Abstract
Background
Systemic inflammation plays a key role in the development of bronchopulmonary dysplasia (BPD). Cortisol is known to dampen inflammation. However, adrenal function following preterm birth is characterized by insufficient cortisol levels for the degree of inflammation, and a relative abundancy of cortisol precursors. We investigated whether this pattern could contribute to the development of BPD in preterm infants born <30 weeks of gestation.
Methods
Cortisol, cortisone, 17-OH progesterone (17-OHP) and 11-deoxycortisol were measured in serum obtained at postnatal days 1, 3, 7, 14 and 28, using liquid-chromatography-tandem-mass-spectrometry. The presence of BPD was ascertained at 36 weeks postmenstrual age.
Results
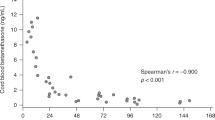
Sixty-five infants were included for analysis, of whom 32 (49%) developed BPD. Preterm infants developing BPD, as compared to those without BPD, had higher levels of 17-OHP, 11-deoxycortisol and cortisone relative to cortisol in their first week of life, but not at birth or beyond day 7.
Conclusion
Preterm infants developing BPD had higher levels of cortisol precursors and cortisone relative to cortisol in their first week of life than infants without BPD. These findings suggest that BPD is preceded by an activated hypothalamus-pituitary-adrenal axis that could not meet the high cortisol demands, which may predispose to inflammation and BPD.
Impact
-
Relative adrenal insufficiency is common in the first weeks after preterm birth, resulting in insufficient cortisol production for the degree of inflammation and a relative abundance of cortisol precursors;
-
Whether this pattern contributes to the development of bronchopulmonary dysplasia (BPD) is not fully elucidated, since most studies focused on cortisol levels;
-
Preterm infants developing BPD had higher levels of cortisol precursors and cortisone relative to cortisol in the first week of life, suggestive of a hypothalamus-pituitary-adrenal-axis activation during BPD development which cannot meet the high cortisol demands in tissues;
-
This glucocorticoid pattern is likely to dispose to inflammation and BPD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ambalavanan, N. et al. Cytokines associated with bronchopulmonary dysplasia or death in extremely low birth weight infants. Pediatrics 123, 1132–1141 (2009).
Finken, M. J. J. et al. Programming of the hypothalamus-pituitary-adrenal axis by very preterm birth. Ann. Nutr. Metab. 70, 170–174 (2017).
Kamrath, C., Hartmann, M. F., Boettcher, C. & Wudy, S. A. Reduced Activity of 11beta-Hydroxylase Accounts for Elevated 17alpha-Hydroxyprogesterone in Preterms. J. Pediatr. 165, 280–284 (2014).
Pijnenburg-Kleizen, K. J. et al. Adrenal Steroid Metabolites Accumulating in Congenital Adrenal Hyperplasia Lead to Transactivation of the Glucocorticoid Receptor. Endocrinology 156, 3504–3510 (2015).
Stewart, P. M., Murry, B. A. & Mason, J. I. Type 2 11 Beta-Hydroxysteroid Dehydrogenase in Human Fetal Tissues. J. Clin. Endocrinol. Metab. 78, 1529–1532 (1994).
Watterberg, K. L., Scott, S. M., Backstrom, C., Gifford, K. L. & Cook, K. L. Links between Early Adrenal Function and Respiratory Outcome in Preterm Infants: Airway Inflammation and Patent Ductus Arteriosus. Pediatrics 105, 320–324 (2000).
Renolleau, C. et al. Association between Baseline Cortisol Serum Concentrations and the Effect of Prophylactic Hydrocortisone in Extremely Preterm Infants. J. Pediatr. 234, 65–70 e63 (2021).
Watterberg, K. L. & Scott, S. M. Evidence of early Adrenal insufficiency in babies who develop bronchopulmonary dysplasia. Pediatrics 95, 120–125 (1995).
Watterberg, K. L. et al. Effect of Dose on Response to Adrenocorticotropin in extremely low birth weight infants. J. Clin. Endocrinol. Metab. 90, 6380–6385 (2005).
Watterberg, K. L., Gerdes, J. S. & Cook, K. L. Impaired Glucocorticoid synthesis in premature infants developing chronic lung disease. Pediatr. Res 50, 190–195 (2001).
Finken, M. J. et al. Glucocorticoid programming in very preterm birth. Horm. Res. Paediatr. 85, 221–231 (2016).
Doyle, L. W., Cheong, J. L., Ehrenkranz, R. A. & Halliday, H. L. Early (<8 Days) Systemic Postnatal Corticosteroids for Prevention of Bronchopulmonary Dysplasia in Preterm Infants. Cochrane Database Syst. Rev. 10, CD001146 (2017).
Doyle, L. W., Cheong, J. L., Hay, S., Manley, B. J. & Halliday, H. L. Early (≪7 Days) Systemic Postnatal Corticosteroids for Prevention of Bronchopulmonary Dysplasia in Preterm Infants. Cochrane Database Syst. Rev. 10, CD001146 (2021).
Singh, N. & Gautham, K. S. Pattern of Postnatal Steroid Use for Bronchopulmonary Dysplasia in Extremely Preterm Infants. J. Perinatol. 42, 1258–1259 (2022).
Yao, S. et al. Postnatal Corticosteroid Use for Prevention or Treatment of Bronchopulmonary Dysplasia in England and Wales 2012-2019: A Retrospective Population Cohort Study. BMJ Open 12, e063835 (2022).
Doyle, L. W., Halliday, H. L., Ehrenkranz, R. A., Davis, P. G. & Sinclair, J. C. An Update on the Impact of Postnatal Systemic Corticosteroids on Mortality and Cerebral Palsy in Preterm Infants: Effect Modification by Risk of Bronchopulmonary Dysplasia. J. Pediatr. 165, 1258–1260 (2014).
Onland, W. et al. Clinical Prediction Models for Bronchopulmonary Dysplasia: A Systematic Review and External Validation Study. BMC Pediatr. 13, 207 (2013).
Romijn, M. et al. Prediction Models for Bronchopulmonary Dysplasia in Preterm Infants: A Systematic Review and Meta-Analysis. J. Pediatr. 113370 (2023). https://doi.org/10.1016/j.jpeds.2023.01.024. Epub ahead of print.
Jobe, A. H. The New Bronchopulmonary Dysplasia. Curr. Opin. Pediatr. 23, 167–172 (2011).
Fanelli, F. et al. Report from the Harmoster Study: Impact of Calibration on Comparability of Lc-Ms/Ms Measurement of Circulating Cortisol, 17oh-Progesterone and Aldosterone. Clin. Chem. Lab Med 60, 726–739 (2022).
Aoki, M., Urakami, T., Nagano, N., Aoki, R. & Morioka, I. Association of Plasma Cortisol Levels with Gestational Age and Anthropometric Values at Birth in Preterm Infants. Int J. Environ. Res Public Health 19, 11448 (2022).
Stoll, B. J. et al. Neonatal Outcomes of Extremely Preterm Infants from the Nichd Neonatal Research Network. Pediatrics 126, 443–456 (2010).
Hoftiezer, L. et al. From Population Reference to National Standard: New and Improved Birthweight Charts. Am. J. Obstet. Gynecol. 220, 383 e381–383 e317 (2019).
Banks, B. A. et al. Association of Plasma Cortisol and Chronic Lung Disease in Preterm Infants. Pediatrics 107, 494–498 (2001).
Nykanen, P., Anttila, E., Heinonen, K., Hallman, M. & Voutilainen, R. Early Hypoadrenalism in Premature Infants at Risk for Bronchopulmonary Dysplasia or Death. Acta Paediatr. 96, 1600–1605 (2007).
Pau, D. A., Mackley, A. & Bartoshesky, L. Newborn Screening Levels of 17-Hydroxyprogesterone in Very Low Birth Weight Infants and the Relationship to Chronic Lung Disease. J. Pediatr. Endocrinol. Metab. 19, 1119–1124 (2006).
Merz, U., Pfaffle, R., Peschgens, T. & Hornchen, H. The Hypothalamic-Pituitary-Adrenal Axis in Preterm Infants Weighing < or = 1250 G: Association with Perinatal Data and Chronic Lung Disease. Acta Paediatr. 87, 313–317 (1998).
Bolt, R. J. et al. Maturity of the Adrenal Cortex in Very Preterm Infants Is Related to Gestational Age. Pediatr. Res 52, 405–410 (2002).
Engels, M. et al. Glucocorticoid Activity of Adrenal Steroid Precursors in Untreated Patients with Congenital Adrenal Hyperplasia. J Clin Endocrinol Metab 104, 5062–72 (2019).
Ng, P. C. et al. Transient Adrenocortical Insufficiency of Prematurity and Systemic Hypotension in Very Low Birthweight Infants. Arch. Dis. Child Fetal Neonatal Ed. 89, F119–F126 (2004).
Krasowski, M. D. et al. Cross-Reactivity of Steroid Hormone Immunoassays: Clinical Significance and Two-Dimensional Molecular Similarity Prediction. BMC Clin. Pathol. 14, 33 (2014).
Agrawal, N., Chakraborty, P. P., Sinha, A. & Maiti, A. False Elevation of Serum Cortisol in Chemiluminescence Immunoassay by Siemens Advia Centaur Xp System in 21-Hydroxylase Deficiency: An ‘Endocrine Laboma’. BMJ Case Rep. 13, e235450 (2020).
Haddad, R. A., Giacherio, D. & Barkan, A. L. Interpretation of Common Endocrine Laboratory Tests: Technical Pitfalls, Their Mechanisms and Practical Considerations. Clin. Diabetes Endocrinol. 5, 12 (2019).
Julious, S. A. Sample Sizes for Clinical Trials 317 (Chapman and Hall/CRC, 2010).
Chow, S,-C,, W. H., Shao, J,. Sample Size Calculations in Clinical Research 480 (Chapman and Hall/CRC, 2007).
Machin, D., C M. J., Tan, S. B., Tan, S. H. Sample Size Tables for Clinical Studies 2 edn(Wiley-Blackwell Science, 1997).
Zar, J. H. Biostatistical Analysis 2 edn(Practice-Hall, 1984).
Ng, P. C. et al. Early Pituitary-Adrenal Response and Respiratory Outcomes in Preterm Infants. Arch. Dis. Child Fetal Neonatal Ed. 89, F127–F130 (2004).
Funding
This study was supported by the Amsterdam Reproduction & Development Research Institute.
Author information
Authors and Affiliations
Contributions
M.R. made substantial contributions to conception and design, acquisition of data, data analysis and interpretation of data, drafted and revised the article, and approved the final version to be published. W.O. and M.J.J.F. made substantial contribution to conception and design, acquisition of data, data analysis and interpretation of data, revised the article critically, and approved the final version to be published. M.vanK. made substantial contribution to conception and design, acquisition of data, interpretation of data, revised the article critically and approved the final version to be published. A.C.H., J.R. and A.H.vanK. made substantial contributions to interpretation of the data, revised the manuscript critically for important intellectual content and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Written informed consent for participation and publication of the study results was obtained from all parents.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Romijn, M., Onland, W., van Keulen, B.J. et al. Glucocorticoid signature of preterm infants developing bronchopulmonary dysplasia. Pediatr Res 94, 1804–1809 (2023). https://doi.org/10.1038/s41390-023-02690-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02690-3