Abstract
Background
Many factors are implicated in the potential ‘under-treatment’ of prostate cancer but little is known about the between-hospital variation.
Methods
The National Prostate Cancer Audit (NPCA) database was used to identify high-risk localised or locally advanced prostate cancer patients in England, between January 2014 and December 2017, and the treatments received. Hospital-level variation in radical local treatment was explored visually using funnel plots. The intra-class correlation coefficient (ICC) quantified the between-hospital variation in a random-intercept multivariable logistic regression model.
Results
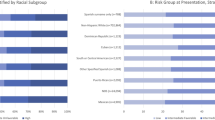
53,888 men, from 128 hospitals, were included and 35,034 (65.0%) received radical local treatment. The likelihood of receiving radical local treatment was increased in men who were younger (the strongest predictor), more affluent, those with fewer comorbidities, and in those with a non-Black ethnic background. There was more between-hospital variation (P < 0.001) for patients aged ≥80 years (ICC: 0.235) compared to patients aged 75–79 years (ICC: 0.070), 70–74 years (ICC: 0.041), and <70 years (ICC: 0.048). Comorbidity and socioeconomic deprivation did not influence the between-hospital variation.
Conclusions
Radical local treatment of high-risk localised or locally advanced prostate cancer depended strongly on age and comorbidity, but also on socioeconomic deprivation and ethnicity, with the between-hospital variation being highest in older patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The cancer registry data used for this study are based on information collected and quality assured by Public Health England’s National Cancer Registration Service (www.ncras.nhs.uk). Access to the data was facilitated by the Public Health England’s Office for Data Release. Hospital Episode Statistics were made available by the NHS Digital (www.digital.nhs.uk); all rights reserved. MGP had full access to all the data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis. Data are not available to other researchers as it uses existing national data sets.
References
National Prostate Cancer Audit. Annual Report 2019: Results of the NPCA prospective audit in England and Wales for men diagnosed from 1 April 2017–31 March 2018. 2019. https://www.npca.org.uk/reports/npca-annual-report-2019/.
European Association of Urology. Guidelines on prostate cancer. 2017. http://uroweb.org/guideline/prostate-cancer/.
Cooperberg MR, Broering JM, Carroll PR. Time trends and local variation in primary treatment of localized prostate cancer. J Clin Oncol. 2010;28:1117–23.
Denberg TD, Glode LM, Steiner JF, Crawford ED, Hoffman RM. Trends and predictors of aggressive therapy for clinical locally advanced prostate carcinoma. BJU Int. 2006;98:335–40.
Lowrance WT, Elkin EB, Yee DS, Feifer A, Ehdaie B, Jacks LM, et al. Locally advanced prostate cancer: a population-based study of treatment patterns. BJU Int. 2012;109:1309–14.
Meltzer D, Egleston B, Abdalla I. Patterns of prostate cancer treatment by clinical stage and age. Am J Public Health. 2001;91:126–8.
National Prostate Cancer Audit. Third year annual report—Results of the NPCA prospective audit and patient survey. 2016. https://www.npca.org.uk/content/uploads/2017/11/NPCA-2016-Annual-Report-Final_131216.pdf.
NHS Digital. Hospital Episode Statistics (HES). 2021. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics.
National Cancer Registration and Analysis Service. National Radiotherapy Dataset (RTDS). 2010. https://www.ncin.org.uk/collecting_and_using_data/rtds.
Brierley J, Gospodarowicz M, Wittekind C. TNM classification of malignant tumours. 8th edn. Chichester: John Wiley & Sons; 2017.
Noble M, McLennan D, Wilkinson K, Whitworth A, Dibben C, Barnes H. The English indices of deprivation 2007. 2008. http://geoconvert.mimas.ac.uk/help/imd-2007-manual.pdf.
Public Health England. Cancer registration data dictionary. 2020. https://www.gov.uk/government/publications/accessing-public-health-england-data.
Armitage JN, van der Meulen JH. Identifying co-morbidity in surgical patients using administrative data with the Royal College of Surgeons Charlson Score. Br J Surg. 2010;97:772–81.
Ministry of Housing CLG. English indices of deprivation 2015. 2015. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015.
NHS Digital. NHS Classifications Service: OPCS Classifications of Interventions and Procedures Version 4.4. 2007. http://systems.digital.nhs.uk/data/clinicalcoding/codingstandards/opcs4.
Knol MJ, Le Cessie S, Algra A, Vandenbroucke JP, Groenwold RH. Overestimation of risk ratios by odds ratios in trials and cohort studies: alternatives to logistic regression. CMAJ 2012;184:895–9.
Gutierrez RG. Parametric frailty and shared frailty survival models. Stata J. 2002;2:22–44.
Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley and Sons; 2004.
Spiegelhalter DJ. Funnel plots for comparing institutional performance. Stat Med. 2005;24:1185–202.
Pietro GD, Chornokur G, Kumar NB, Davis C, Park JY. Racial differences in the diagnosis and treatment of prostate cancer. Int Neurourol J. 2016;20(Suppl 2):S112–9.
Fung C, Dale W, Mohile SG. Prostate cancer in the elderly patient. J Clin Oncol. 2014;32:2523–30.
Boyle HJ, Alibhai S, Decoster L, Efstathiou E, Fizazi K, Mottet N, et al. Updated recommendations of the International Society of Geriatric Oncology on prostate cancer management in older patients. Eur J Cancer. 2019;116:116–36.
Daskivich TJ, Fan KH, Koyama T, Albertsen PC, Goodman M, Hamilton AS, et al. Effect of age, tumor risk, and comorbidity on competing risks for survival in a U.S. population-based cohort of men with prostate cancer. Ann Intern Med. 2013;158:709–17.
Kutikov A, Cooperberg MR, Paciorek AT, Uzzo RG, Carroll PR, Boorjian SA. Evaluating prostate cancer mortality and competing risks of death in patients with localized prostate cancer using a comprehensive nomogram. Prostate Cancer Prostatic Dis. 2012;15:374–9.
Hoffman RM, Koyama T, Albertsen PC, Barry MJ, Daskivich TJ, Goodman M, et al. Self-reported health status predicts other-cause mortality in men with localized prostate cancer: results from the prostate cancer outcomes study. J Gen Intern Med. 2015;30:924–34.
Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE. Understanding of regional variation in the use of surgery. Lancet 2013;382:1121–9.
Boyle JM, Kuryba A, Cowling TE, Aggarwal A, Hill J, van der Meulen J, et al. Determinants of variation in the use of adjuvant chemotherapy for stage III colon cancer in England. Clin Oncol. 2020;32:e135–44.
Benitez Majano S, Di Girolamo C, Rachet B, Maringe C, Guren MG, Glimelius B, et al. Surgical treatment and survival from colorectal cancer in Denmark, England, Norway, and Sweden: a population-based study. Lancet Oncol. 2019;20:74–87.
Puts MT, Tapscott B, Fitch M, Howell D, Monette J, Wan-Chow-Wah D, et al. A systematic review of factors influencing older adults’ decision to accept or decline cancer treatment. Cancer Treat Rev. 2015;41:197–215.
Barbiere JM, Greenberg DC, Wright KA, Brown CH, Palmer C, Neal DE, et al. The association of diagnosis in the private or NHS sector on prostate cancer stage and treatment. J Public Health. 2012;34:108–14.
Burns EM, Rigby E, Mamidanna R, Bottle A, Aylin P, Ziprin P, et al. Systematic review of discharge coding accuracy. J Public Health. 2012;34:138–48.
Acknowledgements
We thank NHS staff for their support in collecting the clinical data, the National Cancer Registration and Analysis Service (www.ncras.nhs.uk) for providing cancer registry and radiotherapy data and NHS Digital (www.digital.nhs.uk) for providing Hospital Episode Statistics. MGP, JN, MM, TC, AS, BB, PC, NWC, HP, AA and JvdM are members of the Project Team of the National Prostate Cancer Audit (www.npca.org.uk). The National Prostate Cancer Audit is commissioned by the Healthcare Quality Improvement Partnership (www.hqip.org.uk) as part of the National Clinical Audit and Patient Outcomes Programme, and funded by NHS England and the Welsh Government. Neither HQIP nor NHS England or the Welsh Government had any involvement in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. The researchers had full independence from the Healthcare Quality Improvement Partnership.
Funding
MGP was supported by a Doctoral Research Fellowship from the National Institute for Health Research (DRF-2018-11-ST2-036). BB was partly supported by an Academic Clinical Fellowship from the National Institute for Health Research. HP was supported by the University College London Hospitals/University College London Comprehensive Biomedical Research Centre. JvdM was partly supported by the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care North Thames. The views expressed in this article are solely those of the authors.
Author information
Authors and Affiliations
Contributions
Designed the work: MGP, JvdM, HP and NWC. Analysed and interpreted data: MGP, JMB, JvdM, HP and NWC. Drafted article: MGP, JvdM, HP and NWC. Provided critical revision: All authors. Approved final version to be published: All authors.
Corresponding author
Ethics declarations
Competing interests
JvdM reports a contract with the Healthcare Quality Improvement Partnership for the provision of the National Prostate Cancer Audit (www.npca.org.uk) funded by the Healthcare Quality Improvement Partnership (www.hqip.org.uk). HP has attended and received honoraria for advisory boards, travel expenses to medical meetings, and served as a consultant for AstraZeneca, Astellas, Janssen, Sanofi Aventis, Takeda, Ipsen, Ferring, Sandoz, and Novartis. NWC has attended and received honoraria for advisory boards, travel expenses to medical meetings, and served as a consultant for AstraZeneca, Astellas, Bayer, Janssen, Sanofi Aventis, Takeda, Ipsen and Ferring.
Ethics approval and consent to participate
This study was exempt from NHS Research Ethics Committee approval because it involved analysis of pseudonymised linked data collated for the purpose of service evaluation as part of the National Prostate Cancer Audit.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Parry, M.G., Boyle, J.M., Nossiter, J. et al. Determinants of variation in radical local treatment for men with high-risk localised or locally advanced prostate cancer in England. Prostate Cancer Prostatic Dis 26, 257–263 (2023). https://doi.org/10.1038/s41391-021-00439-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-021-00439-9
This article is cited by
-
Geographic and socioeconomic variation in treatment of elderly prostate cancer patients in Norway – a national register-based study
Research in Health Services & Regions (2024)
-
Can PROMs improve racial equity in outcomes after prostatectomy?
Nature Reviews Urology (2023)