Abstract
Background
Physical activity (PA) is associated with favorable outcomes in prostate cancer (PCa) patients. We assessed its effect on the risk of PCa reclassification (PCaR) during active surveillance.
Methods
Anthropometric, demographic, and clinical data concerning men diagnosed with a low-risk PCa and initially managed with active surveillance at the two participating institutions were retrospectively collected. The Physical Activity Scale for the Elderly (PASE) was used for patients’ self-assessment of their daily exercise and their consequent stratification into three groups: sedentary (PASE ≤ 65), moderately active (65 < PASE < 125), active (PASE ≥ 125). Kaplan–Meier model was used to evaluate the predictive role of PA on PCaR, computed at 2, 5, 10 years after diagnosis; differences between lifestyle groups were assessed using the log-rank and uni-/multivariable Cox analyses applied to identify predictors of reclassification.
Results
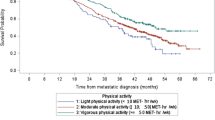
Eighty-five patients were included in the analysis, with a median age of 66 years (IQR: 59–70); 16% were active, 45% were former smokers, and 3 presented with metabolic syndrome (MetS). Prostate-specific antigen (PSA) density was 0.12 (IQR: 0.07–0.15); 34 men showed a PSA doubling time <10 years. The Median PASE score was 86 (IQR: 61.5–115.8): 24 patients were sedentary, 46 moderately active, and 15 active. At a median follow-up of 37 months (IQR: 14–53), 25% of patients experienced PCaR. These were less physically active (PASE score 69.3 vs 87.8; p = 0.056) and presented with significantly smaller prostates (46 ml vs 50.7 ml; p = 0.001) and a higher PSAD (0.14 vs 0.10; p = 0.019). At 2 years, the risk of reclassification was 25 ± 5%, while it was 38 ± 7% at both 5 and 10 years. The risk was significantly different in the three PA groups (Log Rank p = 0.033). PASE score was the only independent predictor of PCaR (HR: 0.987; 95%CI: 0.977–0.998; p = 0.016).
Conclusions
PA influences PCa evolution, as increasing levels are associated with a significantly reduced risk of tumor reclassification among patients undergoing active surveillance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30. https://doi.org/10.3322/caac.21590
Loeb S, Bjurlin MA, Nicholson J, Tammela TL, Penson DF, Carter HB, et al. Overdiagnosis and overtreatment of prostate cancer. Eur Urol. 2014;65:1046–55. https://doi.org/10.1016/j.eururo.2013.12.062
Bacon CG, Giovannucci E, Testa M, Glass TA, Kawachi I. The association of treatment-related symptoms with quality-of-life outcomes for localized prostate carcinoma patients. Cancer. 2002;94:862–71. https://doi.org/10.1002/cncr.10248
Cooperberg MR. Active surveillance for low-risk prostate cancer—an evolving international standard of care. JAMA Oncol. 2017;3:1398–9. https://doi.org/10.1001/jamaoncol.2016.3179
Klotz L. Active surveillance for low-risk prostate cancer. Curr Urol Rep. 2015;16:1–10. https://doi.org/10.1007/s11934-015-0492-z
Sharma V, Wymer KM, Borah BJ, Barocas DA, Thompson RH, Karnes RJ, et al. Cost-effectiveness of active surveillance, radical prostatectomy and external beam radiotherapy for localized prostate cancer: an analysis of the protect trial. J Urol. 2019;202:964–72. https://doi.org/10.1097/JU.0000000000000345
Papadopoulos E, Alibhai SMH, Tomlinson GA, Matthew AG, Nesbitt M, Finelli A, et al. Influence of physical activity on active surveillance discontinuation in men with low-risk prostate cancer. Cancer Causes Control. 2019;30:1009–12. https://doi.org/10.1007/s10552-019-01211-0
Guy DE, Vandersluis A, Klotz LH, Fleshner N, Kiss A, Parker C, et al. Total energy expenditure and vigorous-intensity physical activity are associated with reduced odds of reclassification among men on active surveillance. Prostate Cancer Prostatic Dis. 2018;21:187–95. https://doi.org/10.1038/s41391-017-0010-0
Vandersluis AD, Guy DE, Klotz LH, Fleshner NE, Kiss A, Parker C, et al. The role of lifestyle characteristics on prostate cancer progression in two active surveillance cohorts. Prostate Cancer Prostatic Dis. 2016;19:305–10. https://doi.org/10.1038/pcan.2016.22
Ornish D, Weidner G, Fair WR, Marlin R, Pettengill EB, Raisin CJ, et al. Intensive lifestyle changes may affect the progression of prostate cancer. J Urol. 2005;174:1065–70. https://doi.org/10.1097/01.ju.0000169487.49018.73
Frattaroli J, Weidner G, Dnistrian AM, Kemp C, Daubenmier JJ, Marlin RO, et al. Clinical events in prostate cancer lifestyle trial: results from two years of follow-up. Urology. 2008;72:1319–23. https://doi.org/10.1016/j.urology.2008.04.050
van den Bergh RCN, Roemeling S, Roobol MJ, Roobol W, Schröder FH, Bangma CH. Prospective validation of active surveillance in prostate cancer: the PRIAS study. Eur Urol. 2007;52:1560–3. https://doi.org/10.1016/j.eururo.2007.05.011
Washburn RA, Smith KW, Jette AM, Janney CA. The physical activity scale for the elderly (PASE): Development and evaluation. J Clin Epidemiol. 1993;46:153–62. https://doi.org/10.1016/0895-4356(93)90053-4
Wekesa A, Harrison M, Watson RW. Physical activity and its mechanistic effects on prostate cancer. Prostate Cancer Prostatic Dis. 2015;18:197–207. https://doi.org/10.1038/pcan.2015.9
Kenfield SA, Stampfer MJ, Giovannucci E, Chan JM. Physical activity and survival after prostate cancer diagnosis in the health professionals follow-up study. J Clin Oncol. 2011;29:726–32. https://doi.org/10.1200/JCO.2010.31.5226
Van Blarigan EL, Gerstenberger JP, Kenfield SA, Giovannucci EL, Stampfer MJ, Jones LW, et al. Physical activity and prostate tumor vessel morphology: Data from the health professionals follow-up study. Cancer Prev Res. 2015;8:962–7. https://doi.org/10.1158/1940-6207.CAPR-15-0132
Friedenreich CM, Wang Q, Neilson HK, Kopciuk KA, McGregor SE, Courneya KS. Physical activity and survival after prostate cancer. Eur Urol. 2016;70:576–85. https://doi.org/10.1016/j.eururo.2015.12.032
Wang Y, Jacobs EJ, Gapstur SM, Maliniak ML, Gansler T, McCullough ML, et al. Recreational physical activity in relation to prostate cancer-specific mortality among men with nonmetastatic prostate cancer. Eur Urol. 2017;72:931–9. https://doi.org/10.1016/j.eururo.2017.06.037
Bonn SE, Sjölander A, Lagerros YT, Wiklund F, Stattin P, Holmberg E, et al. Physical activity and survival among men diagnosed with prostate cancer. Cancer Epidemiol Biomark Prev. 2015;24:57–64. https://doi.org/10.1158/1055-9965.EPI-14-0707
Ornish D, Lin J, Chan JM, Epel E, Kemp C, Weidner G, et al. Effect of comprehensive lifestyle changes on telomerase activity and telomere length in men with biopsy-proven low-risk prostate cancer: 5-year follow-up of a descriptive pilot study. Lancet Oncol. 2013;14:1112–20. https://doi.org/10.1016/S1470-2045(13)70366-8
Ornish D, Magbanua MJM, Weidner G, Weinberg V, Kemp C, Green C, et al. Changes in prostate gene expression in men undergoing an intensive nutrition and lifestyle intervention. Proc Natl Acad Sci USA. 2008;105:8369–74. https://doi.org/10.1073/pnas.0803080105
Magbanua MJM, Richman EL, Sosa EV, Jones LW, Simko J, Shinohara K, et al. Physical activity and prostate gene expression in men with low-risk prostate cancer. Cancer Causes Control. 2014;25:515–23. https://doi.org/10.1007/s10552-014-0354-x
Schenk JM, Neuhouser ML, Beatty SJ, VanDoren M, Lin DW, Porter M, et al. Randomized trial evaluating the role of weight loss in overweight and obese men with early stage prostate cancer on active surveillance: rationale and design of the Prostate Cancer Active Lifestyle Study (PALS). Contemp Clin Trials. 2019;81:34–9. https://doi.org/10.1016/j.cct.2019.04.004
De Nunzio C, Nacchia A, Cicione A, Cindolo L, Gacci M, Cancrini F, et al. Physical activity as a protective factor for lower urinary tract symptoms in male patients: a prospective cohort analysis. Urology. 2019;125:163–8. https://doi.org/10.1016/j.urology.2018.12.035
De Nunzio C, Presicce F, Lombardo R, Cancrini F, Petta S, Trucchi A, et al. Physical activity as a risk factor for prostate cancer diagnosis: a prospective biopsy cohort analysis. BJU Int. 2016;117:E29–35. https://doi.org/10.1111/bju.13157
De Nunzio C, Brassetti A, Proietti F, Deroma M, Esperto F, Tubaro A. Metabolic syndrome and smoking are associated with an increased risk of nocturia in male patients with benign prostatic enlargement. Prostate Cancer Prostatic Dis. 2018;21:287–92. https://doi.org/10.1038/s41391-017-0003-z
Peisch SF, Van Blarigan EL, Chan JM, Stampfer MJ, Kenfield SA. Prostate cancer progression and mortality: a review of diet and lifestyle factors. World J Urol. 2017;35:867–74. https://doi.org/10.1007/s00345-016-1914-3
Burton AJ, Martin RM, Donovan JL, Lane JA, Davis M, Hamdy FC, et al. Associations of lifestyle factors and anthropometric measures with repeat PSA levels during active surveillance/monitoring. Cancer Epidemiol Biomark Prev. 2012;21:1877–85. https://doi.org/10.1158/1055-9965. EPI-12-0411
Salinas CA, Tsodikov A, Ishak-Howard M, Cooney KA. Prostate cancer in young men: an important clinical entity. Nat Rev Urol. 2014;11:317–23. https://doi.org/10.1038/nrurol.2014.91
Brassetti A, Lombardo R, Emiliozzi P, Cardi A, Antonio DV, Antonio I, et al. Prostate-specific antigen density is a good predictor of upstaging and upgrading, according to the new grading system: the keys we are seeking may be already in our pocket. Urology. 2017;111:129–35. https://doi.org/10.1016/j.urology.2017.07.071
Leinwand GZ, Gabrielson AT, Krane LS, Silberstein JL. Rethinking active surveillance for prostate cancer in African American men. Transl Androl Urol. 2018;7:S397–410. https://doi.org/10.21037/tau.2018.06.19
Welty CJ, Cowan JE, Nguyen H, Shinohara K, Perez N, Greene KL, et al. Extended followup and risk factors for disease reclassification in a large active surveillance cohort for localized prostate cancer. J Urol. 2015;193:807–11. https://doi.org/10.1016/j.juro.2014.09.094
De Nunzio C, Brassetti A, Simone G, Lombardo R, Mastroianni R, Collura D, et al. Metabolic syndrome increases the risk of upgrading and upstaging in patients with prostate cancer on biopsy: a radical prostatectomy multicenter cohort study. Prostate Cancer Prostatic Dis. 2018;21:438–45. https://doi.org/10.1038/s41391-018-0054-9
De Nunzio C, Simone G, Brassetti A, Mastroianni R, Collura D, Muto G, et al. Metabolic syndrome is associated with advanced prostate cancer in patients treated with radical retropubic prostatectomy: Results from a multicentre prospective study. BMC Cancer. 2016;16:407 https://doi.org/10.1186/s12885-016-2442-7
Colicchia M, Morlacco A, Rangel LJ, Carlson RE, Dal Moro F, Karnes RJ, et al. Role of metabolic syndrome on perioperative and oncological outcomes at radical prostatectomy in a low-risk prostate cancer cohort potentially eligible for active surveillance. 2017. https://doi.org/10.1016/j.euf.2017.12.005
Author information
Authors and Affiliations
Contributions
AB, MF, GN, RS, GT, UA, AB, LM, RM, and FP collected data while FB managed them. AB carried out statistical analysis and drafted the manuscript. MG and GS critically reviewed the paper. All authors have read and approved the final article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval and consent to participate
The retrospective study was performed in accordance with the Declaration of Helsinki. Review board approval was acquired; informed consent for the retrospective study was obtained from all the participants.
Informed consent
Informed consent for the submission and publication of the study was obtained from all individual participants included.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brassetti, A., Ferriero, M., Napodano, G. et al. Physical activity decreases the risk of cancer reclassification in patients on active surveillance: a multicenter retrospective study. Prostate Cancer Prostatic Dis 24, 1151–1157 (2021). https://doi.org/10.1038/s41391-021-00375-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-021-00375-8
This article is cited by
-
Working hard or hardly working? A brief commentary of latest research on exercise and prostate cancer
Prostate Cancer and Prostatic Diseases (2023)
-
Effects of supervised high-intensity interval training on motivational outcomes in men with prostate cancer undergoing active surveillance: results from a randomized controlled trial
International Journal of Behavioral Nutrition and Physical Activity (2022)
-
More evidence that physical activity is beneficial for prostate cancer
Prostate Cancer and Prostatic Diseases (2022)