Abstract
Background
We performed a systematic review and meta-analysis to determine the prevalence and predictors of urethral stricture development post radiation therapy (RT) for prostate cancer (PCa).
Methods
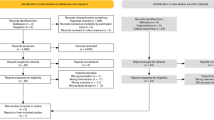
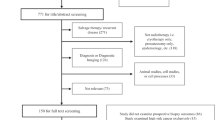
Published articles in PubMed/Medline, Cochrane, and Embase databases from January 2000 to April 2016 were queried. Inclusion criteria were any study that reported the prevalence of urethral strictures following external beam radiation therapy (EBRT), brachytherapy (BT), or both as a primary treatment for PCa. Forty-six articles met our inclusion criteria. A summary estimate of the proportion of patients who developed a urethral stricture was derived via a random effects meta-analysis.
Results
In total, 16,129 PCa patients underwent either EBRT (5681, 35.2%), BT (5849, 36.3%), or both (4599, 28.5%). Overall, 630 strictures were diagnosed at follow-up with a pooled estimate period prevalence of 2.2% (95% confidence interval, CI 1.9–2.6%) in a median follow-up time of 4 years (interquartile range, IQR 2.7–5). Of which, the pooled estimate prevalence was 1.5% (95% CI 0.9–2%) post EBRT, 1.9% (95% CI 1.3–2.4%) post BT, and 4.9% (95% CI 3.8–6%) post both EBRT and BT. Of 20 studies reporting a median time to stricture formation, the overall median time was 2.2 years (IQR 1.8–2.5, range 1.4–9). In a meta-regression analysis, receiving both EBRT and BT increased the estimated difference in proportion of stricture diagnoses by 3% (95% CI 1–6%), p = 0.018 compared to EBRT alone. An increase in median follow-up time was found to significantly increase the risk of developing urethral strictures (p = 0.04).
Conclusions
With a short-term follow-up, urethral strictures occur in 2.2% of men with PCa receiving radiotherapy. Receiving both EBRT and BT increased the risk of stricture formation. Longer follow-up is needed to determine the long-term natural history of stricture formation after RT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E86.
Cooperberg MR, Broering JM, Carroll PR. Time trends and local variation in primary treatment of localized prostate cancer. J Clin Oncol. 2010;28:1117–23.
Blackwell RH, Kandabarow AM, Gupta GN, Harkenrider MM, Quek ML, Flanigan RC. Long-term incidence of hematuria, urethral stricture and bladder cancer after radiation therapy for prostate cancer. Urol Pract. 2015;2:349–58.
Tibbs MK. Wound healing following radiation therapy: a review. Radiother Oncol. 1997;42:99–106.
Hofer MD, Zhao LC, Morey AF, Scott JF, Chang AJ, Brandes SB, et al. Outcomes after urethroplasty for radiotherapy induced bulbomembranous urethral stricture disease. J Urol. 2014;191:1307–12.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Stock RG, Stone NN, Cesaretti JA, Rosenstein BS. Biologically effective dose values for prostate brachytherapy: effects on PSA failure and posttreatment biopsy results. Int J Radiat Oncol Biol Phys. 2006;64:527–33.
Wells G, Shea B, O’connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2011.
Hunter JP, Saratzis A, Sutton AJ, Boucher RH, Sayers RD, Bown MJ. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J Clin Epidemiol. 2014;67:897–903.
Elliott SP, Meng MV, Elkin EP, McAninch JW, Duchane J, Carroll PR, et al. Incidence of urethral stricture after primary treatment for prostate cancer: data from CaPSURE. J Urol. 2007;178:529–34.
Jarosek SL, Virnig BA, Chu H, Elliott SP. Propensity-weighted long-term risk of urinary adverse events after prostate cancer surgery, radiation, or both. Eur Urol. 2015;67:273–80.
Rodda S, Tyldesley S, Morris WJ, Keyes M, Halperin R, Pai H, et al. ASCENDE-RT: an analysis of treatment-related morbidity for a randomized trial comparing a low-dose-rate brachytherapy boost with a dose-escalated external beam boost for high-and intermediate-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2017;98:286–95.
Mohammed N, Kestin L, Ghilezan M, Krauss D, Vicini F, Brabbins D, et al. Comparison of acute and late toxicities for three modern high-dose radiation treatment techniques for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2012;82:204–12.
Earley JJ, Abdelbaky AM, Cunningham MJ, Chadwick E, Langley SE, Laing RW. Correlation between prostate brachytherapy-related urethral stricture and peri-apical urethral dosimetry: A matched case–control study. Radiother Oncol. 2012;104:187–91.
Seppenwoolde Y, Kolkman-Deurloo I-K, Sipkema D, de Langen M, Praag J, Jansen P, et al. HDR prostate monotherapy–dosimetric effects of implant deformation due to posture change between TRUS-and CT-imaging. Radiother Oncol. 2008;86:114–9.
Morton G. The emerging role of high-dose-rate brachytherapy for prostate cancer. Clin Oncol. 2005;17:219–27.
Myers MA, Hagan MP, Todor D, Gilbert L, Mukhopadhyay N, Randolf J, et al. Phase I/II trial of single-fraction high-dose-rate brachytherapy–boosted hypofractionated intensity-modulated radiation therapy for localized adenocarcinoma of the prostate. Brachytherapy. 2012;11:292–8.
Spratt DE, Soni PD, McLaughlin PW, Merrick GS, Stock RG, Blasko JC, et al. American Brachytherapy Society Task Group Report: combination of brachytherapy and external beam radiation for high-risk prostate cancer. Brachytherapy. 2017;16:1–12.
Sweeney C, Xie W, Regan MM, Nakabayashi M, Buyse ME, Clarke NW, et al. Disease-free survival (DFS) as a surrogate for overall survival (OS) in localized prostate cancer (CaP). American Society of Clinical Oncology; 2016;5023.
Allen ZA, Merrick GS, Butler WM, Wallner KE, Kurko B, Anderson RL, et al. Detailed urethral dosimetry in the evaluation of prostate brachytherapy-related urinary morbidity. Int J Radiat Oncol Biol Phys. 2005;62:981–7.
Merrick GS, Butler WM, Wallner KE, Galbreath RW, Lief JH. Long-term urinary quality of life after permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2003;56:454–61.
Butler WM, Merrick GS, Dorsey AT, Hagedorn BM. Comparison of dose length, area, and volume histograms as quantifiers of urethral dose in prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2000;48:1575–82.
Sullivan L, Williams SG, Tai KH, Foroudi F, Cleeve L, Duchesne GM. Urethral stricture following high dose rate brachytherapy for prostate cancer. Radiother Oncol. 2009;91:232–6.
Bece A, Patanjali N, Jackson M, Whitaker M, Hruby G. High-dose-rate brachytherapy boost for prostate cancer: outcomes and genitourinary toxicity. Brachytherapy. 2015;14:670–6.
Kaprealian T, Weinberg V, Speight JL, Gottschalk AR, Roach M, Shinohara K, et al. High-dose-rate brachytherapy boost for prostate cancer: comparison of two different fractionation schemes. Int J Radiat Oncol Biol Phys. 2012;82:222–7.
Walsh PC, RA, Vaughan ED, Wein AJ, eds.. Campbell’s urology. 7th ed. Philadelphia: WB Saunders; 1998.
Madersbacher S, Marberger M. Is transurethral resection of the prostate still justified. BJU Int. 1999;83:227–37.
Seymore CH, El-Mahdi AM, Schellhammer PF. The effect of prior transurethral resection of the prostate on post radiation urethral strictures and bladder neck contractures. Int J Radiat Oncol Biol Phys. 1986;12:1597–600.
Ishiyama H, Satoh T, Kitano M, Tabata K-I, Komori S, Ikeda M, et al. High-dose-rate brachytherapy and hypofractionated external beam radiotherapy combined with long-term hormonal therapy for high-risk and very high-risk prostate cancer: outcomes after 5-year follow-up. J Radiat Res. 2013;55:509–17.
Merrick GS, Butler WM, Tollenaar BG, Galbreath RW, Lief JH. The dosimetry of prostate brachytherapy-induced urethral strictures. Int J Radiat Oncol Biol Phys. 2002;52:461–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Awad, M.A., Gaither, T.W., Osterberg, E.C. et al. Prostate cancer radiation and urethral strictures: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis 21, 168–174 (2018). https://doi.org/10.1038/s41391-017-0028-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-017-0028-3
This article is cited by
-
Prostate cancer risk, screening and management in patients with germline BRCA1/2 mutations
Nature Reviews Urology (2023)
-
Long term genitourinary toxicity following curative intent intensity-modulated radiotherapy for prostate cancer: a systematic review and meta-analysis
Prostate Cancer and Prostatic Diseases (2023)
-
Long-term follow-up suggests high satisfaction rates for bulbomembranous radiation-induced urethral stenoses treated with anastomotic urethroplasty
World Journal of Urology (2023)
-
Randomised controlled trial to investigate the effectiveness of the symptom management after radiotherapy (SMaRT) group intervention to ameliorate lower urinary tract symptoms in men treated for prostate cancer
Supportive Care in Cancer (2022)
-
Management of Lower Urinary Tract Symptoms after Prostate Radiation
Current Urology Reports (2021)