Abstract
Background
While both seminal vesicle (SVI) and lymph-node invasion (LNI) have been identified as adverse prognostic variables among men undergoing radical prostatectomy (RP), the relative impact of each of these features on subsequent oncologic outcomes has not been well defined. We assessed the impact of LNI on long-term oncologic outcomes among patients with SVI at RP.
Methods
We reviewed 19,519 patients who underwent RP and identified 2043 with SVI. Metastasis-free (MFS), cancer-specific (CSS), and overall survival (OS) were estimated for patients with SVI, stratified by the presence and number of pelvic lymph node metastases. Cox proportional hazards models were used to evaluate the independent association of the number of metastatic nodes and lymph node density with oncologic outcomes among patients with SVI, controlling for age, year of surgery, margin status, preoperative PSA, pathologic Gleason score, extraprostatic extension, and use of adjuvant therapies.
Results
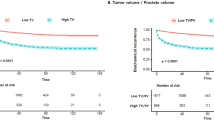
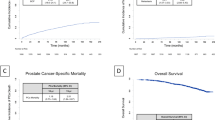
At a median follow up of 12.1 years (IQR 7.0,18.6), 548 patients developed metastatic disease and 1331 died, including 406 who died from prostate cancer (PCa). We found that, among patients with SVI, the presence of a single positive lymph node was not associated with incrementally adverse oncologic outcomes compared to no nodal metastasis at RP, with 10-year MFS, CSS, and OS rates of 81.3% versus 78.3%(p = 0.18), 86.5% versus 89.8%(p = 0.32), and 72.8% versus 76.7%(p = 0.53), respectively. In contrast, on multivariable analyses, the presence of ≥2 metastatic nodes and a 20% lymph-node density cut off remained independently associated with worse survival.
Conclusions
SVI represents an adverse pathologic feature such that the presence of a single positive pelvic lymph node did not further adversely impact prognosis. Meanwhile, a significant number of involved nodes was associated with decreased survival. These findings may aid in risk-stratification as well as clinical trial design for such high-risk patients following surgery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article.
References
Eggener SE, Roehl KA, Smith ND, Antenor JA, Han M, Catalona WJ. Contemporary survival results and the role of radiation therapy in patients with node negative seminal vesicle invasion following radical prostatectomy. J Urol. 2005;173:1150–5.
Pierorazio PM, Ross AE, Schaeffer EM, Epstein JI, Han M, Walsh PC, et al. A contemporary analysis of outcomes of adenocarcinoma of the prostate with seminal vesicle invasion (pT3b) after radical prostatectomy. J Urol. 2011;185:1691–7.
Boorjian SA, Thompson RH, Siddiqui S, Bagniewski S, Bergstralh EJ, Karnes RJ, et al. Long-term outcome after radical prostatectomy for patients with lymph node positive prostate cancer in the prostate specific antigen era. J Urol. 2007;178:864–70.
Schumacher MC, Burkhard FC, Thalmann GN, Fleischmann A, Studer UE. Good outcome for patients with few lymph node metastases after radical retropubic prostatectomy. Eur Urol. 2008;54:344–52.
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67:93–9.
Flammia RS, Hoeh B, Sorce G, Chierigo F, Hohenhorst L, Tian Z, et al. Contemporary seminal vesicle invasion rates in NCCN high-risk prostate cancer patients. Prostate 2022;82:1051–9.
Fossati N, Passoni NM, Moschini M, Gandaglia G, Larcher A, Freschi M, et al. Impact of stage migration and practice changes on high-risk prostate cancer: results from patients treated with radical prostatectomy over the last two decades. BJU Int. 2016;117:740–7.
Bukavina L, Luckenbaugh AN, Hofman MS, Hope T, Kamran SC, Murphy DG, et al. Incorporating prostate-specific membrane antigen positron emission tomography in management decisions for men with newly diagnosed or biochemically recurrent prostate cancer. Eur Urol. 2023;83:521–33.
Mikel Hubanks J, Boorjian SA, Frank I, Gettman MT, Houston Thompson R, Rangel LJ, et al. The presence of extracapsular extension is associated with an increased risk of death from prostate cancer after radical prostatectomy for patients with seminal vesicle invasion and negative lymph nodes. Urol Oncol. 2014;32:26.e1–7.
Carver BS, Bianco FJ Jr, Scardino PT, Eastham JA. Long-term outcome following radical prostatectomy in men with clinical stage T3 prostate cancer. J Urol. 2006;176:564–8.
Swanson GP, Goldman B, Tangen CM, Chin J, Messing E, Canby-Hagino E, et al. The prognostic impact of seminal vesicle involvement found at prostatectomy and the effects of adjuvant radiation: data from Southwest Oncology Group 8794. J Urol. 2008;180:2453–7.
Secin FP, Bianco FJ Jr, Vickers AJ, Reuter V, Wheeler T, Fearn PA, et al. Cancer-specific survival and predictors of prostate-specific antigen recurrence and survival in patients with seminal vesicle invasion after radical prostatectomy. Cancer. 2006;106:2369–75.
Masterson TA, Pettus JA, Middleton RG, Stephenson RA. Isolated seminal vesicle invasion imparts better outcomes after radical retropubic prostatectomy for clinically localized prostate cancer: prognostic stratification of pt3b disease by nodal and margin status. Urology .2005;66:152–5.
Palapattu GS, Allaf ME, Trock BJ, Epstein JI, Walsh PC. Prostate specific antigen progression in men with lymph node metastases following radical prostatectomy: results of long-term followup. J Urol. 2004;172:1860–4.
Daneshmand S, Quek ML, Stein JP, Lieskovsky G, Cai J, Pinski J, et al. Prognosis of patients with lymph node positive prostate cancer following radical prostatectomy: long-term results. J Urol. 2004;172:2252–5.
Porcaro AB, de Luyk N, Corsi P, Sebben M, Tafuri A, Tamanini I, et al. Bilateral lymph node micrometastases and seminal vesicle invasion associated with same clinical predictors in localized prostate cancer. Tumori .2017;103:299–306.
Pagliarulo V, Hawes D, Brands FH, Groshen S, Cai J, Stein JP, et al. Detection of occult lymph node metastases in locally advanced node-negative prostate cancer. J Clin Oncol. 2006;24:2735–42.
Potter SR, Mangold LA, Shue MJ, Taylor DC, Lecksell KL, Epstein JI, et al. Molecular and immunohistochemical staging of men with seminal vesicle invasion and negative pelvic lymph nodes at radical prostatectomy. Cancer. 2000;89:2577–86.
Badani KK, Reddy BN, Moskowitz EJ, Paulucci DJ, Beksac AT, Martini A, et al. Lymph node yield during radical prostatectomy does not impact rate of biochemical recurrence in patients with seminal vesicle invasion and node-negative disease. Urol Oncol. 2018;36:310.e1–.e6.
DiMarco DS, Zincke H, Sebo TJ, Slezak J, Bergstralh EJ, Blute ML. The extent of lymphadenectomy for pTXNO prostate cancer does not affect prostate cancer outcome in the prostate specific antigen era. J Urol. 2005;173:1121–5.
Fiori C, Checcucci E, Stura I, Amparore D, De Cillis S, Piana A, et al. Development of a novel nomogram to identify the candidate to extended pelvic lymph node dissection in patients who underwent mpMRI and target biopsy only. Prostate Cancer Prostatic Dis. 2023;26:388–94.
Lucciola S, Pisciotti ML, Frisenda M, Magliocca F, Gentilucci A, Del Giudice F, et al. Predictive role of node-rads score in patients with prostate cancer candidates for radical prostatectomy with extended lymph node dissection: comparative analysis with validated nomograms. Prostate Cancer Prostatic Dis. 2023;26:379–87.
Cheng L, Zincke H, Blute ML, Bergstralh EJ, Scherer B, Bostwick DG. Risk of prostate carcinoma death in patients with lymph node metastasis. Cancer. 2001;91:66–73.
Bader P, Burkhard FC, Markwalder R, Studer UE. Disease progression and survival of patients with positive lymph nodes after radical prostatectomy. Is there a chance of cure? J Urol. 2003;169:849–54.
Passoni NM, Abdollah F, Suardi N, Gallina A, Bianchi M, Tutolo M, et al. Head-to-head comparison of lymph node density and number of positive lymph nodes in stratifying the outcome of patients with lymph node-positive prostate cancer submitted to radical prostatectomy and extended lymph node dissection. Urol Oncol. 2014;32:29.e1–8.
Chen MS, Howard LE, Stock S, Dolgner A, Freedland SJ, Aronson W, et al. Validation of the prostate cancer comorbidity index in predicting cause-specific mortality in men undergoing radical prostatectomy. Prostate Cancer Prostatic Dis. 2022. https://doi.org/10.1038/s41391-022-00550-5. [Epub ahead of print].
Bloom KD, Richie JP, Schultz D, Renshaw A, Saegaert T, D’Amico AV. Invasion of seminal vesicles by adenocarcinoma of the prostate: PSA outcome determined by preoperative and postoperative factors. Urology .2004;63:333–6.
Freedland SJ, Aronson WJ, Presti JC Jr, Amling CL, Terris MK, Trock B, et al. Predictors of prostate-specific antigen progression among men with seminal vesicle invasion at the time of radical prostatectomy. Cancer. 2004;100:1633–8.
Rehman A, El-Zaatari ZM, Han SH, Shen SS, Ayala AG, Miles B, et al. Seminal vesicle invasion combined with extraprostatic extension is associated with higher frequency of biochemical recurrence and lymph node metastasis than seminal vesicle invasion alone: Proposal for further pT3 prostate cancer subclassification. Ann Diagn Pathol. 2020;49:151611.
Author information
Authors and Affiliations
Contributions
Protocol / project development: RRP, RN, SB. Data collection or management: LJ. Data analysis: LJR. Manuscript writing / editing: RRP, RN, SB. Other (Interpretation of data and revision): PS, IF, MT, VS, JCC, RJK, and SAB.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Institutional review board approval IRB: 22-009986. The study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41391_2023_724_MOESM1_ESM.docx
Supplementary table: Multivariable Cox regression analyses for metastasis-free survival, cancer-specific survival, and overall survival in 1,241 patients with prostate cancer with concomitant seminal
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rodrigues Pessoa, R., Nabavizadeh, R., Shah, P. et al. Relative impact of lymph-node metastasis and seminal vesical invasion on oncologic outcomes following radical prostatectomy. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00724-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00724-9
This article is cited by
-
Shifting the paradigm in high-risk prostate cancer: how good is TNM alone?
Prostate Cancer and Prostatic Diseases (2023)
-
The relative impact of lymph-node metastasis and seminal vesical invasion on oncologic outcomes following radical prostatectomy
Prostate Cancer and Prostatic Diseases (2023)