Abstract
Background
Neutrophil–lymphocyte ratio (NLR) is a widely used, representative marker of systemic inflammatory response within the body. NLR can be calculated from simple, inexpensive peripheral blood samples. High NLR is a negative prognostic factor in a variety of malignancies including urological tumors. In this study, we aim to assess the prognostic value of preoperative neutrophil- lymphocyte ratio (NLR) in patients treated with radical prostatectomy (RP) for localized prostate cancer (PCa).
Materials and methods
Records of 7426 patients were retrospectively analyzed from prospectively collected datasets. A cut-off point of 3 was taken for NLR based on ROC analyses and previous literature.
Results
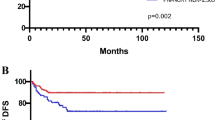
23% (n = 1707) of patients had an NLR of ≥3. Patients with NLR ≥3 were more likely to harbor unfavorable pathological features such as higher biopsy Gleason score (GS), higher RP GS, higher rates of extra capsular extension, nodal involvement (all p < 0.001) and positive surgical margins (p = 0.002). On multivariable analyses, NLR ≥ 3 was associated with higher RP GS (OR 2.32; p < 0.001), seminal vesicle invasion (OR 1.60; p < 0.001) and nodal involvement (OR 1.43; p < 0.001). On multivariable analyses, NLR ≥ 3 was significantly associated with GS upgrading at RP (OR 1.39 p < 0.001). During a median follow up of 45 months, NLR ≥ 3 was associated with higher risk of BCR (p = 0.001). However, on multivariable Cox regression analysis such association was not shown (HR 0.86; p = 0.4).
Conclusion
Preoperative NLR ≥ 3 was associated with aggressive PCa, such as upgrading at RP. Even though its effect on clinical-decision making seems to be limited when all clinical and pathological confounders are taken into account, preoperative NLR may still be useful in selected patients to identify aggressive PCa helping patient selection for active surveillance protocols. Conversely, it does not predict BCR when adjusted for the effect of pathological features.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Siegel, RL, Miller, KD, Jemal, A Cancer statistics, 2016. CA Cancer J Clin. 2016 Jan [cited 2017 Jul 4];66:7–30. http://www.ncbi.nlm.nih.gov/pubmed/26742998.
Mantovani A, Allavena P, Sica A, Balkwill F, Cancer-related inflammation. Nature. 2008;454:436–44. http://www.nature.com/doifinder/10.1038/nature07205.
De Martino, M et al. Validation of serum C-reactive protein (CRP) as an independent prognostic factor for disease-free survival in patients with localised renal cell carcinoma (RCC). BJU Int. 2013;111:E348–53.
Zhou L, Cai X, Liu Q, Jian Z-Y, Li H, Wang K-J. Prognostic role of C-reactive protein in urological cancers: a meta-analysis. Sci Rep. 2015;5:12733 https://doi.org/10.1038/srep12733.
Macciò A, Madeddu C. Inflammation and ovarian cancer. Cytokine. 2012;58:133–47.
Lu H, Ouyang W, Huang C. Inflammation, a key event in cancer development. Mol Cancer Res. 2006;4:221–33. http://mcr.aacrjournals.org/content/4/4/221.full.html%5Cnhttp://mcr.aacrjournals.org/content/4/4/221.full
Kusumanto YH, Dam WA, Hospers GAP, Meijer C, Mulder NH. Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis. 2003;6:283–7.
Sevcenco S, Mathieu R, Baltzer P, Klatte T, Fajkovic H, Seitz C, et al. The prognostic role of preoperative serum C-reactive protein in predicting the biochemical recurrence in patients treated with radical prostatectomy. Prostate Cancer Prostatic Dis. 2016;19:163–7.
Koike Y, Miki C, Okugawa Y, Yokoe T, Toiyama Y, Tanaka K, et al. Preoperative C-reactive protein as a prognostic and therapeutic marker for colorectal cancer. J Surg Oncol. 2008;98:540–4.
Lee H, Jeong SJ, Hong SK, Byun S-S, Lee SE, Oh JJ. High preoperative neutrophil-lymphocyte ratio predicts biochemical recurrence in patients with localized prostate cancer after radical prostatectomy. World J Urol. 2016;34:821–7. http://www.ncbi.nlm.nih.gov/pubmed/26449784.
De Martino M, Pantuck AJ, Hofbauer S, Waldert M, Shariat SF, Belldegrun AS, et al. Prognostic impact of preoperative neutrophil-to-lymphocyte ratio in localized nonclear cell renal cell carcinoma. J Urol. 2013;190:1999–2004.
Tang L, Li X, Wang B, Luo G, Gu L, Chen L, et al. Prognostic value of neutrophil-to-lymphocyte ratio in localized and advanced prostate cancer: a systematic review and meta-analysis. PLoS One. 2016;11:e0153981. http://dx.plos.org/10.1371/journal.pone.0153981
Templeton, AJ et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106:dju124.
Kawahara T, Fukui S, Sakamaki K, Ito Y, Ito H, Kobayashi N, et al. Neutrophil-to-lymphocyte ratio predicts prostatic carcinoma in men undergoing needle biopsy. Oncotarget. 2015;6:32169–76.
Nuhn P, Vaghasia AM, Goyal J, Zhou XC, Carducci MA, Eisenberger MA, et al. Association of pretreatment neutrophil-to-lymphocyte ratio (NLR) and overall survival (OS) in patients with metastatic castration-resistant prostate cancer (mCRPC) treated with first-line docetaxel. BJU Int. 2014;114:E11–7.
Leibowitz-Amit R, Templeton AJ, Omlin A, Pezaro C, Atenafu EG, Keizman D, et al. Clinical variables associated with PSA response to abiraterone acetate in patients with metastatic castration-resistant prostate cancer. Ann Oncol. 2014;25:657–62. http://annonc.oxfordjournals.org/content/25/3/657.short
Gazel E, Tastemur S, Acikgoz O, Yigman M, Olcucuoglu E, Camtosun A, et al. Importance of neutrophil/lymphocyte ratio in prediction of PSA recurrence after radical prostatectomy. Asian Pacific J Cancer Prev. 2015;16:1813–6.
Cookson MS, et al. Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American Urological Association Prostate Guidelines for Localized Prostate CancerUpdate Panel report and recommendations for a standard in the reporting of surgical outcomes. Urol. 2007;177:540–5.
Wheeler TM, Lebovitz RM. Fresh tissue harvest for research from prostatectomy specimens. Prostate. 1994;25:274–9. [cited 2016 Nov 27]. http://doi.wiley.com/10.1002/pros.2990250507.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988 [cited 2017 Jul 12];44:837–45. http://www.ncbi.nlm.nih.gov/pubmed/3203132.
D’Amico AV, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. J Am Med Assoc 1998;280:969–74.
Partin AW, Mangold LA, Lamm DM, Walsh PC, Epstein JI, Pearson JD. Contemporary update of prostate cancer staging nomograms (Partin Tables) for the new millennium. Urology. 2001;58:843–8.
Maeda Y, Kawahara T, Koizumi M, Ito H, Kumano Y, Ohtaka M, et al. Lack of an association between neutrophil-to-lymphocyte ratio and PSA failure of prostate cancer patients who underwent radical prostatectomy. Biomed Res Int. 2016;2016:6197353.
Minardi D, Scartozzi M, Montesi L, Santoni M, Burattini L, Bianconi M, et al. Neutrophil-to-lymphocyte ratio may be associated with the outcome in patients with prostate cancer. Springerplus. 2015;4:255. http://www.springerplus.com/content/4/1/255.
Kwon YS, Han CS, Yu JW, Kim S, Modi P, Davis R, et al. Neutrophil and lymphocyte counts as clinical markers for stratifying low-risk prostate cancer. Clin Genitourin Cancer. 2016;14:e1–8. http://linkinghub.elsevier.com/retrieve/pii/S1558767315001913.
Montironi R, Hammond EH, Lin DW, Gore JL, Srigley JR, Samaratunga H, et al. Consensus statement with recommendations on active surveillance inclusion criteria and definition of progression in men with localized prostate cancer: the critical role of the pathologist. Virchows Archiv. 2014;465:623–8.
Ploussard G, Isbarn H, Briganti A, Sooriakumaran P, Surcel CI, Salomon L, et al. Can we expand active surveillance criteria to include biopsy Gleason 3+4 prostate cancer? A multi-institutional study of 2,323 patients. Urol Oncol Semin Orig Investig. 2015;33:71e1–9.
Moschini M, Spahn M, Mattei A, Cheville J, Karnes RJ. Incorporation of tissue-based genomic biomarkers into localized prostate cancer clinics. BMC Med. 2016;14:67. http://www.ncbi.nlm.nih.gov/pubmed/27044421%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4820857.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with Ethical Standards
All data were collected after receiving approval from local ethical committee.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Özsoy, M., Moschini, M., Fajkovic, H. et al. Elevated preoperative neutrophil–lymphocyte ratio predicts upgrading at radical prostatectomy. Prostate Cancer Prostatic Dis 21, 100–105 (2018). https://doi.org/10.1038/s41391-017-0015-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-017-0015-8
This article is cited by
-
A high high-density lipoprotein level is associated with Gleason score upgrade in Chinese patients diagnosed with high-grade prostate carcinoma
BMC Urology (2023)
-
Neutrophil-to-lymphocyte ratio predicts nodal involvement in unfavourable, clinically nonmetastatic prostate cancer patients and overall survival in pN1 patients
Scientific Reports (2023)