Abstract
Background
Infants born less than 29 weeks, or extremely preterm (EPT), experience increased morbidity and mortality. We hypothesized that exposure to maternal infection might contribute to neurodevelopmental impairment (NDI) or death at 2 years of age.
Methods
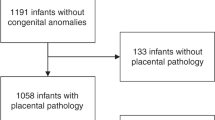
We conducted a retrospective cohort study of EPT infants from January 2010 to December 2020. Maternal data extracted included maternal infections, classified as extrauterine or intrauterine. Placental pathologic and infant data were extracted. The primary outcome was NDI or death at 2 years of age.
Results
548 EPT infants were born to 496 pregnant people: 379 (69%) were not exposed to any documented maternal infection prenatally, 124 (23%) to extrauterine infection, and 45 (8%) to intrauterine infection. Neither diagnosis of maternal extrauterine nor intrauterine infection was associated with NDI or death at 2 years of age (p > 0.05). Acute histologic chorioamnionitis was associated with NDI or death at 2 years of age (p = 0.033).
Conclusions
Maternal infection was not associated with NDI or death at 2 years of age in EPT infants. However, acute histologic chorioamnionitis was associated with this outcome. Further work should investigate the differential influence of infection and immune response with this pathology as relates to outcomes in EPT infants.
Impact
-
Maternal infection was not associated with neurodevelopmental impairment (NDI) or death at 2 years of age in extremely preterm (EPT) infants. This is reassuring support that mechanisms at the maternal-fetal interface largely protect the EPT infant.
-
However, pathologic findings of acute histologic chorioamnionitis were associated with NDI and death at 2 years of age.
-
Further work should investigate the differential influence of infection and immune response with acute histologic chorioamnionitis on pathology as relates to outcomes in EPT infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Patel, R. M. Short- and Long-Term Outcomes for Extremely Preterm Infants. Am. J. Perinatol. 33, 318–328 (2016).
Stoll, B. J. et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126, 443–456 (2010).
Patel, R. M. et al. Causes and timing of death in extremely premature infants from 2000 through 2011. N. Engl. J. Med. 372, 331–340 (2015).
Tang, Q., Zhang, L., Li, H. & Shao, Y. The fetal inflammation response syndrome and adverse neonatal outcomes: a meta-analysis. J. Matern Fetal Neonatal Med. 34, 3902–3914 (2021).
Francis, F. et al. Fetal inflammatory response syndrome (FIRS) and outcome of preterm neonates - a prospective analytical study. J. Matern Fetal Neonatal Med. 32, 488–492 (2019).
Yoon, B. H. et al. Fetal exposure to an intra-amniotic inflammation and the development of cerebral palsy at the age of three years. Am. J. Obstet. Gynecol. 182, 675–681 (2000).
Hill, J. B., Sheffield, J. S., McIntire, D. D. & Wendel, G. D., Jr. Acute Pyelonephritis in Pregnancy. Obstet. Gynecol. 105, 18–23 (2005).
Dingens, A. S., Fairfortune, T. S., Reed, S. & Mitchell, C. Bacterial vaginosis and adverse outcomes among full-term infants: a cohort study. BMC Pregnancy Childbirth 16, 278 (2016).
Huang, J. et al. Antenatal infection and intraventricular hemorrhage in preterm infants: A meta-analysis. Medicine. 98, e16665 (2019).
Bierstone, D. et al. Association of Histologic Chorioamnionitis With Perinatal Brain Injury and Early Childhood Neurodevelopmental Outcomes Among Preterm Neonates. JAMA Pediatr. 172, 534–541 (2018).
Vohr, B. R. et al. Are outcomes of extremely preterm infants improving? Impact of Bayley assessment on outcomes. J. Pediatr. 161, 222–8.e3 (2012).
Mir, I. N. et al. Impact of multiple placental pathologies on neonatal death, bronchopulmonary dysplasia, and neurodevelopmental impairment in preterm infants. Pediatr. Res. 87, 885–891 (2020).
Stoll, B. J. et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993-2012. Jama 314, 1039–1051 (2015).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 187, 1–7 (1978).
Redline, R. W., Heller, D., Keating, S. & Kingdom, J. Placental diagnostic criteria and clinical correlation-a workshop report. Placenta 26, S114–S117 (2005).
Greer, L. G. et al. An immunologic basis for placental insufficiency in fetal growth restriction. Am. J. Perinatol. 29, 533–538 (2012).
Mir, I. N. et al. Placental pathology is associated with severity of neonatal encephalopathy and adverse developmental outcomes following hypothermia. Am. J. Obstet. Gynecol. 213, 849.e1–7 (2015).
Khong, T. Y. et al. Sampling and Definitions of Placental Lesions: Amsterdam Placental Workshop Group Consensus Statement. Arch. Pathol. Lab Med. 140, 698–713 (2016).
Goldenberg, R. L., Hauth, J. C. & Andrews, W. W. Intrauterine infection and preterm delivery. N. Engl. J. Med. 342, 1500–1507 (2000).
Goldenberg, R. L., Culhane, J. F., Iams, J. D. & Romero, R. Epidemiology and causes of preterm birth. Lancet 371, 75–84 (2008).
Romero, R. et al. The preterm parturition syndrome. Bjog 113, 17–42 (2006).
Romero, R. et al. The role of infection in preterm labour and delivery. Paediatr. Perinat. Epidemiol. 15, 41–56 (2001).
Watterberg, K. L., Demers, L. M., Scott, S. M. & Murphy, S. Chorioamnionitis and early lung inflammation in infants in whom bronchopulmonary dysplasia develops. Pediatrics 97, 210–215 (1996).
Been, J. V. et al. Chorioamnionitis alters the response to surfactant in preterm infants. J. Pediatr. 156, 10–15.e1 (2010).
Green, C. A. et al. Association of chorioamnionitis and patent ductus arteriosus in a national U.S. cohort. J. Perinatol. 41, 119–125 (2021).
Park, H. W., Choi, Y. S., Kim, K. S. & Kim, S. N. Chorioamnionitis and Patent Ductus Arteriosus: A Systematic Review and Meta-Analysis. PLoS One 10, e0138114 (2015).
Kim, C. J. et al. Acute chorioamnionitis and funisitis: definition, pathologic features, and clinical significance. Am. J. Obstet. Gynecol. 213, S29–S52 (2015).
Megli, C. J. & Coyne, C. B. Infections at the maternal-fetal interface: an overview of pathogenesis and defence. Nat. Rev. Microbiol. 20, 67–82 (2022).
Ander, S. E., Diamond, M. S., Coyne, C. B. Immune responses at the maternal-fetal interface. Sci Immunol. 4 https://doi.org/10.1126/sciimmunol.aat6114 (2019).
Clark, E. A. et al. Association of fetal inflammation and coagulation pathway gene polymorphisms with neurodevelopmental delay at age 2 years. Am. J. Obstet. Gynecol. 203, 83.e1–83.e10 (2010).
García-Muñoz Rodrigo, F., Galán Henríquez, G. M. & Ospina, C. G. Morbidity and mortality among very-low-birth-weight infants born to mothers with clinical chorioamnionitis. Pediatr. Neonatol. 55, 381–386 (2014).
Rees, S., Harding, R. & Walker, D. The biological basis of injury and neuroprotection in the fetal and neonatal brain. Int. J. Dev. Neurosci. 29, 551–563 (2011).
Schlapbach, L. J. et al. Impact of sepsis on neurodevelopmental outcome in a Swiss National Cohort of extremely premature infants. Pediatrics 128, e348–e357 (2011).
Shi, Z., et al. Chorioamnionitis in the Development of Cerebral Palsy: A Meta-analysis and Systematic Review. Pediatrics. 139 https://doi.org/10.1542/peds.2016-3781 (2017).
Ylijoki, M. K., Ekholm, E., Ekblad, M. & Lehtonen, L. Prenatal Risk Factors for Adverse Developmental Outcome in Preterm Infants-Systematic Review. Front Psychol. 10, 595 (2019).
Mir, I. N. et al. Autism spectrum disorders in extremely preterm infants and placental pathology findings: a matched case-control study. Pediatr. Res. 89, 1825–1831 (2021).
Raghavan, R. et al. Preterm birth subtypes, placental pathology findings, and risk of neurodevelopmental disabilities during childhood. Placenta 83, 17–25 (2019).
Venkatesh, K. K. et al. Histologic chorioamnionitis and risk of neurodevelopmental impairment at age 10 years among extremely preterm infants born before 28 weeks of gestation. Am. J. Obstet. Gynecol. 223, 745.e1–745.e10 (2020).
Acknowledgements
The authors thank Pollieanna Sepulveda for her assistance in data extraction, and Dr. Catherine Spong for her overall guidance on the project. This research was made possible through internal funding. C.L.H. is supported by grants K23HD103876 and L30HD109864.
Author information
Authors and Affiliations
Contributions
Each author listed has meet the following criteria: substantial contributions to conception and design (C.L.H., I.M.), acquisition of data (C.L.H., I.M., P.S.K.), or analysis and interpretation of data (all authors); drafting the article or revising it critically for important intellectual content (all authors); and final approval of the version to be published (all authors).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Herrera, C.L., Kadari, P.S., Pruszynski, J.E. et al. Impact of maternal infection on outcomes in extremely preterm infants. Pediatr Res 95, 573–578 (2024). https://doi.org/10.1038/s41390-023-02898-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02898-3
This article is cited by
-
Trends in prenatal and pediatric viral infections, and the impact of climate change
Pediatric Research (2024)