Abstract
Background
To analyze the clinical characteristics and outcomes of children with severe neurological symptoms associated with the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection during the Omicron pandemic in China.
Methods
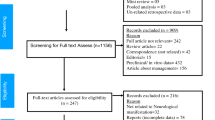
This study used a questionnaire to obtain data from pediatric intensive care unit (PICU) centers in seven tertiary hospitals in Northeast China from December 1, 2022, to January 31, 2023.
Results
A total of 255 patients were confirmed to have SARS-CoV-2 infection, and 45 patients (17.65 %) were included in this study. Of these, seven (15.6%) patients died, and the median time from admission to death was 35 h (IQR, 14–120 h). Twenty (52.6%) survivors experienced neurological sequelae. Patients with platelet counts lower than 100 × 109/L had a higher incidence of complications such as multiple organ dysfunction, mechanical ventilation rate, and mortality. Cranial magnetic resonance imaging (MRI) always reveals cerebral tissue edema, with some severe lesions forming a softening site.
Conclusion
Children infected with SARS-CoV-2 often exhibit severe neurological symptoms, and in some cases, they may rapidly develop malignant cerebral edema or herniation, leading to a fatal outcome. An early decrease in platelet count may associated with an unfavorable prognosis.
Impact
-
Since early December 2022, China has gradually adjusted its prevention and control policy of SARS-CoV-2; Omicron outbreaks have occurred in some areas for a relatively short period. Due to the differences in ethnicity, endemic strains and vaccination status, there was a little difference from what has been reported about children with SARS-CoV-2 infection with severe neurological symptoms in abroad. This is the first multicenter clinical study in children with nervous system involvement after acute SARS-CoV-2 infection in China, and helpful for pediatricians to have a more comprehensive understanding of the clinical symptoms and prognosis of such disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All authors agreed that the data and materials mentioned in this article are true and availability. The datasets used and/or analyzed during the current study available from the appendix.
References
Wang, L. et al. Comparison of outcomes from covid infection in pediatric and adult patients before and after the emergence of omicron. medRxiv https://doi.org/10.1101/2021.12.30.21268495 (2022).
Viana, R. et al. Rapid epidemic expansion of the SARS-cov-2 omicron variant in southern africa. Nature 603, 679–686 (2022).
Lin, J. E. et al. Neurological issues in children with covid-19. Neurosci. Lett. 743, 135567 (2021).
Schober, M. E., Pavia, A. T. & Bohnsack, J. F. Neurologic manifestations of covid-19 in children: emerging pathophysiologic insights. Pediatr. Crit. Care Med. 22, 655–661 (2021).
Lewis, A. et al. Cerebrospinal fluid in covid-19: a systematic review of the literature. J. Neurol. Sci. 421, 117316 (2021).
Stafstrom, C. E. & Jantzie, L. L. Covid-19: neurological considerations in neonates and children. Children 7. https://doi.org/10.3390/children7090133 (2020).
Franke, C. et al. High frequency of cerebrospinal fluid autoantibodies in covid-19 patients with neurological symptoms. Brain Behav. Immun. 93, 415–419 (2021).
Nordvig, A. S. et al. Potential neurologic manifestations of covid-19. Neurol. Clin. Pract. 11, e135–e146 (2021).
Smadja, D. M. et al. Covid-19 is a systemic vascular hemopathy: insight for mechanistic and clinical aspects. Angiogenesis 24, 755–788 (2021).
Thakur, K. T. et al. Covid-19 neuropathology at columbia university irving medical center/new york presbyterian hospital. Brain 144, 2696–2708 (2021).
Mizuguchi, M. et al. Acute necrotising encephalopathy of childhood: a new syndrome presenting with multifocal, symmetric brain lesions. J. Neurol. Neurosurg. Psychiatry 58, 555–561 (1995).
Michael, B. D. et al. Consensus clinical guidance for diagnosis and management of adult COVID-19 encephalopathy patients. J. Neuropsychiatry Clin. Neurosci. 35, 12–27 (2023).
Garcia-Vera, C. et al. Covid-19 in children: clinical and epidemiological spectrum in the community. Eur J. Pediatr. 181, 1235–1242 (2022).
Cui, X. et al. A systematic review and meta-analysis of children with coronavirus disease 2019 (covid-19). J. Med. Virol. 93, 1057–1069 (2021).
Moreira, A. et al. Demographic predictors of hospitalization and mortality in us children with covid-19. Eur. J. Pediatr. 180, 1659–1663 (2021).
Ranabothu, S. et al. Spectrum of covid-19 in children. Acta Paediatr. 109, 1899–1900 (2020).
Lee, P. Y. et al. Distinct clinical and immunological features of SARS-cov-2-induced multisystem inflammatory syndrome in children. J. Clin. Investig. 130, 5942–5950 (2020).
Panda, P. K. et al. Neurological complications of SARS-cov-2 infection in children: a systematic review and meta-analysis. J. Trop. Pediatr. 67. https://doi.org/10.1093/tropej/fmaa070 (2021).
Nepal, G. et al. Neurological manifestations of covid-19 associated multi-system inflammatory syndrome in children: a systematic review and meta-analysis. J. Nepal Health Res. Counc. 19, 10–18 (2021).
Abdel-Mannan, O. et al. Neurologic and radiographic findings associated with covid-19 infection in children. Jama Neurol. 77, 1440–1445 (2020).
Ray, S. T. J. et al. Neurological manifestations of SARS-cov-2 infection in hospitalised children and adolescents in the uk: a prospective national cohort study. Lancet Child Adolesc. Health 5, 631–641 (2021).
LaRovere, K. L. et al. Neurologic involvement in children and adolescents hospitalized in the united states for covid-19 or multisystem inflammatory syndrome. Jama Neurol. 78, 536 (2021).
Xiao, L., Ran, X., Zhong, Y. & Li, S. Clinical value of blood markers to assess the severity of coronavirus disease 2019. BMC Infect. Dis. 21, 1471–2334 (2021).
Zhao, X. et al. Early decrease in blood platelet count is associated with poor prognosis in COVID-19 patients-indications for predictive, preventive, and personalized medical approach. EPMA J. 11, 139–145 (2020).
Gorog, D. A. et al. Current and novel biomarkers of thrombotic risk in COVID-19: a Consensus Statement from the International COVID-19 Thrombosis Biomarkers Colloquium. Nat. Rev. Cardiol. 19, 475–495 (2022).
Overmyer, K. A. et al. Large-scale multi-omic analysis of COVID-19 severity. Cell Syst. 12, 23–40 (2021).
Liao, D. et al. Haematological characteristics and risk factors in the classification and prognosis evaluation of COVID-19: a retrospective cohort study. Lancet Haematol. 7, e671–e678 (2020).
Henry, B. M., de Oliveira, M., Benoit, S., Plebani, M. & Lippi, G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin. Chem. Lab. Med. 58, 1021–1028 (2020).
COVID-19 Forecasting Team. Past SARS-cov-2 infection protection against re-infection: a systematic review and meta-analysis. Lancet 401, 833–842 (2023).
Tenforde, M. W. et al. Vaccine effectiveness against influenza-associated urgent care, emergency department, and hospital encounters during the 2021-2022 season, vision network. J. Infect. Dis. https://doi.org/10.1093/infdis/jiad015 (2023).
Adams, K. et al. Prevalence of SARS-cov-2 and influenza coinfection and clinical characteristics among children and adolescents aged <18 years who were hospitalized or died with influenza - united states, 2021-22 influenza season. MMWR Morb. Mortal Wkly Rep. 71, 1589–1596 (2022).
Funding
This work was supported by the Major science and technology Project of Liaoning Province (No. 2020JH1/10300001 to Chun-Feng Liu); the Natural Science Foundation of Liaoning Province (No. 2023-MS-191 to T.Z.), and 345 Talent Project of Shengjing Hospital of China Medical University (C.-F.L. and T.Z.).
Author information
Authors and Affiliations
Contributions
T.Z., and C.F.L, conceived and designed the study. T.Z., Q.F.Z., H.M.Y., P.L., P.S., Y.M.L., Z.Z., Y.Z.H., X.Y.Y., Q.Q.G.C.L.M. and Q.S., collected all the data. T.Z. analyzed the data. All authors participated in drafting or revising of the manuscript, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study was approved by the Ethics Committee of Shengjing Hospital of China Medical University (2023PS434K), and the patient consent was not required in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, T., Zhang, QF., Yang, HM. et al. Children with severe neurological symptoms associated with SARS-CoV-2 infection during Omicron pandemic in China. Pediatr Res 95, 1088–1094 (2024). https://doi.org/10.1038/s41390-023-02904-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02904-8
This article is cited by
-
Neurological manifestations and risk factors associated with poor prognosis in hospitalized children with Omicron variant infection
European Journal of Pediatrics (2024)