Abstract
Background
Acquired neonatal intestinal diseases have an array of overlapping presentations and are often labeled under the dichotomous classification of necrotizing enterocolitis (which is poorly defined) or spontaneous intestinal perforation, hindering more precise diagnosis and research. The objective of this study was to take a fresh look at neonatal intestinal disease classification using unsupervised machine learning.
Methods
Patients admitted to the University of Florida Shands Neonatal Intensive Care Unit January 2013–September 2019 diagnosed with an intestinal injury, or had imaging findings of portal venous gas, pneumatosis, abdominal free air, or had an abdominal drain placed or exploratory laparotomy during admission were included. Congenital gastroschisis, omphalocele, intestinal atresia, malrotation were excluded. Data was collected via retrospective chart review with subsequent hierarchal, unsupervised clustering analysis.
Results
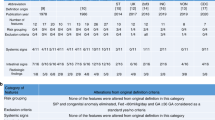
Five clusters of intestinal injury were identified: Cluster 1 deemed the “Low Mortality” cluster, Cluster 2 deemed the “Mature with Inflammation” cluster, Cluster 3 deemed the “Immature with High Mortality” cluster, Cluster 4 deemed the “Late Injury at Full Feeds” cluster, and Cluster 5 deemed the “Late Injury with High Rate of Intestinal Necrosis” cluster.
Conclusion
Unsupervised machine learning can be used to cluster acquired neonatal intestinal injuries. Future study with larger multicenter datasets is needed to further refine and classify types of intestinal diseases.
Impact
-
Unsupervised machine learning can be used to cluster types of acquired neonatal intestinal injury.
-
Five major clusters of acquired neonatal intestinal injury are described, each with unique features.
-
The clusters herein described deserve future, multicenter study to determine more specific early biomarkers and tailored therapeutic interventions to improve outcomes of often devastating neonatal acquired intestinal injuries.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The dataset generated and analyzed during this study is included as a supplement.
References
Mizrahi, A., Barlow, O., Berdon, W., Blanc, W. A. & Silverman, W. A. Necrotizing enterocolitis in premature infants. J. Pediatr. 66, 697–706 (1965).
Lueschow, S. R., Boly, T. J., Jasper, E., Patel, R. M. & McElroy, S. J. A critical evaluation of current definitions of necrotizing enterocolitis. Pediatr. Res. 91, 590–597 (2022).
Alda, E. Why so many published studies and so little progress in necrotizing enterocolitis? Arch. Argent. Pediatr. 118, 372–374 (2020).
Patel, R. M., Ferguson, J., McElroy, S. J., Khashu, M. & Caplan, M. S. Defining necrotizing enterocolitis: current difficulties and future opportunities. Pediatr. Res 88, 10–15 (2020).
Neu, J., Modi, N. & Caplan, M. Necrotizing enterocolitis comes in different forms: Historical perspectives and defining the disease. Semin. Fetal Neonatal Med. 23, 370–373 (2018).
Neu, J. Necrotizing Enterocolitis: The future. Neonatology 117, 240–244 (2020).
Neu, J. Prevention of necrotizing Enterocolitis. Clin. Perinatol. 49, 195–206 (2022).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 187, 1–7 (1978).
Walsh, M. C. & Kliegman, R. M. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr. Clin. North Am. 33, 179–201 (1986).
Nagaraj, H. S., Sandhu, A. S., Cook, L. N., Buchino, J. J. & Groff, D. B. Gastrointestinal perforation following indomethacin therapy in very low birth weight infants. J. Pediatr. Surg. 16, 1003–1007 (1981).
Aschner, J. L., Deluga, K. S., Metlay, L. A., Emmens, R. W. & Hendricks-Munoz, K. D. Spontaneous focal gastrointestinal perforation in very low birth weight infants. J. Pediatr. 113, 364–367 (1988).
De La Cruz, D., Lure, A. & Neu, J. Necrotizing Enterocolitis. World Rev. Nutr. Diet. 122, 367–378 (2021).
Moss, R. L. et al. Laparotomy versus peritoneal drainage for necrotizing enterocolitis and perforation. N. Engl. J. Med 354, 2225–2234 (2006).
Rees, C. M. et al. Peritoneal drainage or laparotomy for neonatal bowel perforation? A randomized controlled trial. Ann. Surg. 248, 44–51 (2008).
Blakely, M. L. et al. Initial laparotomy versus peritoneal drainage in extremely low birthweight infants with surgical necrotizing enterocolitis or isolated intestinal perforation: a multicenter randomized clinical trial. Ann. Surg. 274, e370–e380 (2021).
2022 Manual of Operations, Part 2, Release 26.1 (PDF) – Help Center. https://vtoxford.zendesk.com/hc/en-us/articles/4405064008467-2022-Manual-of-Operations-Part-2-Release-26-1-PDF -.
CDC, Ncezid & DHQP. CDC/NHSN Surveillance Definitions for Specific Types of Infections. (2022).
Ji, J. et al. A data-driven algorithm integrating clinical and laboratory features for the diagnosis and prognosis of necrotizing enterocolitis. PLoS One 9, e89860 (2014).
Battersby, C., Longford, N., Costeloe, K. & Modi, N. Development of a gestational age-specific case definition for neonatal necrotizing Enterocolitis. JAMA Pediatr. 171, 256–263 (2017).
Gephart, S. M. et al. Changing the paradigm of defining, detecting, and diagnosing NEC: Perspectives on Bell’s stages and biomarkers for NEC. Semin. Pediatr. Surg. 27, 3–10 (2018).
Caplan, M. S. et al. Necrotizing Enterocolitis: Using regulatory science and drug development to improve outcomes. J. Pediatr. 212, 208–215.e1 (2019).
Noorbakhsh-Sabet, N., Zand, R., Zhang, Y. & Abedi, V. Artificial intelligence transforms the future of health care. Am. J. Med 132, 795–801 (2019).
Hamamoto, R. Application of artificial intelligence for medical research. Biomolecules 11, 90 (2021).
De Francesco, D. et al. Data-driven longitudinal characterization of neonatal health and morbidity. Sci. Transl. Med. 15, eadc9854 (2023).
Campbell, J. P. et al. Applications of artificial intelligence for retinopathy of prematurity screening. Pediatrics 147, e2020016618 (2021).
Matsushita, F. Y., Krebs, V. L. J. & de Carvalho, W. B. Identifying clinical phenotypes in extremely low birth weight infants—an unsupervised machine learning approach. Eur. J. Pediatr. 181, 1085–1097 (2022).
Lure, A. C. et al. Using machine learning analysis to assist in differentiating between necrotizing enterocolitis and spontaneous intestinal perforation: A novel predictive analytic tool. J. Pediatr. Surg. 56, 1703–1710 (2021).
Pammi, M., Aghaeepour, N. & Neu, J. Multiomics, artificial intelligence, and precision medicine in perinatology. Pediatr. Res. 2022 1–8 (2022) https://doi.org/10.1038/s41390-022-02181-x.
Lin, Y. C., Salleb-Aouissi, A. & Hooven, T. A. Interpretable prediction of necrotizing enterocolitis from machine learning analysis of premature infant stool microbiota. BMC Bioinforma. 23, 104 (2022).
Martin, C. R. Definitions of necrotizing enterocolitis: What are we defining and is machine learning the answer? Pediatr. Res. 91, 488–489 (2021).
Jarman, A. Hierarchical cluster analysis: Comparison of single linkage, complete linkage, average linkage and centroid linkage method. (2020).
Espinosa, C. A. et al. Multiomic signals associated with maternal epidemiological factors contributing to preterm birth in low- and middle-income countries. Sci. Adv. 9, eade7692 (2023).
Jehan, F. et al. Multiomics characterization of preterm birth in low- and middle-income countries. JAMA Netw. Open 3, e2029655 (2020).
Ghaemi, M. S. et al. Multiomics modeling of the immunome, transcriptome, microbiome, proteome and metabolome adaptations during human pregnancy. Bioinformatics 35, 95–103 (2019).
Kelleher, S. T., McMahon, C. J. & James, A. Necrotizing Enterocolitis in children with congenital heart disease: a literature review. Pediatr. Cardiol. 42, 1688–1699 (2021).
Pammi, M. et al. Intestinal dysbiosis in preterm infants preceding necrotizing enterocolitis: a systematic review and meta-analysis. Microbiome 5, 31 (2017).
Funding
No financial assistance was received in support of this study.
Author information
Authors and Affiliations
Contributions
D.G., A.L., N.A., and J.N. contributed to conception and design of the study. D.G., A.L., S.M., T.G., and E.S. contributed significantly to the acquisition of data. A.C. and N.A. performed data analysis, used machine learning for hierarchal clustering, and performed statistical analysis. D.G., A.C., N.A., D.S., D.C., and J.N. were involved with drafting, revising, and final approval of the article.
Corresponding author
Ethics declarations
Competing interests
Dr. Aghaeepour is a member of the Scientific Advisory Boards of January AI, Parallel Bio, Celine Therapeutics, and WellSim Biomedical Technologies, is a paid consultant for MaraBio Systems, and is Cofounder and the Chief Scientist of Takeoff AI. Dr. Neu serves on the Scientific Advisory Boards of Astarte, Medela, and Arla Foods; serves on the Global Scientific Council for the Nestle Nutrition Institute; serves as a consultant for Glycome and Siolta Therapeutics; and has a research grant through Infant Bacterial Therapeutics. The remaining authors have no conflicts of interest to be reported.
Consent statement
Patient consent was not required to perform this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gipson, D.R., Chang, A.L., Lure, A.C. et al. Reassessing acquired neonatal intestinal diseases using unsupervised machine learning. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03074-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03074-x