Abstract
Purpose
To identify trends, costs, and predictors in the use of different surgical procedures for post-radical prostatectomy incontinence (PPI).
Materials and methods
We identified 21,589 men who were diagnosed with localized prostate cancer (PCa) and treated with radical prostatectomy (RP) from 2003 to 2017. The primary outcome was the incontinence procedure performances. Optum’s de-identified Clinformatics® Data Mart Database was queried to define the cohort of interest. The average costs of the different incontinence procedures were obtained and compared. Also, demographic, and clinical predictors of incontinence surgery were evaluated by multivariable regression analysis.
Results
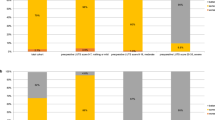
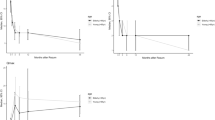
Of the 21,589 men with localized PCa treated with RP, 740 (3.43%) underwent at least one incontinence procedure during a median of 5 years of follow-up. In total, there were 844 unique incontinence procedures. Male slings were the most common procedure (47.5%), had an intermediate cost compared to the other treatment options, and was the first-choice treatment for the majority of patients (50%). The use of an artificial urinary sphincter (AUS) was the second most common (35.3%), but also was the most expensive treatment and was first-choice-treatment for 32.3% of patients. On multivariable analysis, metabolic syndrome related disorders, adjuvant/salvage radiation therapy as well as a history of neurological comorbidities were independently associated with an increased likelihood of incontinence surgery.
Conclusions
The receipt of male slings increased and then subsequently decreased, while AUS utilization was stable, and the use of urethral bulking agents was uncommon. From a cost standpoint, AUS was the most expensive option. Finally, patient’s comorbidity history and RP related factors were found to influence the choice for primary or subsequent PPI interventions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Due to the nature of this code-control research, data are not allowed to be shared publicly, so supporting data are not available.
References
Punnen S, Cowan JE, Chan JM, Carroll PR, Cooperberg MR. Long-term health-related quality of life after primary treatment for localized prostate cancer: results from the CaPSURE registry. Eur Urol. 2015;68:600–8.
Boorjian SA, Eastham JA, Graefen M, Guillonneau B, Karnes RJ, Moul JW, et al. A critical analysis of the long-term impact of radical prostatectomy on cancer control and function outcomes. Eur Urol. 2012;61:664–75.
Penson DF, McLerran D, Feng Z, Li L, Albertsen PC, Gilliland FD, et al. 5-year urinary and sexual outcomes after radical prostatectomy: results from the Prostate Cancer Outcomes Study. J Urol. 2008;179:S40–4.
Sacco E, Prayer-Galetti T, Pinto F, Fracalanza S, Betto G, Pagano F, et al. Urinary incontinence after radical prostatectomy: incidence by definition, risk factors and temporal trend in a large series with a long-term follow-up. BJU Int. 2006;97:1234–41.
Murphy DG, Kerger M, Crowe H, Peters JS, Costello AJ. Operative details and oncological and functional outcome of robotic-assisted laparoscopic radical prostatectomy: 400 cases with a minimum of 12 months follow-up. Eur Urol. 2009;55:1358–66.
Montague DK, Angermeier KW, Paolone DR. Long-term continence and patient satisfaction after artificial sphincter implantation for urinary incontinence after prostatectomy. J Urol. 2001;166:547–9.
James MH, McCammon KA. Artificial urinary sphincter for post-prostatectomy incontinence: a review. Int J Urol. 2014;21:536–43.
Bauer RM, Soljanik I, Fullhase C, Buchner A, May F, Stief CG, et al. Results of the AdVance transobturator male sling after radical prostatectomy and adjuvant radiotherapy. Urology 2011;77:474–9.
Cornu JN, Sebe P, Ciofu C, Peyrat L, Cussenot O, Haab F. Mid-term evaluation of the transobturator male sling for post-prostatectomy incontinence: focus on prognostic factors. BJU Int. 2011;108:236–40.
Bauer RM, Gozzi C, Hubner W, Nitti VW, Novara G, Peterson A, et al. Contemporary management of postprostatectomy incontinence. Eur Urol. 2011;59:985–96.
Optum. Optum integrated data: bring precision to your investment decisions (2014). https://www.optum.com/content/dam/optum3/optum/en/resources/fact-sheets/Integrated-Data-product-sheet.pdf.
Kim PH, Pinheiro LC, Atoria CL, Eastham JA, Sandhu JS, Elkin EB. Trends in the use of incontinence procedures after radical prostatectomy: a population based analysis. J Urol. 2013;189:602–8.
Gupta S, Ding L, Granieri M, Le NB, Peterson AC. Utilization of surgical procedures and racial disparity in the treatment of urinary incontinence after prostatectomy. Neurourol Urodyn. 2016;35:733–7.
Nelson M, Dornbier R, Kirshenbaum E, Eguia E, Sweigert P, Baker M, et al. Use of Surgery for Post-Prostatectomy Incontinence. J Urol. 2020;203:786–91.
MacDonald S, Colaco M, Terlecki R. Waves of Change: National Trends in Surgical Management of Male Stress Incontinence. Urology 2017;108:175–9.
Liu JS, Hofer MD, Milose J, Oberlin DT, Flury SC, Morey AF, et al. Male Sling and Artificial Urethral Sphincter for Male Stress Urinary Incontinence Among Certifying American Urologists. Urology 2016;87:95–9.
Leow JJ, Chang SL, Meyer CP, Wang Y, Hanske J, Sammon JD, et al. Robot-assisted Versus Open Radical Prostatectomy: A Contemporary Analysis of an All-payer Discharge Database. Eur Urol. 2016;70:837–45.
Ficarra V, Novara G, Rosen RC, Artibani W, Carroll PR, Costello A, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol. 2012;62:405–17.
Fossati N, Di Trapani E, Gandaglia G, Dell'Oglio P, Umari P, Buffi NM, et al. Assessing the Impact of Surgeon Experience on Urinary Continence Recovery After Robot-Assisted Radical Prostatectomy: Results of Four High-Volume Surgeons. J Endourol. 2017;31:872–7.
Vora AA, Dajani D, Lynch JH, Kowalczyk KJ. Anatomic and technical considerations for optimizing recovery of urinary function during robotic-assisted radical prostatectomy. Curr Opin Urol. 2013;23:78–87.
Fisher MB, Aggarwal N, Vuruskan H, Singla AK. Efficacy of artificial urinary sphincter implantation after failed bone-anchored male sling for postprostatectomy incontinence. Urology 2007;70:942–4.
Rehder P, Haab F, Cornu JN, Gozzi C, Bauer RM. Treatment of postprostatectomy male urinary incontinence with the transobturator retroluminal repositioning sling suspension: 3-year follow-up. Eur Urol. 2012;62:140–5.
Lim E, Leslie S, Thanigasalam R, Steffens D. To sling or not to sling? Impact of intraoperative sling procedures during radical prostatectomy on postoperative continence outcomes: A systematic review and meta‐analysis. BJUI Compass. 2021;2:226–37.
Peterson AC, Chen Y. Patient reported incontinence after radical prostatectomy is more common than expected and not associated with the nerve sparing technique: results from the Center for Prostate Disease Research (CPDR) database. Neurourol Urodyn. 2012;31:60–3.
Nishikawa M, Watanabe H, Kurahashi T. Impact of metabolic syndrome on early recovery of continence after robot-assisted radical prostatectomy. Int J Urol. 2017;24:692–7.
Wille S, Heidenreich A, von Knobloch R, Hofmann R, Engelmann U. Impact of comorbidities on post-prostatectomy incontinence. Urologia Internationalis. 2006;76:223–6.
Teber D, Sofikerim M, Ates M, Gözen AS, Güven O, Sanli O et al. Is type 2 diabetes mellitus a predictive factor for incontinence after laparoscopic radical prostatectomy? A matched pair and multivariate analysis. J Urol. 2010;183:1087–91.
Cakmak S, Canda AE, Ener K, Atmaca AF, Altinova S, Balbay MD. Does Type 2 Diabetes Mellitus Have an Impact on Postoperative Early, Mid-Term and Late-Term Urinary Continence After Robot-Assisted Radical Prostatectomy? J Endourol. 2019;33:201–6.
Chung BI, Leow JJ, Gelpi-Hammerschmidt F, Wang Y, Del Giudice F, De S, et al. Racial disparities in postoperative complications after radical nephrectomy: a population-based analysis. Urology. 2015;85:1411–6. https://doi.org/10.1016/j.urology.2015.03.001. Epub 2015 Apr 14. PMID: 25881864
Chung KJ, Kim JH, Min GE, Park HK, Li S, Del Giudice F, et al. Changing Trends in the Treatment of Nephrolithiasis in the Real World. J Endourol. 2019;33:248–53. https://doi.org/10.1089/end.2018.0667. Epub 2019 Feb 13. PMID: 30628473
Author information
Authors and Affiliations
Contributions
FDG: Conceptualization, Data curation, Investigation, Methodology, Paper writing, Paper revision. JH: Ppaer writing, Data curation, Investigation. SL: Data curation, formal analysis, Methodology, Software, Validation, Paper editing. SS: Validation. EE: Paper editing, validation, supervision. MM: Methodology, Investigation. SS: Methodology, Investigation, Paper revision. MF: Methodology, Paper revision. FC: Methodology, Paper revision. SDP: Investigation, Paper revision. RA: Supervision, Paper revision. WK: Supervision, Paper revision. SC: Supervision, Paper revision. GEC: Supervision, Paper revision. EB: Paper revision, validation. VA: Paper revision, validation. CS: Paper revision. MM: Supervision. DD’A: Supervision. DRB: Validation. BIC: Conceptualization, Supervision, Paper writing, Paper editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Del Giudice, F., Huang, J., Li, S. et al. Contemporary trends in the surgical management of urinary incontinence after radical prostatectomy in the United States. Prostate Cancer Prostatic Dis 26, 367–373 (2023). https://doi.org/10.1038/s41391-022-00558-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00558-x
This article is cited by
-
Editorial: new horizons in robotic platforms
Prostate Cancer and Prostatic Diseases (2024)
-
The significance of transrectal ultrasound and urologist_dually guided pelvic floor muscle exercise in improving urinary continence after radical prostatectomy
European Journal of Medical Research (2023)
-
Prevalence of lower urinary tract symptoms in taxi drivers: a cross-sectional web-based survey
Prostate Cancer and Prostatic Diseases (2023)
-
Robotic assisted simple prostatectomy versus other treatment modalities for large benign prostatic hyperplasia: a systematic review and meta-analysis of over 6500 cases
Prostate Cancer and Prostatic Diseases (2023)
-
Insufficient utilization of care in male incontinence surgery: health care reality in Germany from 2006 to 2020 and a systematic review of the international literature
World Journal of Urology (2023)