Abstract
Background
Studies examining the association between in utero Zika virus (ZIKV) exposure and child neurodevelopmental outcomes have produced varied results.
Methods
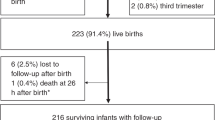
We aimed to assess neurodevelopmental outcomes among normocephalic children born from pregnant people enrolled in the Zika in Pregnancy in Honduras (ZIPH) cohort study, July–December 2016. Enrollment occurred during the first prenatal visit. Exposure was defined as prenatal ZIKV IgM and/or ZIKV RNA result at enrollment. Normocephalic children, >6 months old, were selected for longitudinal follow-up using the Bayley Scales of Infant and Toddler Development (BSID-III) and the Ages & Stages Questionnaires: Social-Emotional (ASQ:SE-2).
Results
One hundred fifty-two children were assessed; after exclusion, 60 were exposed and 72 were unexposed to ZIKV during pregnancy. Twenty children in the exposed group and 21 children in the unexposed group had a composite score <85 in any of the BSID-III domains. Although exposed children had lower cognitive and language scores, differences were not statistically significant. For ASQ:SE-2 assessment, there were not statistically significant differences between groups.
Conclusions
This study found no statistically significant differences in the neurodevelopment of normocephalic children between in utero ZIKV exposed and unexposed. Nevertheless, long-term monitoring of children with in utero ZIKV exposure is warranted.
Impact
-
This study found no statistically significant differences in the neurodevelopment in normocephalic children with in utero Zika virus exposure compared to unexposed children, although the exposed group showed lower cognitive and language scores that persisted after adjustment by maternal age and education and after excluding children born preterm and low birth weight from the analysis.
-
Children with prenatal Zika virus exposure, including those normocephalic and have no evidence of abnormalities at birth, should be monitored for neurodevelopmental delays. Follow-up is important to be able to detect developmental abnormalities that might not be detected earlier in life.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
John, C. C., Black, M. M. & Nelson, C. A. Neurodevelopment: the impact of nutrition and inflammation during early to middle childhood in low resource settings. Pediatrics 139, S59–S71 (2017).
Krauer, F. et al. Zika virus infection as a cause of congenital brain abnormalities and Guillain–Barré syndrome: systematic review. PLoS Med. 14, e1002203 (2017).
Marbán-Castro, E. et al. Neurodevelopment in normocephalic children exposed to Zika virus in utero with no observable defects at birth: a systematic review with meta-analysis. Int. J. Environ. Res. Public Health 19, 7319 (2022).
Lopes Moreira, M. E. et al. Neurodevelopment in infants exposed to Zika virus in utero. N. Engl. J. Med. 379, 2377–2379 (2018).
Nielsen-Saines, K. et al. Delayed childhood neurodevelopment and neurosensory alterations in the second year of life in a prospective cohort of ZIKV-exposed children. Nat. Med. 25, 1213–1217 (2019).
Cranston, J. S. et al. Association between antenatal exposure to Zika virus and anatomical and neurodevelopmental abnormalities in children. JAMA Netw. Open 3, e209303 (2020).
Mulkey, S. B. et al. Neurodevelopmental abnormalities in children with in utero Zika virus exposure without congenital Zika syndrome. JAMA Pediatr. 174, 269–276 (2020).
Valdes, V. et al. Cognitive development of infants exposed to the Zika virus in Puerto Rico. JAMA Netw. Open. 2, e1914061 (2019).
Blackmon, K. et al. Neurodevelopment in normocephalic children with and without prenatal Zika virus exposure. Arch. Dis. Child. 107, 244–250 (2022).
Buekens, P. et al. Zika virus infection in pregnant women in Honduras: study protocol. Reprod. Health 13, 82 (2016).
Alger, J. et al. Microcephaly outcomes among Zika virus-infected pregnant women in Honduras. Am. J. Trop. Med. Hyg. 104, 1737–1740 (2021).
Santiago, G. A. et al. Performance of the trioplex real-time RT-PCR assay for detection of Zika, dengue, and chikungunya viruses. Nat. Commun. 9, 1391 (2018).
Ward, M. J. et al. Zika virus and the World Health Organization criteria for determining recent infection using plaque reduction neutralization testing. Am. J. Trop. Med. Hyg. 99, 780–782 (2018).
Villar, J. et al. International standards for newborn weight, length, and head circumference by gestational age and sex: the newborn cross-sectional study of the INTERGROWTH-21st Project. Lancet 384, 857–868 (2014).
Bayley, N. Bayley-III: Bayley Scales of Infant and Toddler Development 3rd edn (Pearson, 2006).
Bayley, N. Spanish Adaptation of the Bayley Scales of Infant and Toddler Development 3rd edn (Pearson Educación S.A, 2015).
Squires, J., Bricker, D. & Twombly, E. Ages & Stages Questionnaires®: Social-Emotional, Second Edition (ASQ®:SE-2). A Parent-Completed Child Monitoring System for Social-emotional Behaviors (Brookes Publishing Co, 2015).
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 450, 76–85 (2006).
Ballot, D. E. et al. Use of the Bayley Scales of Infant and Toddler Development, Third Edition, to assess developmental outcome in infants and young children in an urban setting in South Africa. Int. Sch. Res. Notices. 2017, 1631760 (2017).
Squires, J., Bricker, D., Twombly, E., Murphy, K. & Hoselton, R. ASQ:SE-2 Technical Report. Tech Rep. 28 (2015).
Harris, P. A. et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381 (2009).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2021).
Grant, R. et al. In utero Zika virus exposure and neurodevelopment at 24 months in toddlers normocephalic at birth: a cohort study. BMC Med. 19, 12 (2021).
Gerzson, L. R. et al. Neurodevelopment of nonmicrocephalic children, after 18 months of life, exposed prenatally to Zika virus. J. Child. Neurol. 35, 278–282 (2020).
Sobral da Silva, P. F. et al. Neurodevelopment in children exposed to Zika virus: what are the consequences for children who do not present with microcephaly at birth? Viruses 13, 1427 (2021).
Ticona, J. et al. Developmental outcomes in children exposed to Zika virus in utero from a Brazilian urban slum cohort study. PLoS Negl. Trop. Dis. 15, e0009162 (2021).
Gonzalez, M. et al. ZEN Study Team. Cohort profile: congenital Zika virus infection and child neurodevelopmental outcomes in the ZEN cohort study in Colombia. Epidemiol. Health. 42, e2020060 (2020).
Marbán-Castro, E. et al. Zika virus infection in pregnant travellers and impact on childhood neurodevelopment in the first two years of life: a prospective observational study. Travel Med. Infect. Dis. 40, 101985 (2021).
Faiçal, A. V. et al. Neurodevelopmental delay in normocephalic children with in utero exposure to Zika virus. BMJ Paediatr. Open 3, e000486 (2019).
Tiene, S. F. et al. Early predictors of poor neurologic outcomes in a prospective cohort of infants with antenatal exposure to Zika virus. Pediatr. Infect. Dis. J. 41, 255–262 (2022).
Key, A. P. et al. A prospective study of neurodevelopmental trends between 3 and 24 months in normocephalic infants with prenatal Zika virus exposure: evidence of emerging communication delays in the NATZIG cohort. Early Hum. Dev. 163, 105470 (2021).
Mercado-Reyes, M. et al. Pregnancy, birth, infant, and early childhood neurodevelopmental outcomes among a cohort of women with symptoms of Zika virus disease during pregnancy in three surveillance sites, project Vigilancia de Embarazadas con Zika (VEZ), Colombia, 2016-2018. Trop. Med. Infect. Dis. 6, 183 (2021).
Peçanha, P. M. et al. Neurodevelopment of children exposed intra-uterus by Zika virus: a case series. PLoS ONE 15, e0229434 (2020).
Aizawa, C. Y. P. et al. Neurodevelopment in the third year of life in children with antenatal ZIKV-exposure. Rev. Saúde Pública 55, 15 (2021).
Einspieler, C. et al. Association of infants exposed to prenatal Zika virus infection with their clinical, neurologic, and developmental status evaluated via the General Movement Assessment Tool. JAMA Netw. Open. 2, e187235 (2019).
Stringer, E. M. et al. Neurodevelopmental outcomes of children following in utero exposure to Zika in Nicaragua. Clin. Infect. Dis. 72, e146–e153 (2021).
Mulkey, S. B. et al. Preschool neurodevelopment in Zika virus-exposed children without congenital Zika syndrome. Pediatr. Res. https://doi.org/10.1038/s41390-022-02373-5 (2022).
Griffin, I. et al. Zika virus IgM detection and neutralizing antibody profiles 12–19 months after illness onset. Emerg. Infect. Dis. 25, 299–303 (2019).
Basile, A. J. et al. Performance of InBios ZIKV Detect™ 2.0 IgM Capture ELISA in two reference laboratories compared to the original ZIKV Detect™ IgM Capture ELISA. J. Virol. Methods 271, 113671 (2019).
Waechter, R. et al. Improving neurodevelopment in Zika-exposed children: a randomized controlled trial. PLoS Negl. Trop. Dis. 16, e0010263 (2022).
Acknowledgements
We thank Karla Rivera and Renato Valenzuela, Instituto de Enfermedades Infecciosas y Parasitología Antonio Vidal, Tegucigalpa, Honduras, for their administrative support. We thank Andrea Meyer, Center for Emerging Reproductive and Perinatal Epidemiology (CERPE), Tulane University, New Orleans, Louisiana, USA, for editing this manuscript and administrative support.
Funding
The Zika in Pregnancy in Honduras (ZIPH) study is partially funded by Vysnova Partners SC-2018–3045-TU.
Author information
Authors and Affiliations
Contributions
P.B., V.T.T., J.A., M.L.C., E.W.H., S.M.G. and D.W. contributed to the conception and design of the research. R.L. examined the children and performed BSID-III and ASQ:SE-2 assessments. L.W., Allison C., M.C., J.F., F.R., Diana V., Douglas V., Z.A., M.B., H.B., C.B., Alejandra C., Alvaro C., J.G.A., K.G., L.G., S.M.G., E.W.H., G.H., W.L., M.T.L., Carlos M., Cynthia M., C.O., K.P., H.R., A.P.C., C.S., D.W., C.Z. and A.F.T. contributed to the acquisition, analysis and/or interpretation of data. K.G., I.L., L.P. and D.W. contributed to the performance and analysis of the laboratory tests. J.A., M.L.C., V.T.T., P.B., L.W., Diana V., S.M.G. and E.W.H. drafted and revised the manuscript. All authors reviewed and approved the submitted version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Tulane University, New Orleans, USA and the Faculty of Medical Sciences, Universidad Nacional Autónoma de Honduras (UNAH), Tegucigalpa, Honduras, institutional review boards. Informed consent was obtained from parents or caretakers of all participating children. As described, all methods and procedures were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alger, J., Cafferata, M.L., López, R. et al. Neurodevelopmental assessment of normocephalic children born to Zika virus exposed and unexposed pregnant people. Pediatr Res 95, 566–572 (2024). https://doi.org/10.1038/s41390-023-02951-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02951-1
This article is cited by
-
Trends in prenatal and pediatric viral infections, and the impact of climate change
Pediatric Research (2024)