Abstract
Background
We aimed to evaluate the predictors of sustainability of biologic drugs for paediatric patients with Crohn’s disease (CD).
Methods
The Czech National Prospective Registry of Biologic and Targeted Therapy of Inflammatory Bowel Disease (CREdIT) was used to identify the biologic treatment courses in paediatric patients with CD. Mixed-effects Cox models and propensity score analyses were employed to evaluate predictors of treatment sustainability.
Results
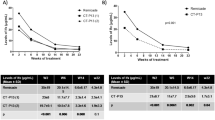
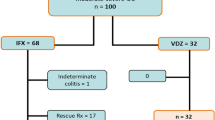
Among the 558 observations of 473 patients, 264 were treated with adalimumab (47%), 240 with infliximab (43%), 41 with ustekinumab (7%), and 13 with vedolizumab (2%). Multivariable analysis revealed higher discontinuation risk with infliximab compared to adalimumab (HR = 0.600, 95%CI 0.389–0.926), both overall and in first-line treatment (HR = 0.302, 95%CI 0.103–0.890). Infliximab versus adalimumab was associated with shorter time to escalation (HR = 0.094, 95%CI 0.043–0.203). Propensity-score analysis demonstrated lower sustainability of infliximab (HR = 0.563, 95%CI 1.159–2.725). The time since diagnosis to treatment initiation (HR = 0.852, 95%CI 0.781–0.926) was the most important predictor. Baseline immunosuppressive therapy prolonged sustainability with infliximab (HR = 2.899, 95%CI 1.311–6.410).
Conclusions
Given the results suggesting shorter sustainability, the need for earlier intensification and thus higher drug exposure, and the greater need for immunosuppression with infliximab than with adalimumab, the choice of these drugs cannot be considered completely equitable.
Impact
-
Our study identified predictors of sustainability of biologic treatment in paediatric patients with Crohn’s disease, including adalimumab (versus infliximab), early initiation of biologic treatment, and normalised baseline haemoglobin levels. Infliximab treatment was associated with earlier intensification, higher drug exposure, and a greater need for immunosuppression.
-
Parents and patients should be fully informed of the disadvantages of intravenous infliximab versus adalimumab during the decision-making process.
-
This study emphasises the importance of not delaying the initiation of biologic therapy in paediatric patients with Crohn’s disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Qiu, Y. et al. Systematic review with meta-analysis: loss of response and requirement of Anti-Tnfalpha dose intensification in Crohn’s Disease. J. Gastroenterol. 52, 535–554 (2017).
Schultheiss, J. P. D. et al. Loss of response to Anti-Tnfalpha agents depends on treatment duration in patients with inflammatory bowel disease. Aliment. Pharm. Ther. 54, 1298–1308 (2021).
Bronsky, J. et al. Adalimumab vs infliximab in pediatric patients with Crohn’s disease: a propensity score analysis and predictors of treatment escalation. Clin. Transl. Gastroenterol. 13, e00490 (2022).
Kaplan, J. L. et al. Use, durability, and risks for discontinuation of initial and subsequent biologics in a large pediatric-onset Ibd Cohort. J. Pediatr. Gastroenterol. Nutr. 76, 566–575 (2023).
Jongsma, M. M. E. et al. First-line treatment with infliximab versus conventional treatment in children with newly diagnosed moderate-to-severe Crohn’s Disease: an open-label multicentre randomised controlled trial. Gut 71, 34–42 (2022).
Lauriot Dit Prevost, C. et al. Bowel damage and disability in crohn’s disease: a prospective study in a tertiary referral centre of the lemann index and inflammatory bowel disease disability index. Aliment. Pharm. Ther. 51, 889–898 (2020).
Kerur, B. et al. Biologics delay progression of Crohn’s disease, but not early surgery, in children. Clin. Gastroenterol. Hepatol. 16, 1467–1473 (2018).
Powers JM. Approach to the child with anemia. In: UpToDate, Post TW (Ed), Wolters Kluwer. https://www.uptodate.com. (Accessed on July 20, 2023).
Singh, S. et al. Comparative effectiveness and safety of anti-tumor necrosis factor agents in biologic-naive patients with Crohn’s disease. Clin. Gastroenterol. Hepatol. 14, 1120–1129.e1126 (2016).
Di Domenicantonio, R. et al. Population-based cohort study on comparative effectiveness and safety of biologics in inflammatory bowel disease. Clin. Epidemiol. 10, 203–213 (2018).
Ananthakrishnan, A. N. et al. Comparative effectiveness of infliximab and adalimumab in Crohn’s disease and ulcerative colitis. Inflamm. Bowel Dis. 22, 880–885 (2016).
Nuti, F. et al. Prospective evaluation of the achievement of mucosal healing with Anti-Tnf-Alpha therapy in a paediatric Crohn’s disease cohort. J. Crohns Colitis 10, 5–12 (2016).
Li, S., Reynaert, C., Su, A. L. & Sawh, S. Efficacy and safety of infliximab in pediatric crohn disease: a systematic review and meta-analysis. Can. J. Hosp. Pharm. 72, 227–238 (2019).
Atia, O. et al. Dop45 utilization and sustainability of biologics in Cd - a nationwide study from the Epi-Iirn. J. Crohn’s Colitis 15, S082–S083 (2021).
Hyams, J. et al. Induction and maintenance infliximab therapy for the treatment of moderate-to-severe Crohn’s Disease in children. Gastroenterology 132, 863–873 (2007).
Hyams, J. S. et al. Safety and efficacy of adalimumab for moderate to severe Crohn’s disease in children. Gastroenterology 143, 365–374.e362 (2012).
Schreiber, S. et al. Randomized controlled trial: subcutaneous vs intravenous infliximab Ct-P13 maintenance in inflammatory bowel disease. Gastroenterology 160, 2340–2353 (2021).
Bittner, B., Richter, W. & Schmidt, J. Subcutaneous administration of biotherapeutics: an overview of current challenges and opportunities. BioDrugs 32, 425–440 (2018).
Sandborn, W. J. et al. Efficacy and safety of vedolizumab subcutaneous formulation in a randomized trial of patients with ulcerative colitis. Gastroenterology 158, 562–572.e512 (2020).
Baumgart, D. C. & Le Berre, C. Newer biologic and small-molecule therapies for inflammatory bowel disease. N. Engl. J. Med. 385, 1302–1315 (2021).
Matsumoto, T. et al. Adalimumab monotherapy and a combination with azathioprine for Crohn’s disease: a prospective, randomized trial. J. Crohns Colitis 10, 1259–1266 (2016).
Colombel, J. F. et al. Infliximab, Azathioprine, or combination therapy for Crohn’s disease. N. Engl. J. Med. 362, 1383–1395 (2010).
Colombel, J. F. et al. Combination therapy with infliximab and azathioprine improves infliximab pharmacokinetic features and efficacy: a post hoc analysis. Clin. Gastroenterol. Hepatol. 17, 1525–1532.e1521 (2019).
Feagan, B. G. et al. Methotrexate in combination with infliximab is no more effective than infliximab alone in patients with Crohn’s Disease. Gastroenterology 146, 681–688 e681 (2014).
Kierkus, J. et al. Monotherapy with infliximab versus combination therapy in the maintenance of clinical remission in children with moderate to severe Crohn Disease. J. Pediatr. Gastroenterol. Nutr. 60, 580–585 (2015).
Hamdeh, S. et al. Early vs late use of anti-tnfa therapy in adult patients with crohn disease: a systematic review and meta-analysis. Inflamm. Bowel Dis. 26, 1808–1818 (2020).
van Rheenen, P. F. et al. The medical management of paediatric Crohn’s disease: an ecco-espghan guideline update. J. Crohns Colitis 15, 171–194 (2020).
Hradsky, O. et al. Risk factors for dermatological complications of Anti-Tnf therapy in a cohort of children with Crohn’s disease. Eur. J. Pediatr. 180, 3001–3008 (2021).
Freling, E. et al. Cumulative incidence of, risk factors for, and outcome of dermatological complications of Anti-Tnf therapy in inflammatory bowel disease: a 14-Year experience. Am. J. Gastroenterol. 110, 1186–1196 (2015).
Nigam, G. B., Bhandare, A. P., Antoniou, G. A. & Limdi, J. K. Systematic review and meta-analysis of dermatological reactions in patients with inflammatory bowel disease treated with anti-tumour necrosis factor therapy. Eur. J. Gastroenterol. Hepatol. 33, 346–357 (2021).
Hyams, J. S. et al. Long-term outcome of maintenance infliximab therapy in children with Crohn’s disease. Inflamm. Bowel Dis. 15, 816–822 (2009).
Sridhar, S., Maltz, R. M., Boyle, B. & Kim, S. C. Dermatological manifestations in pediatric patients with inflammatory bowel diseases on anti-tnf therapy. Inflamm. Bowel Dis. 24, 2086–2092 (2018).
Lerchova, T. et al. Prediction of Thiopurine failure in pediatric crohn’s disease: pediatric ibd porto group of espghan. Pediatr Res. 93, 1659–1666 (2023).
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing. We would also like to thank Institute of Biostatistics and Analyses for operating the CREDIT Registry. This work was supported by the Grant Agency of Charles University in Prague (grant number 227023) and the Ministry of Health, Czech Republic, for the conceptual development of the research organisations (00064203, University Hospital Motol, Prague, Czech Republic).
Author information
Authors and Affiliations
Contributions
O.H.: Created the conception, study design and data analysis, patient recruitment, first draught of the paper. I.C.: Patient recruitment and revision of the original article. M.D.: Patient recruitment and revision of the original article. D.K.: Patient recruitment and revision of the original article. T.L.: Patient recruitment and revision of the original article. K.M.: Patient recruitment and revision of the original article. J.S.: Patient recruitment and revision of the original article. R.V.: Patient recruitment and revision of the original article. N.L.: Patient recruitment and revision of the original article. E.K.: Patient recruitment and revision of the original article. M.V.V.: Patient recruitment and revision of the original article. A.S.: Patient recruitment and revision of the original article. L.G.: Patient recruitment and revision of the original article. M.V.: Patient recruitment and revision of the original article. I.Z.: Patient recruitment and revision of the original article. M.Z.: Patient recruitment and revision of the original article. M.B.: Leading the registry, patient recruitment and revision of the original article. J.B.: Leading the project team, patient recruitment and revision of the original article.
Corresponding author
Ethics declarations
Competing interests
O.H.: lectures/congress fees/consultancy (outside the scope of the submitted work; MSD, AbbVie, Takeda, Sandoz, Nutricia, Nestlé, and Ferring). I.C.: no conflict. M.D.: congress fees (outside the scope of the submitted work; Nutricia, Nestlé). D.K.: congress fee (outside the scope of the submitted work; Takeda). T.L.: lectures/congress fees/consultancy (outside the scope of the submitted work; Ferring, Nutricia, Biocodex, and AbbVie). K.M.: lectures/congress fees/consultancy (outside the scope of the submitted work; Takeda, Janssen-Cilag). J.S.: lectures/congress fees (AstraZeneca, AbbVie, Nestlé, Nutricia, MSD, and Takeda). R.V.: congress fees (outside submitted work; AbbVie, Nestlé). N.L.: lectures/congress fees/consultancy (outside the scope of the submitted work; AbbVie, Sandoz, Nutricia, Nestlé). E.K.: lectures/congress fees/consultancy (outside the scope of the submitted work; AbbVie, Nutricia, and Nestlé). M.V.V.: lectures, congress fees (outside submitted work) - Nestlé, Nutricia. A.S.: Lectures/congress fees/consultancy —AbbVie, Takeda, Nutricia, Nestlé. L.G.: no conflict. M.V.: no conflict. I.Z.: no conflict. M.Z.: no conflict. M.B.: lectures/congress fees/consultancy (outside the scope of the submitted work; Abbvie, Takeda, Janssen-Cilag, Celltrion, Roche, AstraZeneca, Biogen, Tillotts, Ferring, Alfasigma, PRO.MED.CS, Sandoz, Bristol-Myers Squibb, Pfizer, and Swedish Orphan Biovitrum). J.B.: lectures/congress fees/consultancy (outside the scope of the submitted work; MSD, AbbVie, Sandoz, Danone-Nutricia, and Nestlé).
Ethicas approval and consent for participate
This study was approved by the Ethics Committee (EK - 440/30) and all parents or participants provided informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hradsky, O., Copova, I., Durilova, M. et al. Sustainability of biologic treatment in paediatric patients with Crohn’s disease: population-based registry analysis. Pediatr Res (2023). https://doi.org/10.1038/s41390-023-02913-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-023-02913-7