Abstract
Background
Few studies have evaluated the differential benefits of breastfeeding on infant neurodevelopment at varying levels of prenatal alcohol exposure (PAE). This study examined whether the association between breastfeeding and neurodevelopment is modified by prenatal drinking pattern.
Methods
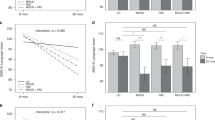
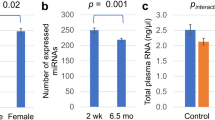
The study included 385 infants from Ukraine born to women prospectively enrolled in a cohort study during pregnancy. Neurodevelopment was assessed at six and 12 months using the Bayley Scales of Infant Development II (BSID-II) Mental Developmental Index (MDI) and Psychomotor Developmental Index (PDI). Linear regression modeling with interaction terms and stratification by PAE group was used to determine the relationship between breastfeeding, PAE, and neurodevelopment.
Results
A significant interaction between PAE and breastfeeding was observed for the MDI and PDI at six and 12 months. Infants with high PAE who were breastfed at least four months had BSID-II scores 14 or more points higher compared to those never breastfed. Counterintuitively, those with moderate PAE had poorer performance on the BSID-II at 12 months when breastfed longer.
Conclusion
There was a significant joint effect of PAE and breastfeeding on infant neurodevelopment at six and 12 months. Breastfeeding may provide distinct benefits to infants exposed to high levels of PAE.
Impact
-
We found a positive effect of breastfeeding on infant neurodevelopment among infants with prenatal alcohol exposure (PAE), particularly those exposed to higher levels during gestation.
-
This study is one of the first to evaluate whether breastfeeding mitigates harm caused by PAE.
-
Breastfeeding may provide distinct benefits to infants with higher levels of PAE.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The data used in this analysis can be accessed following approved application to the CIFASD data sharing committee. https://cifasd.org/data-sharing/.
References
Bandoli, G. et al. Patterns of prenatal alcohol use that predict infant growth and development. Pediatrics 143, e20182399 (2019).
Mattson, S. N., Bernes, G. A. & Doyle, L. R. Fetal alcohol spectrum disorders: a review of the neurobehavioral deficits associated with prenatal alcohol exposure. Alcohol Clin. Exp. Res. 43, 1046–1062 (2019).
Flak, A. L. et al. The association of mild, moderate, and binge prenatal alcohol exposure and child neuropsychological outcomes: a meta-analysis. Alcohol Clin. Exp. Res. 38, 214–226 (2014).
Richardson, G. A., Day, N. L. & Goldschmidt, L. Prenatal alcohol, marijuana, and tobacco use: infant mental and motor development. Neurotoxicol. Teratol. 17, 479–487 (1995).
Carter, R. C. et al. Fetal alcohol growth restriction and cognitive impairment. Pediatrics 138, e20160775 (2016).
Jedrychowski, W. et al. Effect of exclusive breastfeeding on the development of children’s cognitive function in the Krakow prospective birth cohort study. Eur. J. Pediatr. 171, 151–158 (2012).
Hou, L. et al. Impact of the duration of breastfeeding on the intelligence of children: A systematic review with network meta-analysis. Breastfeed. Med. 16, 687–696 (2021).
Leventakou, V. et al. Breastfeeding duration and cognitive, language and motor development at 18 months of age: Rhea mother–child cohort in Crete, Greece. J. Epidemiol. Community Health 69, 232–239 (2015).
Belfort, M. B. The science of breastfeeding and brain development. Breastfeed. Med. 12, 459–461 (2017).
Horta, B. L., Victora, C. G., World Health Organization. Long-Term Effects of Breastfeeding: a Systematic Review. World Health Organization; 2013. Published April 10, 2013. Accessed May 7, https://apps.who.int/iris/handle/10665/79198 2023.
Horta, B. L., Loret de Mola, C. & Victora, C. G. Breastfeeding and intelligence: a systematic review and meta-analysis. Acta Paediatr. 104, 14–19 (2015).
McCrory, C. & Murray, A. The effect of breastfeeding on neuro-development in infancy. Matern. Child Health J. 17, 1680–1688 (2013).
World Health Organization. Infant and young child feeding. World Health Organization. Published June 9, 2021. Accessed May 7, https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding 2023.
Centers for Disease Control and Prevention. Breastfeeding FAQs. Centers for Disease Control and Prevention. Published March 2, 2022. Updated August 4, 2022. Accessed May 7, https://www.cdc.gov/breastfeeding/faq/index.htm 2023.
May, P. A. et al. Breastfeeding and maternal alcohol use: prevalence and effects on child outcomes and fetal alcohol spectrum disorders. Reprod. Toxicol. 63, 13–21 (2016).
Wilson, J. et al. Alcohol consumption by breastfeeding mothers: frequency, correlates and infant outcomes. Drug Alcohol Rev. 36, 667–676 (2017).
Hoyme, H. E. et al. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics 138, e20154256 (2016).
Chambers, C. D. et al. Prevalence and predictors of maternal alcohol consumption in 2 regions of Ukraine. Alcohol Clin. Exp. Res. 38, 1012–1019 (2014).
Bandoli, G. et al. Assessing the independent and joint effects of unmedicated prenatal depressive symptoms and alcohol consumption in pregnancy and infant neurodevelopmental outcomes. Alcohol Clin. Exp. Res. 40, 1304–1311 (2016).
Coles, C. D. et al. Dose and timing of prenatal alcohol exposure and maternal nutritional supplements: developmental effects on 6-month-old infants. Matern. Child Health J. 19, 2605–2614 (2015).
About Us: Our Mission. Collaborative Initiative on Fetal Alcohol Spectrum Disorders (CIFASD). Published 2016. Accessed May 7, https://cifasd.org/about/ 2023.
Bandoli, G. et al. Patterns of prenatal alcohol exposure and alcohol‐related dysmorphic features. Alcohol Clin. Exp. Res. 44, 2045–2052 (2020).
Garrison, L., Morley, S., Chambers, C. D. & Bakhireva, L. N. Forty years of assessing neurodevelopmental and behavioral effects of prenatal alcohol exposure in infants: what have we learned? Alcohol Clin. Exp. Res. 43, 1632–1642 (2019).
Bayley, N. Bayley Scales of Infant Development. 2nd Edition. Psychological Corporation; 1993.
Mesa, D. A. et al. The use of cardiac orienting responses as an early and scalable biomarker of alcohol‐related neurodevelopmental impairment. Alcohol Clin. Exp. Res. 41, 128–138 (2017).
Lowe, J. R., Erickson, S. J., Schrader, R. & Duncan, A. F. Comparison of the Bayley II Mental Developmental Index and the Bayley III cognitive scale: are we measuring the same thing? Acta Pediatr. 101, e55–e58 (2012).
Nellis, L. & Gridley, B. E. Review of the Bayley scales of infant development—Second edition. J. Sch. Psychol. 32, 201–209 (1994).
Hollingshead, A. B. Four factor index of social status. J. Sociol. 8, 21–51 (2011).
Terasaki, L. S., Gomez, J. & Schwarz, J. M. An examination of sex differences in the effects of early-life opiate and alcohol exposure. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 371, 20150123 (2016).
May, P. A. et al. Who is most affected by prenatal alcohol exposure: Boys or girls? Drug Alcohol Depend. 177, 258–267 (2017).
Eickmann, S. H. et al. Breast feeding and mental and motor development at 12 months in a low-income population in northeast Brazil: breast feeding and mental development. Paediatr. Perinat. Epidemiol. 21, 129–137 (2007).
Guxens, M. et al. Breastfeeding, long-chain polyunsaturated fatty acids in colostrum, and infant mental development. Pediatrics 128, e880–e889 (2011).
Jardi, C. et al. Influence of breastfeeding and iron status on mental and psychomotor development during the first year of life. Infant Behav. Dev. 50, 300–310 (2018).
Thulier, D. & Mercer, J. Variables associated with breastfeeding duration. J. Obst. Gynecol. Neonatal Nurs. 38, 259–268 (2009).
Primo, C. C. et al. Which factors influence women in the decision to breastfeed. Invest. Educ. Enferm. 34, 198–210 (2016).
Ogbo, F. A. et al. Prevalence and determinants of cessation of exclusive breastfeeding in the early postnatal period in Sydney, Australia. Int. Breastfeed. J. 12, 16 (2017).
Martins, F. A. et al. Breastfeeding patterns and factors associated with early weaning in the Western Amazon. Rev. Saúde. Pública. 55, 21 (2021).
McCormack, C. et al. Prenatal alcohol consumption between conception and recognition of pregnancy. Alcohol Clin. Exp. Res. 41, 369–378 (2017).
Mårdby, A. C., Lupattelli, A., Hensing, G. & Nordeng, H. Consumption of alcohol during pregnancy—a multinational European study. Women Birth 30, e207–e213 (2017).
Romanenko, L., Shlemkevych, O. & Arendt, M. The current state of breastfeeding in Ukraine: an interview with Lidiia Romanenko and Olha Shlemkevych. J. Hum. Lact. 39, 15–21 (2023).
The United States Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Nutrition, Physical Activity, and Obesity. Breastfeeding report card: United States, 2022. Centers for Disease Control and Prevention. Updated August 31, Accessed August 16, 2023. https://www.cdc.gov/breastfeeding/data/reportcard.htm# 2022.
Acknowledgements
All or part of this work was done in conjunction with the CIFASD, which is funded by grants from the National Institute on Alcohol Abuse and Alcoholism. Additional information about CIFASD can be found at www.cifasd.org. We acknowledge the contribution of Omni-Net, Ukraine, and the participating families and staff in Rivne and Khmelnytskyi, Ukraine. These data were collected as part of the Collaborative Initiative on Fetal Alcohol Spectrum Disorders (CIFASD).
Funding
Supported by the National Institutes of Health (NIH) National Institute on Alcohol Abuse and Alcoholism (NIAAA) grant U01AA014835 and the NIH Office of Dietary Supplements (principal investigator: Dr Chambers). Gretchen Bandoli is funded by an NIH award (K01 AA027811).
Author information
Authors and Affiliations
Contributions
K.E.S. completed the data analysis and drafted the initial manuscript. G.B. conceptualized and designed the study and reviewed and revised the manuscript. C.C. conceptualized and designed the study, was responsible for the initial data collection, reviewed the manuscript for intellectual content, and reviewed and revised the manuscript. R.S.G. reviewed and revised the manuscript. W.W. was responsible for the initial data collection and reviewed the manuscript for intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
All study participants signed informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schaffer, K.E., Chambers, C.D., Garfein, R.S. et al. Breastfeeding and neurodevelopment in infants with prenatal alcohol exposure. Pediatr Res 95, 819–826 (2024). https://doi.org/10.1038/s41390-023-02848-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02848-z