Abstract
Background
Benign prostatic hyperplasia (BPH) is common noncancerous prostate enlargement, which is usually associated with lower urinary tract symptoms (LUTS) and can lead to complex urinary, bladder, or kidney diseases. The majority of elderly men will be affected by BPH as age increases.
Methods
Here, we conducted a genome-wide association study (GWAS) of BPH using 1942 cases and 4730 controls from the Electronic Medical Records and Genomics network (eMERGE) as discovery cohort. We then used 5109 cases and 161,911 controls from UK Biobank as validation cohort.
Results
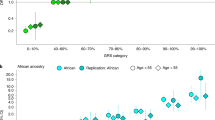
This GWAS discovered 35 genome-wide significant variants (P < 5 × 10−8), located at 22 different loci in discovery cohort. We validated four significant variants located at four different loci in validation cohort: rs8027714 at 15q11.2, rs8136152 at 22q13.2, rs10192133 at 2q24.2, and rs1237696 at 11q22.1. rs1237696 is an intronic variant on chromosome 11 in the progesterone receptor (PGR) gene (P = 4.21 ×10–8, OR [95% CI] = 1.36 [1.22–1.52]). PGR is a known drug target for BPH as the PGR agonist gestonorone caproate has been used to treat BPH in multiple countries.
Conclusions
Our results suggest that genetic variants identified from BPH GWAS can identify pharmacologic targets for BPH treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132:474–9.
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–602.
Sarma AV, Wei JT. Clinical practice. Benign prostatic hyperplasia and lower urinary tract symptoms. N Engl J Med. 2012;367:248–57.
Egan KB. The epidemiology of benign prostatic hyperplasia associated with lower urinary tract symptoms: prevalence and incident rates. Urologic Clin North Am. 2016;43:289–97.
Rodriguez-Nieves JA, Macoska JA. Prostatic fibrosis, lower urinary tract symptoms, and BPH. Nat Rev Urol. 2013;10:546–50.
Kim EH, Larson JA, Andriole GL. Management of benign prostatic hyperplasia. Annu Rev Med. 2016;67:137–51.
Nadler RB, Humphrey PA, Smith DS, Catalona WJ, Ratliff TL. Effect of inflammation and benign prostatic hyperplasia on elevated serum prostate specific antigen levels. J Urol. 1995;154:407–13.
Vickers AJ, Cronin AM, Bjork T, Manjer J, Nilsson PM, Dahlin A, et al. Prostate specific antigen concentration at age 60 and death or metastasis from prostate cancer: case-control study. BMJ. 2010;341:c4521.
Chang RT, Kirby R, Challacombe BJ. Is there a link between BPH and prostate cancer? Practitioner. 2012;256:13–6, 2.
Gudmundsson J, Sigurdsson JK, Stefansdottir L, Agnarsson BA, Isaksson HJ, Stefansson OA, et al. Genome-wide associations for benign prostatic hyperplasia reveal a genetic correlation with serum levels of PSA. Nat Commun. 2018;9:4568.
Suzuki S, Platz EA, Kawachi I, Willett WC, Giovannucci E. Intakes of energy and macronutrients and the risk of benign prostatic hyperplasia. Am J Clin Nutr. 2002;75:689–97.
Gacci M, Corona G, Vignozzi L, Salvi M, Serni S, De Nunzio C, et al. Metabolic syndrome and benign prostatic enlargement: a systematic review and meta-analysis. BJU Int. 2015;115:24–31.
Bartsch G, Rittmaster RS, Klocker H. Dihydrotestosterone and the concept of 5alpha-reductase inhibition in human benign prostatic hyperplasia. Eur Urol. 2000;37:367–80.
Neuhouser ML, Kristal AR, Penson DF. Steroid hormones and hormone-related genetic and lifestyle characteristics as risk factors for benign prostatic hyperplasia: review of epidemiologic literature. Urology. 2004;64:201–11.
Rohrmann S, Giovannucci E, Smit E, Platz EA. Association of IGF-1 and IGFBP-3 with lower urinary tract symptoms in the third national health and nutrition examination survey. Prostate. 2007;67:1693–8.
St Sauver JL, Sarma AV, Jacobson DJ, McGree ME, Lieber MM, Girman CJ, et al. Associations between C-reactive protein and benign prostatic hyperplasia/lower urinary tract symptom outcomes in a population-based cohort. Am J Epidemiol. 2009;169:1281–90.
St Sauver JL, Jacobson DJ, McGree ME, Lieber MM, Jacobsen SJ. Protective association between nonsteroidal antiinflammatory drug use and measures of benign prostatic hyperplasia. Am J Epidemiol. 2006;164:760–8.
St Sauver JL, Jacobson DJ, McGree ME, Girman CJ, Lieber MM, Jacobsen SJ. Longitudinal association between prostatitis and development of benign prostatic hyperplasia. Urology. 2008;71:475–9.
Kristal AR, Arnold KB, Schenk JM, Neuhouser ML, Weiss N, Goodman P, et al. Race/ethnicity, obesity, health related behaviors and the risk of symptomatic benign prostatic hyperplasia: results from the prostate cancer prevention trial. J Urol. 2007;177:1395–400.
Giovannucci E, Rimm EB, Chute CG, Kawachi I, Colditz GA, Stampfer MJ, et al. Obesity and benign prostatic hyperplasia. Am J Epidemiol. 1994;140:989–1002.
Sarma AV, St Sauver JL, Hollingsworth JM, Jacobson DJ, McGree ME, Dunn RL, et al. Diabetes treatment and progression of benign prostatic hyperplasia in community-dwelling black and white men. Urology. 2012;79:102–8.
Parsons JK, Im R. Alcohol consumption is associated with a decreased risk of benign prostatic hyperplasia. J Urol. 2009;182:1463–8.
Platz EA, Kawachi I, Rimm EB, Colditz GA, Stampfer MJ, Willett WC, et al. Physical activity and benign prostatic hyperplasia. Arch Intern Med. 1998;158:2349–56.
Hellwege JN, Stallings S, Torstenson ES, Carroll R, Borthwick KM, Brilliant MH, et al. Heritability and genome-wide association study of benign prostatic hyperplasia (BPH) in the eMERGE network. Sci Rep. 2019;9:6077.
Giri A, Edwards TL, Motley SS, Byerly SH, Fowke JH. Genetic determinants of metabolism and benign prostate enlargement: associations with prostate volume. PLoS ONE. 2015;10:e0132028.
Na R, Helfand BT, Chen H, Conran CA, Crawford SE, Hayward SW, et al. A genetic variant near GATA3 implicated in inherited susceptibility and etiology of benign prostatic hyperplasia (BPH) and lower urinary tract symptoms (LUTS). Prostate. 2017;77:1213–20.
Verma SS, de Andrade M, Tromp G, Kuivaniemi H, Pugh E, Namjou-Khales B, et al. Imputation and quality control steps for combining multiple genome-wide datasets. Front Genet. 2014;5:370.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
Hoffmann TJ, Passarelli MN, Graff RE, Emami NC, Sakoda LC, Jorgenson E, et al. Genome-wide association study of prostate-specific antigen levels identifies novel loci independent of prostate cancer. Nat Commun. 2017;8:14248.
Depostat for benign prostatic hyperplasia? Drug Therap Bull. 1973;11:75–6.
Aubrey DA, Khosla T. The effect of 17-alpha-hydroxy-19-norprogesterone caproate (SH582) on benign prostatic hypertrophy. The. Br J Surg. 1971;58:648–52.
Watanabe H, Kaiho H, Takahashi H, Kato T, Shima M. [Effects of 17-alpha-hydroxy-19-norprogesterone acaproate (SH-582) on prostatic hypertrophy with special reference to estimation of size of the prostate by means of ultrasonotomography]. Hinyokika kiyo Acta urologica Japonica. 1970;16:438–45.
Ochiai K, Komase M, Oshima H, Negishi T, Yamauchi A. [Effects of SH 582 (gestonorone caproate) for prostatic hypertrophy]. Hinyokika kiyo Acta urologica Japonica. 1970;16:473–81.
Yu Y, Lee JS, Xie N, Li E, Hurtado-Coll A, Fazli L, et al. Prostate stromal cells express the progesterone receptor to control cancer cell mobility. PLoS ONE. 2014;9:e92714.
Chen R, Yu Y, Dong X. Progesterone receptor in the prostate: a potential suppressor for benign prostatic hyperplasia and prostate cancer. J Steroid Biochem Mol Biol. 2017;166:91–6.
Grindstad T, Richardsen E, Andersen S, Skjefstad K, Rakaee Khanehkenari M, Donnem T, et al. Progesterone receptors in prostate cancer: progesterone receptor B is the isoform associated with disease progression. Sci Rep. 2018;8:11358.
Song L, Shen W, Zhang H, Wang Q, Wang Y, Zhou Z. Differential expression of androgen, estrogen, and progesterone receptors in benign prostatic hyperplasia. Bosn J Basic Med Sci. 2016;16:201–8.
GTEx Consortium. Genetic effects on gene expression across human tissues. Nature. 2017;550:204–13.
Meiraz D, Margolin Y, Lev-Ran A, Lazebnik J. Treatment of benign prostatic hyperplasia with hydroxyprogesterone-caproate: placebo-controlled study. Urology. 1977;9:144–8.
Neumann LC, Markaki Y, Mladenov E, Hoffmann D, Buiting K, Horsthemke B. The imprinted NPAP1/C15orf2 gene in the Prader-Willi syndrome region encodes a nuclear pore complex associated protein. Hum Mol Genet. 2012;21:4038–48.
Fortner RT, Katzke V, Kuhn T, Kaaks R. Obesity and breast cancer. Recent results Cancer Res. Fortschr der Krebsforsch Prog dans les Rech sur le cancer. 2016;208:43–65.
Mauland KK, Trovik J, Wik E, Raeder MB, Njolstad TS, Stefansson IM, et al. High BMI is significantly associated with positive progesterone receptor status and clinico-pathological markers for non-aggressive disease in endometrial cancer. Br J Cancer. 2011;104:921–6.
Vincze B, Kapuvari B, Udvarhelyi N, Horvath Z, Matrai Z, Czeyda-Pommersheim F, et al. Serum estrone concentration, estrone sulfate/estrone ratio and BMI are associated with human epidermal growth factor receptor 2 and progesterone receptor status in postmenopausal primary breast cancer patients suffering invasive ductal carcinoma. SpringerPlus. 2015;4:387.
Ohara M, Akimoto E, Noma M, Matsuura K, Doi M, Kagawa N, et al. Prognostic impact of progesterone receptor status combined with body mass index in breast cancer patients treated with adjuvant aromatase inhibitor. Oncol Lett. 2015;10:3286–92.
Oudanonh T, Nabi H, Ennour-Idrissi K, Lemieux J, Diorio C. Progesterone receptor status modifies the association between body mass index and prognosis in women diagnosed with estrogen receptor positive breast cancer. Int J Cancer. 2020;146:2736–45.
Yanai A, Miyagawa Y, Murase K, Imamura M, Yagi T, Ichii S, et al. Influence of body mass index on clinicopathological factors including estrogen receptor, progesterone receptor, and Ki67 expression levels in breast cancers. Int J Clin Oncol. 2014;19:467–72.
Gottesman O, Kuivaniemi H, Tromp G, Faucett WA, Li R, Manolio TA, et al. The Electronic Medical Records and Genomics (eMERGE) Network: past, present, and future. Genet Med: Off J Am Coll Med Genet. 2013;15:761–71.
McCarty CA, Chisholm RL, Chute CG, Kullo IJ, Jarvik GP, Larson EB, et al. The eMERGE Network: a consortium of biorepositories linked to electronic medical records data for conducting genomic studies. BMC Med Genomics. 2011;4:13.
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81:559–75.
Delaneau O, Marchini J, Zagury JF. A linear complexity phasing method for thousands of genomes. Nat Methods. 2011;9:179–81.
Howie BN, Donnelly P, Marchini J. A flexible and accurate genotype imputation method for the next generation of genome-wide association studies. PLoS Genet. 2009;5:e1000529.
Li W, Middha M, Bicak M, Sjoberg DD, Vertosick E, Dahlin A, et al. Genome-wide scan identifies role for AOX1 in prostate cancer survival. Eur Urol. 2018;74:710–9.
Price AL, Patterson NJ, Plenge RM, Weinblatt ME, Shadick NA, Reich D. Principal components analysis corrects for stratification in genome-wide association studies. Nat Genet. 2006;38:904–9.
Acknowledgements
Work in the Klein lab is supported by the National Cancer Institute (R01 CA175491). This work was supported in part through the computational resources and staff expertize provided by Scientific Computing at the Icahn School of Medicine at Mount Sinai, including infrastructure supported by the Office of Research Infrastructure of the National Institutes of Health under award number S10OD018522. We are grateful to the eMERGE network for making their data available through dbGaP phs000888.v1.p1. Specifically, we acknowledge a consortium of ten participating sites (Cincinnati Children’s Hospital Medical Center/Boston Children’s Hospital, Children’s Hospital of Philadelphia, Essentia Institute of Rural Health, Marshfield Clinic Research Foundation and Pennsylvania State University, Geisinger Clinic, Group Health Cooperative/University of Washington, Mayo Clinic, Icahn School of Medicine at Mount Sinai, Northwestern University, Vanderbilt University Medical Center) funded by the NHGRI. Assistance with phenotype harmonization and genotype data cleaning was provided by the eMERGE Administrative Coordinating Center (U01HG004603) and the National Center for Biotechnology Information (NCBI). We are also grateful to Ben Neale and the Neale Lab for making their analyses of the UK Biobank data freely available prior to publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, W., Klein, R.J. Genome-wide association study identifies a role for the progesterone receptor in benign prostatic hyperplasia risk. Prostate Cancer Prostatic Dis 24, 492–498 (2021). https://doi.org/10.1038/s41391-020-00303-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-020-00303-2
This article is cited by
-
Genetic risk assessment of lethal prostate cancer using polygenic risk score and hereditary cancer susceptibility genes
Journal of Translational Medicine (2023)
-
Genetic, Genomic, and Heritable Components of Benign Prostatic Hyperplasia
Current Bladder Dysfunction Reports (2023)