Abstract
Background
Understanding competing risks for mortality is critical in determining prognosis among men with non-metastatic castration-resistant prostate cancer (nmCRPC), a disease state that often affects older men and has substantial heterogeneity in risk of cancer mortality. We sought to determine the impact of age, comorbidity, and PSA doubling time (PSADT) on competing risks for mortality in men with nmCRPC.
Methods
We conducted a retrospective analysis of 1238 patients diagnosed with nmCRPC in 2000–2015 in the SEARCH database. Multivariable Cox proportional hazards and competing risks regression were used to determine the hazards of overall, prostate cancer-specific (PCSM), and other-cause mortality (OCM) across age, Charlson comorbidity index (CCI), and PSADT subgroups.
Results
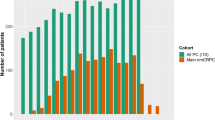
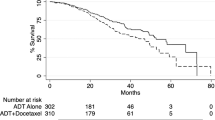
Men with nmCRPC were elderly (median age 77) and had substantial comorbidity burdens (CCI > 1 n = 701, 57%). Multivariable Cox analysis showed higher CCI was associated with higher hazard of OCM, while slower PSADT was associated with lower hazard of PCSM across all age subgroups. Among those with CCI ≥ 3 (vs. CCI0), the hazard ratio of OCM was 2.7 (95% CI 1.1–6.3), 2.0 (95% CI 1.1–3.6), and 2.5 (95% CI 1.5–4.0) for those aged <70, 70–79, and ≥80, respectively. Among those with PSADT ≥ 9 months (vs. < 9 months), the hazard ratios for PCSM were 0.5 (95% CI 0.3–0.9), 0.6 (95% CI 0.4–0.9), and 0.6 (95% CI 0.4–0.9) for those aged <70, 70–79, and ≥80. Competing risks curves revealed PCSM was the predominant cause of death for those with PSADT < 9 months across all age and comorbidity groups. PCSM and OCM were relatively equal competitors for mortality among those with PSADT≥9 months except those aged > 80 with CCI ≥ 3, in whom OCM was the predominant cause of death.
Conclusions
Among men with nmCRPC, age, comorbidity, and PSADT are associated with risk and cause of death and may assist clinicians in counseling patients regarding cancer prognosis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Kirby M, Hirst C, Crawford ED. Characterising the castration-resistant prostate cancer population: a systematic review. Int J Clin Pract. 2011;65:1180–92.
Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368:138–48.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424–33.
D’Amico AV, Schultz D, Schneider L, Hurwitz M, Kantoff PW, Richie JP. Comparing prostate specific antigen outcomes after different types of radiotherapy management of clinically localized prostate cancer highlights the importance of controlling for established prognostic factors. J Urol. 2000;163:1797–801.
Howard LE, Moreira D, De Hoedt A, Aronson WJ, Kane CJ, Amling CL, et al. Thresholds for PSA doubling time in men with non-metastatic castration-resistant prostate cancer. BJU Int. 2017;120(5B):E80–E86.
Read WL, Tierney RM, Page NC, Costas I, Govindan R, Spitznagel EL, et al. Differential prognostic impact of comorbidity. J Clin Oncol. 2004;22:3099–103.
Daskivich TJ, Fan KH, Koyama T, Albertsen PC, Goodman M, Hamilton AS, et al. Effect of age, tumor risk, and comorbidity on competing risks for survival in a U.S. population-based cohort of men with prostate cancer. Ann Intern Med. 2013;158:709–17.
Daskivich TJ, Chamie K, Kwan L, Labo J, Dash A, Greenfield S, et al. Comorbidity and competing risks for mortality in men with prostate cancer. Cancer. 2011;117:4642–50.
Albertsen PC, Moore DF, Shih W, Lin Y, Li H, Lu-Yao GL. Impact of comorbidity on survival among men with localized prostate cancer. J Clin Oncol. 2011;29:1335–41.
Uchio EM, Aslan M, Wells CK, Calderone J, Concato J. Impact of biochemical recurrence in prostate cancer among US veterans. Arch Intern Med. 2010;170:1390–5.
Small EJ, Saad F, Chowdhury S, Hadaschik BA, Graff JN, Olmos D, et al. SPARTAN, a phase 3 double-blind, randomized study of apalutamide (APA) versus placebo (PBO) in patients (pts) with nonmetastatic castration-resistant prostate cancer (nmCRPC). J Clin Oncol. 2018;36:161.
Hussain M, Fizazi K, Saad F, Rathenborg P, Shore ND, Demirhan E, et al. PROSPER: a phase 3, randomized, double-blind, placebo (PBO)-controlled study of enzalutamide (ENZA) in men with nonmetastatic castration-resistant prostate cancer (M0 CRPC). J Clin Oncol. 2018;36.
Moreira DM, Howard LE, Sourbeer KN, Amarasekara HS, Chow LC, Cockrell DC, et al. Predicting bone scan positivity in non-metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis. 2015;18:333–7.
Scher HI, Morris MJ, Basch E, Heller G. End points and outcomes in castration-resistant prostate cancer: from clinical trials to clinical practice. J Clin Oncol. 2011;29:3695–704.
Howard LE, Moreira DM, De Hoedt A, Aronson WJ, Kane CJ, Amling CL, et al. Thresholds for PSA doubling time in men with non-metastatic castration-resistant prostate cancer. BJU Int. 2017;120(5b):E80–e6.
Hanyok BT, Howard LE, Amling CL, Aronson WJ, Cooperberg MR, Kane CJ, et al. Is computed tomography a necessary part of a metastatic evaluation for castration-resistant prostate cancer? Results from the Shared Equal Access Regional Cancer Hospital Database. Cancer. 2016;122:222–9.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Rozet F, Roumeguere T, Spahn M, Beyersdorff D, Hammerer P. Non-metastatic castrate-resistant prostate cancer: a call for improved guidance on clinical management. World J Urol. 2016;34:1505–13.
Tombal B. Non-metastatic CRPC and asymptomatic metastatic CRPC: which treatment for which patient? Ann Oncol. 2012;23(Suppl 10):x251–8.
Gillessen S, Omlin A, Attard G, de Bono JS, Efstathiou E, Fizazi K, et al. Management of patients with advanced prostate cancer: recommendations of the St Gallen Advanced Prostate Cancer Consensus Conference (APCCC) 2015. Ann Oncol. 2016.
Pfizer and Astellas announce positive top-line results from phase 3 PROSPER Trial of XTANDI (enzalutamide) in patients with non-metastatic castration-resistant prostate cancer 2017. Available from: http://press.pfizer.com/press-release/pfizer-and-astellas-announce-positive-top-line-results-phase-3-prosper-trial-xtandi-en.
Saigal CS, Gore JL, Krupski TL, Hanley J, Schonlau M, Litwin MS, et al. Androgen deprivation therapy increases cardiovascular morbidity in men with prostate cancer. Cancer. 2007;110:1493–500.
Keating NL, O’Malley AJ, Smith MR. Diabetes and cardiovascular disease during androgen deprivation therapy for prostate cancer. J Clin Oncol. 2006;24:4448–56.
Keating NL, O’Malley AJ, Freedland SJ, Smith MR. Diabetes and cardiovascular disease during androgen deprivation therapy: observational study of veterans with prostate cancer. J Natl Cancer Inst. 2010;102:39–46.
Daskivich TJ, Litwin MS, Penson DF. Effect of age, tumor risk, and comorbidity in a U.S. population-based cohort of men with prostate cancer. Ann Intern Med. 2013;159:370.
Acknowledgements
Dr. Daskivich would like to acknowledge funding from K08 CA230155. Dr. Aronson would like to acknowledge funding from RO1 CA231219.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Daskivich is a consultant for Janssen Research and Development, LLC. Dr. Freedland is a consultant for Astellas Pharmceuticals and Janssen Research and Development. Other authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Whitney, C.A., Howard, L.E., Freedland, S.J. et al. Impact of age, comorbidity, and PSA doubling time on long-term competing risks for mortality among men with non-metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis 22, 252–260 (2019). https://doi.org/10.1038/s41391-018-0095-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-018-0095-0
This article is cited by
-
Is time to castration resistant prostate cancer a potential intermediate end-point for time to metastasis among men initiating androgen deprivation therapy for non-metastatic prostate cancer with rapid PSA doubling time (<9 months)?
Prostate Cancer and Prostatic Diseases (2023)
-
Competing risk nomogram for predicting cancer-specific mortality in patients with non-melanoma skin cancer
Journal of Cancer Research and Clinical Oncology (2023)
-
Time to castration resistance is a novel prognostic factor of cancer-specific survival in patients with nonmetastatic castration-resistant prostate cancer
Scientific Reports (2022)
-
A competing risk nomogram predicting cause-specific mortality in patients with lung adenosquamous carcinoma
BMC Cancer (2020)
-
Spanish validation of Charlson index applied to prostate cancer
Clinical and Translational Oncology (2020)