Abstract
Importance
Fluoroquinolone (FQ)-resistant rectal vault flora is associated with infectious complications in men undergoing transrectal ultrasound-guided prostate needle biopsy (TRUS-PNB).
Objective
To determine the patient factors that predict FQ-resistant rectal cultures in men who are undergoing transrectal ultrasound-guided prostate needle biopsy.
Methods
An IRB approved retrospective review of 6183 consecutive men who had undergone a rectal swab culture in preparation for TRUS-PNB between January 2013 and December 2014 was performed. Multivariable logistic regression was used to determine the clinical and demographic factors associated with FQ-resistant Enterobacteriaceae in the rectal vault.
Results
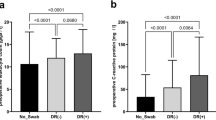
Of the 6179 rectal swabs analyzed, 4842 (78%) were FQ-sensitive, and 1337 (22%) were FQ-resistant. On univariable analysis, increasing age, prior TRUS-PNB, higher number of biopsy cores obtained, diabetes mellitus, antimicrobial use within the past 6 months and non-Caucasian race were predictors of FQ-resistance (all p < 0.05). Men with FQ-resistant cultures were more likely to have benign pathology on TRUS-PNB (p = 0.004). On multivariable analysis, increasing patient age (OR = 1.01/year [1.00–1.02]), use of antimicrobials in the last 6 months (OR = 2.85[2.18–3.72]), African American (OR = 1.99 [1.66–2.37]), Asian (OR = 3.39 [2.63–4.37]), and Hispanic (OR = 2.10 [1.72–2.55]) races were independently associated with FQ-resistant rectal cultures. The overall infectious rate was 1.1% (56/5214) and the sepsis rate was 0.46% (24/5214). The infection rate in the FQ-resistant group was 3.9% (43/1107) compared to FQ-sensitive group 0.3% (13/4107), p < 0.001.
Conclusion
In this cohort, increasing age, recent antimicrobial-use, and non-Caucasian race were independent predictors of FQ-resistance in the rectal vault. As FQ-resistance is associated with infectious complications from transrectal ultrasound-guided prostate needle biopsy, understanding risk factors may assist infection control efforts.
Key points
-
Question: What are the factors that predict fluoroquinolone (FQ)-resistant rectal cultures in men undergoing transrectal ultrasound-guided prostate needle biopsy?
-
Findings: Increasing age, recent antimicrobial-use, African American, Asian, and Hispanic race were independent predictors of FQ resistance in the rectal vault.
-
Meaning: Older man, antimicrobial usage within 6 months, African American, Asian and Hispanic race were associated with men with FQ-resistance rectal flora and may benefit from alternative prophylaxis and monitoring strategies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Change history
31 January 2019
The original version of this article contained an error in the name of author Alfredo Mena Lora. This has now been corrected.
References
Nam RK, Saskin R, Lee Y, Liu Y, Law C, Klotz LH, et al. Increasing hospital admission rates for urological complications after transrectal ultrasound guided prostate biopsy. J Urol. 2013;189(1 Suppl):S12–17. discussionS17-18
Bearden DT, Danziger LH. Mechanism of action of and resistance to quinolones. Pharmacotherapy. 2001;21(10 Pt 2):224s–232s.
Warren JW, Abrutyn E, Hebel JR, Johnson JR, Schaeffer AJ, Stamm WE. Guidelines for antimicrobial treatment of uncomplicated acute bacterial cystitis and acute pyelonephritis in women. Infectious Diseases Society of America (IDSA). Clin Infect Dis. 1999;29:745–58.
Johnson L, Sabel A, Burman WJ, Everhart RM, Rome M, MacKenzie TD, et al. Emergence of fluoroquinolone resistance in outpatient urinary Escherichia coli isolates. Am J Med. 2008;121:876–84.
Peirano G, Pitout JD. Fluoroquinolone-resistant Escherichia coli sequence type 131 isolates causing bloodstream infections in a canadian region with a centralized laboratory system: rapid emergence of the H30-Rx sublineage. Antimicrob Agents Chemother. 2014;58:2699–703.
Banerjee R, Johnston B, Lohse C, Porter SB, Clabots C, Johnson JR. Escherichia coli sequence type 131 is a dominant, antimicrobial-resistant clonal group associated with healthcare and elderly hosts. Infect Control Hosp Epidemiol. 2013;34:361–9.
Brigmon MM, Bookstaver PB, Kohn J, Albrecht H, Al-Hasan MN. Impact of fluoroquinolone resistance in Gram-negative bloodstream infections on healthcare utilization. Clin Microbiol Infect. 2015;21:843–9.
Ebbing L, Metlay JP, Bilker WB, Edelstein PH, Fishman NO. Association between fluoroquinolone resistance and mortality in Escherichia coli and Klebsiella pneumoniae infections: the role of inadequate empirical antimicrobial therapy. Clin Infect Dis. 2005;41:923–9.
Loeb S, Carter HB, Berndt SI, Ricker W, Schaeffer EM. Complications after prostate biopsy: data from SEER-Medicare. J Urol. 2011;186:1830–4.
Liss MA, Ehdaie B, Loeb S, Meng MV, Raman JD, Spears V, et al. An update of the American Urological Association white paper on the prevention and treatment of the more common complications related to prostate biopsy. J Urol. 2017;198:329–34.
Papagiannopoulos D, Abern M, Wilson N, O’Block N, Raff L, Coogan C, et al. Predictors of infectious complications after targeted prophylaxis for prostate needle biopsy. J Urol. 2017;199:155–160.
Ng CF, Chan SY. Re: The incidence of fluoroquinolone resistant infections after prostate biopsy--are fluoroquinolones still effective prophylaxis? Feliciano J, Teper E, Ferrandino M, Macchia RJ, Blank W, Grunberger I, et al. J Urol. 2008;179:952–955. J Urol.2008;180:1570–1.author reply 1571.
Roberts MJ, Williamson DA, Hadway P, Doi SA, Gardiner RA, Paterson DL. Baseline prevalence of antimicrobial resistance and subsequent infection following prostate biopsy using empirical or altered prophylaxis: a bias-adjusted meta-analysis. Int J Antimicrob Agents. 2014;43:301–9.
Papagiannopoulos D, Abern M, Wilson N, O’Block N, Raff L, Coogan C, et al. Predictors of infectious complications after targeted prophylaxis for prostate needle biopsy. J Urol. 2018;199:155–60.
Morgan-Linnell SK, Becnel Boyd L, Steffen D, Zechiedrich L. Mechanisms accounting for fluoroquinolone resistance in Escherichia coli clinical isolates. Antimicrob Agents Chemother. 2009;53:235–41.
Karlowsky JA, Hoban DJ, Decorby MR, Laing NM, Zhanel GG. Fluoroquinolone-resistant urinary isolates of Escherichia coli from outpatients are frequently multidrug resistant: results from the North American Urinary Tract Infection Collaborative Alliance-Quinolone Resistance study. Antimicrob Agents Chemother. 2006;50:2251–4.
Redgrave LS, Sutton SB, Webber MA, Piddock LJV. Fluoroquinolone resistance: mechanisms, impact on bacteria, and role in evolutionary success. Trends Microbiol. 2014;22:438–45.
van der Starre WE, van Nieuwkoop C, Paltansing S, van’t Wout JW, Groeneveld GH, Becker MJ, et al. Risk factors for fluoroquinolone-resistant Escherichia coli in adults with community-onset febrile urinary tract infection. J Antimicrob Chemother. 2011;66:650–6.
Rattanaumpawan P, Tolomeo P, Bilker WB, Fishman NO, Lautenbach E. Risk factors for fluoroquinolone resistance in Enterococcus urinary tract infections in hospitalized patients. Epidemiol Infect. 2011;139:955–61.
Rehman MS, Rashid N, Ashfaq M, Saif A, Ahmad N, Han JI. Global risk of pharmaceutical contamination from highly populated developing countries. Chemosphere. 2015;138:1045–55.
Kookana RS, Williams M, Boxall AB, Larsson DG, Gaw S, Choi K, et al. Potential ecological footprints of active pharmaceutical ingredients: an examination of risk factors in low-, middle- and high-income countries. Philos Trans R Soc Lond B Biol Sci. 2014;369 pii: 20130586. https://doi.org/10.1098/rstb.2013.0586.
Van Boeckel TP, Gandra S, Ashok A, Caudron Q, Grenfell BT, Levin SA. et al. Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data. Lancet Infect Dis.2014;14:742–50.
Hoeffel EM, Rastogi S, Kim MO, Hasan S, Economics US, Administration et al. The Asian Population: 2010. U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau, 2012.
Rohren EM, Etchebehere EC, Araujo JC, Hobbs BP, Swanston NM, Everding M, et al. Determination of skeletal tumor burden on 18F-fluoride PET/CT. J Nucl Med. 2015;56:1507–12.
Patel U, Dasgupta P, Amoroso P, Challacombe B, Pilcher J, Kirby R. Infection after transrectal ultrasonography-guided prostate biopsy: increased relative risks after recent international travel or antibiotic use. BJU Int. 2012;109:1781–5.
Rattanaumpawan P, Tolomeo P, Bilker WB, Fishman NO, Lautenbach E. Risk factors for fluoroquinolone resistance in Gram-negative bacilli causing healthcare-acquired urinary tract infections. J Hosp Infect. 2010;76:324–7.
Lautenbach E, Fishman NO, Bilker WB, et al. Risk factors for fluoroquinolone resistance in nosocomial escherichia coli and klebsiella pneumoniae infections. Arch Intern Med. 2002;162:2469–77.
Bozeman CB, Carver BS, Eastham JA, Venable DD. Treatment of chronic prostatitis lowers serum prostate specific antigen. J Urol. 2002;167:1723–6.
Speakman MJ, Cheng X. Management of the complications of BPH/BOO. Indian J Urol. 2014;30:208–13.
Saraswati S, Sitaraman R. Aging and the human gut microbiota—from correlation to causality. Front. Microbiol. 2015;5.
Magrone T, Jirillo E. The interaction between gut microbiota and age-related changes in immune function and inflammation. Immun Ageing. 2013;10:31.
Vyas L, Acher P, Kinsella J, Challacombe B, Chang RT, Sturch P, et al. Indications, results and safety profile of transperineal sector biopsies (TPSB) of the prostate: a single centre experience of 634 cases. BJU Int. 2014;114:32–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Tan, W., Papagiannopoulos, D., Latchamsetty, K.C. et al. Predictors of fluoroquinolone-resistant bacteria in the rectal vault of men undergoing prostate biopsy. Prostate Cancer Prostatic Dis 22, 268–275 (2019). https://doi.org/10.1038/s41391-018-0092-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-018-0092-3
This article is cited by
-
Risk assessment of multi-factorial complications after transrectal ultrasound-guided prostate biopsy: a single institutional retrospective cohort study
International Journal of Clinical Oncology (2021)
-
Infectious complications of prostate biopsy: winning battles but not war
World Journal of Urology (2020)
-
A novel method for pain control: infiltration free local anesthesia technique (INFLATE) for transrectal prostatic biopsy using transcutaneous electrical nerve stimulation (TENS)
International Urology and Nephrology (2019)