019;201:1121–6.
Xue J, Qin Z, Cai H, Zhang C, Li X, Xu W, et al. Comparison between transrectal and transperineal prostate biopsy for detection of prostate cancer: a meta-analysis and trial sequential analysis. Oncotarget. 2017;8:23322–36.
Skouteris VM, Crawford ED, Mouraviev V, Arangua P, Metsinis MP, Skouteris M, et al. Transrectal ultrasound-guided versus transperineal mapping prostate biopsy: complication comparison. Rev Urol. 2018;20:19–25.
Tu X, Liu Z, Chang T, Qiu S, Xu H, Bao Y, et al. Transperineal magnetic resonance imaging-targeted biopsy may perform better than transrectal route in the detection of clinically significant prostate cancer: systematic review and meta-analysis. Clin Genitourin Cancer. 2019;17:e860–e70.
Rai BP, Mayerhofer C, Somani BK, Kallidonis P, Nagele U, Tokas T. Magnetic resonance imaging/ultrasound fusion-guided transperineal versus magnetic resonance imaging/ultrasound fusion-guided transrectal prostate biopsy-a systematic review. Eur Urol Oncol. 2021;4:904–13.
Loy LM, Lim GH, Leow JJ, Lee CH, Tan TW, Tan CH. A systematic review and meta-analysis of magnetic resonance imaging and ultrasound guided fusion biopsy of prostate for cancer detection-Comparing transrectal with transperineal approaches. Urol Oncol. 2020;38:650–60.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ (Clin Res ed). 2016;355:i4919.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clin Res ed). 2011;343:d5928.
McGuinness LA, Higgins JPT Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Research Synthesis Methods. (2020);n/a.
Wegelin O, Exterkate L, van der Leest M, Kummer JA, Vreuls W, de Bruin PC, et al. The FUTURE trial: a multicenter randomised controlled trial on target biopsy techniques based on magnetic resonance imaging in the diagnosis of prostate cancer in patients with prior negative biopsies. Eur Urol. 2019;75:582–90.
Ber Y, Segal N, Tamir S, Benjaminov O, Yakimov M, Sela S, et al. A noninferiority within-person study comparing the accuracy of transperineal to transrectal MRI-US fusion biopsy for prostate-cancer detection. Prostate Cancer Prostatic Dis. 2020;23:449–56.
El-Achkar A, Abou Heidar N, Labban M, Al-Moussawy M, Moukaddem H, Nasr R, et al. MRI/US fusion transperineal versus transrectral biopsy of prostate cancer: Outcomes and complication rates, a tertiary medical center experience in the Middle East. Turkish J Urol. 2022;48:98–105.
Hsieh PF, Chang TY, Lin WC, Chang H, Chang CH, Huang CP, et al. A comparative study of transperineal software-assisted magnetic resonance/ultrasound fusion biopsy and transrectal cognitive fusion biopsy of the prostate. BMC Urol. 2022;22:72.
Kaufmann S, Russo GI, Thaiss W, Notohamiprodjo M, Bamberg F, Bedke J, et al. Cognitive versus software-assisted registration: development of a new nomogram predicting prostate cancer at MRI-targeted biopsies. Clin Genitourin Cancer. 2018;16:e953–e60.
Koparal MY, Sözen TS, Karşıyakalı N, Aslan G, Akdoğan B, Şahin B, et al. Comparison of transperineal and transrectal targeted prostate biopsy using Mahalanobis distance matching within propensity score caliper method: A multicenter study of Turkish Urooncology Association. Prostate. 2022;82:425–32.
Marenco Jimenez JL, Claps F, Ramón-Borja JC, Mascarós Martinez JM, Gutierrez AW, Lozano ÁGF, et al. Rebiopsy rate after transperineal or transrectal prostate biopsy. Prostate Int. 2021;9:78–81.
Pepe P, Garufi A, Priolo G, Pennisi M. Transperineal Versus Transrectal MRI/TRUS fusion targeted biopsy: detection rate of clinically significant prostate cancer. Clin Genitourin Cancer. 2017;15:e33–e6.
Pepe P, Garufi A, Priolo GD, Pennisi M. Multiparametric MRI/TRUS fusion prostate biopsy: advantages of a transperineal approach. Anticancer Res. 2017;37:3291–4.
Rabah D, Al-Taweel W, Khan F, Arafa M, Mehmood S, Mokhtar A, et al. Transperineal versus transrectal multi-parametric magnetic resonance imaging fusion targeted prostate biopsy. Saudi Med J. 2021;42:649–54.
Tewes S, Peters I, Tiemeyer A, Peperhove M, Hartung D, Pertschy S, et al. Evaluation of MRI/Ultrasound Fusion-Guided Prostate Biopsy Using Transrectal and Transperineal Approaches. BioMed Res Int. 2017;2017:2176471.
Ugge H, Jarl S, Georgouleas P, Andersson SO, Sundqvist P, Frey J. Diagnostic outcomes from transrectal and transperineal prostate biopsies—experiences from a Swedish tertiary care Centre. Scand J Urol. 2021;55:434–40.
Winoker JS, Wajswol E, Falagario U, Maritini A, Moshier E, Voutsinas N, et al. Transperineal versus transrectal targeted biopsy with use of electromagnetically-tracked MR/US Fusion Guidance Platform for the Detection of Clinically Significant Prostate Cancer. Urology. 2020;146:278–86.
Yaxley AJ, Yaxley JW, Thangasamy IA, Ballard E, Pokorny MR. Comparison between target magnetic resonance imaging (MRI) in-gantry and cognitively directed transperineal or transrectal-guided prostate biopsies for Prostate Imaging-Reporting and Data System (PI-RADS) 3-5 MRI lesions. BJU Int. 2017;120:43–50.
Zattoni F, Marra G, Kasivisvanathan V, Grummet J, Nandurkar R, Ploussard G, et al. The detection of prostate cancer with magnetic resonance imaging-targeted prostate biopsies is superior with the transperineal vs the transrectal approach. a european association of urology-young academic urologists prostate cancer working group multi-institutional study. J Urol. 2022;208:830–7.
Wegelin O, Exterkate L, van der Leest M, Kelder JC, Bosch J, Barentsz JO, et al. Complications and adverse events of three magnetic resonance imaging-based target biopsy techniques in the diagnosis of prostate cancer among men with prior negative biopsies: results from the FUTURE trial, a multicentre randomised controlled trial. Eur Urol Oncol. 2019;2:617–24.
Udeh EI, Amu OC, Nnabugwu II, Ozoemena O. Transperineal versus transrectal prostate biopsy: our findings in a tertiary health institution. Niger J Clin Pract. 2015;18:110–4.
Guo LH, Wu R, Xu HX, Xu JM, Wu J, Wang S, et al. Comparison between ultrasound guided transperineal and transrectal prostate biopsy: a prospective, randomized, and controlled trial. Sci Rep. 2015;5:16089.
Pradere B, Veeratterapillay R, Dimitropoulos K, Yuan Y, Omar MI, MacLennan S, et al. Nonantibiotic strategies for the prevention of infectious complications following prostate biopsy: a systematic review and meta-analysis. J Urol. 2021;205:653–63.
Arsov C, Rabenalt R, Blondin D, Quentin M, Hiester A, Godehardt E, et al. Prospective randomized trial comparing magnetic resonance imaging (MRI)-guided in-bore biopsy to MRI-ultrasound fusion and transrectal ultrasound-guided prostate biopsy in patients with prior negative biopsies. Eur Urol. 2015;68:713–20.
Kaufmann S, Russo GI, Bamberg F, Löwe L, Morgia G, Nikolaou K, et al. Prostate cancer detection in patients with prior negative biopsy undergoing cognitive-, robotic- or in-bore MRI target biopsy. World J Urol. 2018;36:761–8.
Puech P, Rouvière O, Renard-Penna R, Villers A, Devos P, Colombel M, et al. Prostate cancer diagnosis: multiparametric MR-targeted biopsy with cognitive and transrectal US-MR fusion guidance versus systematic biopsy-prospective multicenter study. Radiology. 2013;268:461–9.
Wysock JS, Rosenkrantz AB, Huang WC, Stifelman MD, Lepor H, Deng FM, et al. A prospective, blinded comparison of magnetic resonance (MR) imaging-ultrasound fusion and visual estimation in the performance of MR-targeted prostate biopsy: the PROFUS trial. Eur Urol. 2014;66:343–51.
Mai Z, Zhou Z, Yan W, Xiao Y, Zhou Y, Liang Z, et al. The transverse and vertical distribution of prostate cancer in biopsy and radical prostatectomy specimens. BMC cancer. 2018;18:1205.
Schouten MG, van der Leest M, Pokorny M, Hoogenboom M, Barentsz JO, Thompson LC, et al. Why and Where do We Miss Significant Prostate Cancer with Multi-parametric Magnetic Resonance Imaging followed by Magnetic Resonance-guided and Transrectal Ultrasound-guided Biopsy in Biopsy-naïve Men? Eur Urol. 2017;71:896–903.
Giannarini G, Crestani A, Rossanese M, Ficarra V. Multiparametric magnetic resonance imaging targeted biopsy for early detection of prostate cancer: all that glitters is not gold! Eur Urol. 2017;71:904–6.
Williams C, Ahdoot M, Daneshvar MA, Hague C, Wilbur AR, Gomella PT, et al. Why does magnetic resonance imaging-targeted biopsy miss clinically significant cancer? J Urol. 2022;207:95–107.
Halstuch D, Baniel J, Lifshitz D, Sela S, Ber Y, Margel D. Assessment of needle tip deflection during transrectal guided prostate biopsy: implications for targeted biopsies. J Endourol. 2018;32:252–6.
Acknowledgements
The authors thank Dr. Chi Chen, Changzhong Chen, and Xing-Lin Chen for providing statistical methodology consultation.
Funding
This work was supported by the National Natural Science Foundation of China (Grant number: 81500522) and Science & Technology Department of Sichuan Province (Grant number: 2020YFS0090, 2020YFS0046) and Cadre Health Research Project of Sichuan Province (Grant number: ZH2023-102)
Author information
Authors and Affiliations
Contributions
Conceptualization: XT, QW, YGB. Data curation: QYW, CCZ. Formal analysis: QYW, CCZ, XT. Data collection: QYW, CCZ, XT, JJY, THL, ZHL, LY, SQ. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, Q., Tu, X., Zhang, C. et al. Transperineal magnetic resonance imaging targeted biopsy versus transrectal route in the detection of prostate cancer: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00729-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00729-4
This article is cited by
-
A novel biopsy scheme for prostate cancer: targeted and regional systematic biopsy
BMC Urology (2024)
-
Transrectal prostate biopsy: easy, effective and safe
Prostate Cancer and Prostatic Diseases (2024)