Abstract
Background
A current area of research interest is the association between ADHD and weight status. This paper aimed to describe the anthropometric status of school children with ADHD, considering age and clinical presentation (inattentive, hyperactive-impulsive, or combined), compared with control children.
Methods
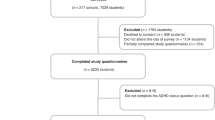
Participants came from the “Epidemiological Research Project on Neurodevelopmental Disorders” and consisted of 198 preschoolers (41 with ADHD) and 389 elementary school children (163 with ADHD). ADHD was diagnosed using DSM-5 criteria. Anthropometric measurements were taken at various anatomical points, and height, weight, and body composition were also measured.
Results
In preschoolers, an association was found between hyperactive-impulsive ADHD and greater height and lower waist-to-height ratio. In elementary school children, regardless of the medication, combined ADHD was associated with smaller head, hip, arm, and thigh circumferences and lower weight, height, and BMI. A total of 19.7% of them were underweight. In contrast, children with inattentive and hyperactive/impulsive presentations presented the highest percentage of overweight/obesity (56%).
Conclusion
The anthropometric status of the school children with ADHD showed differences in terms of age and presentation. Preschoolers with hyperactive-impulsive ADHD are taller, and elementary school children with combined ADHD are shorter and smaller than their age-matched control peers.
Impact
-
The anthropometric status of the school children with ADHD showed differences in terms of age and presentation.
-
Preschoolers with hyperactive-impulsive ADHD are taller than their control peers.
-
Elementary school children with combined ADHD, regardless of the pharmacological treatment, are shorter and smaller than their control peers.
-
Medication may anthropometrically affect the height of children with inattentive presentation.
-
Anthropometric and dietary monitoring should be recommended to parents of children with ADHD, with and without medication.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (American Psychiatric Association). https://doi.org/10.1176/appi.books.9780890425596.744053 (2013).
Canals Sans, J., Morales Hidalgo, P., Roigé Castellví, J., Voltas Moreso, N. & Hernández Martínez, C. Prevalence and epidemiological characteristics of ADHD in pre-school and school age children in the province of Tarragona, Spain. J. Atten. Disord. 25, 1818–1833 (2021).
Sayal, K., Prasad, V., Daley, D., Ford, T. & Coghill, D. ADHD in children and young people: prevalence, care pathways, and service provision. Lancet Psychiatry 5, 175–186 (2018).
Pinhas-Hamiel, O. et al. Attention-deficit/hyperactivity disorder and obesity: a national study of 1.1 million Israeli adolescents. J. Clin. Endocrinol. Metab. 107, e1434–e1443 (2022).
Jongpitakrat, K. & Limsuwan, N. Prevalences of overweight and obesity in children and adolescents: the comparison of ADHD and other clinical samples. J. Atten. Disord. 26, 1464–1470. https://doi.org/10.1177/10870547221081106 (2022).
Childress, A. C. et al. Long-term treatment with extended-release methylphenidate treatment in children aged 4 to <6. J. Am. Acad. Child Adolesc. Psychiatry 61, 80–92 (2022).
Racicka, E., Hanć, T., Giertuga, K., Bryńska, A. & Wolańczyk, T. Prevalence of overweight and obesity in children and adolescents With ADHD: the significance of comorbidities and pharmacotherapy. J. Atten. Disord. 22, 1095–1108 (2018).
Goulardins, J. B. et al. The relationship between motor skills, ADHD symptoms, and childhood body weight. Res Dev. Disabil. 55, 279–286 (2016).
Ptacek, R., Kuzelova, H., Paclt, I., Zukov, I. & Fischer, S. Anthropometric changes in non-medicated ADHD boys. Neuroendocrinol. Lett. 30, 377–381 (2009).
Hanć, T. et al. Attention-deficit/hyperactivity disorder is related to decreased weight in the preschool period and to increased rate of overweight in school-age boys. J. Child Adolesc. Psychopharmacol. 25, 691–700 (2015).
Faraone, S. V., Lecendreux, M. & Konofal, E. Growth dysregulation and ADHD: an epidemiologic study of children in France. J. Atten. Disord. 16, 572–578 (2012).
Biederman, J., Mick, E. & Faraone, S. V. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: impact of remission definition and symptom type. Am. J. Psychiatry 157, 816–818 (2000).
Turan, S., Tunctürk, M., Çıray, R. O., Halaç, E. & Ermiş, Ç. ADHD and risk of childhood adiposity: a review of recent research. Curr. Nutr. Rep. 10, 30–46 (2021).
el Archi, S. et al. Negative affectivity and emotion dysregulation as mediators between ADHD and disordered eating: a systematic review. Nutrients 12, 1–34 (2020).
Dmitrzak-Weglarz, M. et al. Common and unique genetic background between attention-deficit/hyperactivity disorder and excessive body weight. Genes (Basel) 12, 1407 (2021).
Carucci, S. et al. Long term methylphenidate exposure and growth in children and adolescents with ADHD. A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 120, 509–525 (2021).
Schwartz, B. S. et al. Attention deficit disorder, stimulant use, and childhood body mass index trajectory. Pediatrics 133, 668–676 (2014).
Yackobovitch-Gavan, M. et al. Sex-specific long-term height and body mass index trajectories of children diagnosed with attention-deficit/hyperactivity disorder and treated with stimulants. J. Pediatr. 238, 296–304.e4 (2021).
Granato, M. F., Ferraro, A. A., Lellis, D. M. & Casella, E. B. Associations between attention-deficit hyperactivity disorder (ADHD) treatment and patient nutritional status and height. Behav. Neurol. 2018, 1–7 (2018).
Harstad, E. B. et al. ADHD, stimulant treatment, and growth: a longitudinal study. Pediatrics 134, e935–e944 (2014).
Biederman, J. et al. Growth deficits and attention-deficit/hyperactivity disorder revisited: impact of gender, development, and treatment. Pediatrics 111, 1010–1016 (2003).
Cerrillo-Urbina, A. J. et al. The effects of physical exercise in children with attention deficit hyperactivity disorder: a systematic review and meta-analysis of randomized control trials. Child Care Health Dev. 41, 779–788 (2015).
Villa-González, R., Villalba-Heredia, L., Crespo, I., del Valle, M. & Olmedillas, H. A systematic review of acute exercise as a coadjuvant treatment of ADHD in young people. Psicothema 32, 67–74 (2020).
Rusek, W. et al. Changes in children’s body composition and posture during puberty growth. Children (Basel) 8, 288 (2021).
Rojo-Marticella, M. et al. Do children with attention-deficit/hyperactivity disorder follow a different dietary pattern than that of their control peers? Nutrients 14, 1131 (2022).
Zhang, S., Huang, Y., Zaid, M. & Tong, L. ADHD symptoms and obesity in chinese children and adolescents: a longitudinal study with abnormal eating behaviors as moderating factors. J. Atten. Disord. 26, 1452–1463 (2022).
Gair, S. L., Brown, H. R., Kang, S., Grabell, A. S. & Harvey, E. A. Early development of comorbidity between symptoms of ADHD and anxiety. Res. Child Adolesc. Psychopathol. 49, 311–323 (2021).
Pervanidou, P. et al. Internalizing and externalizing problems in obese children and adolescents: associations with daily salivary cortisol concentrations. Hormones (Athens) 14, 623–631 (2015).
Morales-Hidalgo, P., Voltas-Moreso, N., Hernández-Martínez, C. & Canals-Sans, J. Emotional problems in preschool and school-aged children with neurodevelopmental disorders in Spain: EPINED epidemiological project. Res. Dev. Disabil. 135, 104454 (2023).
Esteban-Figuerola, P., Morales-Hidalgo, P., Arija-Val, V. & Canals-Sans, J. Are there anthropometric and body composition differences between children with autism spectrum disorder and children with typical development? Analysis by age and spectrum severity in a school population. Autism 25, 1307–1320 (2021).
Yuan, Y. et al. Prevalence of overweight and obesity in children and adolescents with intellectual disabilities in China. J. Intellect. Disabil. Res. 65, 655–665 (2021).
Yang, R., Mao, S., Zhang, S., Li, R. & Zhao, Z. Prevalence of obesity and overweight among Chinese children with attention deficit hyperactivity disorder: a survey in Zhejiang Province, China. BMC Psychiatry 13, 133 (2013).
Zerón-Rugerio, M. F. et al. ADHD subtypes are associated differently with circadian rhythms of motor activity, sleep disturbances, and body mass index in children and adolescents: a case–control study. Eur. Child Adolesc. Psychiatry 30, 1917–1927 (2021).
Mayes, S. D. et al. ADHD subtypes and comorbid anxiety, depression, and oppositional-defiant disorder: differences in sleep problems. J. Pediatr. Psychol. 34, 328–337 (2009).
Garaulet, M. et al. Fragmentation of daily rhythms associates with obesity and cardiorespiratory fitness in adolescents: The HELENA study. Clin. Nutr. 36, 1558–1566 (2017).
Kaufman, J. et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 36, 980–988 (1997).
Achenbach, T. M., & Rescorla, L. A. Child Behavior Checklist for Ages 6-18. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. (2001).
Achenbach, T. M. Manual for the Youth Self-Report and 1991 Profile (Department of Psychiatry, University of Vermont, 1991).
Cashin, K. & Oot, L. Guide to Anthropometry: A Practical Tool for Program Planners, Managers, and Implementers. Food and Nutrition Technical Assistance III Project (FANTA)/ FHI 360 https://www.fantaproject.org/sites/default/files/resources/FANTA-Anthropometry-Guide-May2018.pdf (2018).
de Onis, M. et al. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ 85, 660–667 (2007).
Casadei, K. & Kiel, J. Anthropometric Measurement. StatPearls https://www.ncbi.nlm.nih.gov/books/NBK537315/ (2021).
Bowling, A. B., Tiemeier, H. W., Jaddoe, V. W. V., Barker, E. D. & Jansen, P. W. ADHD symptoms and body composition changes in childhood: a longitudinal study evaluating directionality of associations. Pediatr. Obes. 13, 567–575 (2018).
Kesztyüs, D., Lampl, J. & Kesztyüs, T. The weight problem: overview of the most common concepts for body mass and fat distribution and critical consideration of their usefulness for risk assessment and practice. Int. J. Environ. Res. Public Health 18, 11070 (2021).
Macek, P. et al. Optimal body fat percentage cut-off values in predicting the obesity-related cardiovascular risk factors: a cross-sectional cohort study. Diabetes Metab. Syndr. Obes. 13, 1587 (2020).
Wang, Y. & Chen, H. Use of percentiles and scores in anthropometry. In: Preedy, V. R. Editor. Handbook of Anthropometry: Physical Measures of Human Form in Health and Disease. 29–48 (Springer, New York, NY). https://doi.org/10.1007/978-1-4419-1788-1_2 (2012).
Norte-Navarro, A. & Ortiz-Moncada, R. Calidad de la dieta española según el índice de alimentación saludable. Nutr. Hosp. 26, 330–336 (2011).
Hollingshead, A. B. Four factor index of social status. Yale J. Sociol. 8, 21–52 (1975).
Hanć, T. & Cortese, S. Attention deficit/hyperactivity-disorder and obesity: a review and model of current hypotheses explaining their comorbidity. Neurosci. Biobehav. Rev. 92, 16–28 (2018).
Seymour, K. E., Reinblatt, S. P., Benson, L. & Carnell, S. Overlapping neurobehavioral circuits in ADHD, obesity, and binge eating: evidence from Neuroimaging Research. CNS Spectr. 20, 401 (2015).
García Solano, M. et al. Weight status in the 6- to 9-year-old school population in Spain: results of the ALADINO 2019 Study. Nutr. Hosp. 38, 943–953 (2021).
Swanson, J. et al. Stimulant-related reductions of growth rates in the PATS. J. Am. Acad. Child Adolesc. Psychiatry 45, 1304–1313 (2006).
Canals, J., Morales-Hidalgo, P., Jané, M. C. & Domènech, E. ADHD prevalence in Spanish preschoolers: comorbidity, socio-demographic factors, and functional consequences. J. Atten. Disord. 22, 143–153 (2018).
Deng, L. et al. Methylphenidate and atomoxetine treatment negatively affect physical growth indexes of school-age children and adolescents with attention-deficit/hyperactivity disorder. Pharm. Biochem Behav. 208, 173225 (2021).
Biederman, J., Spencer, T. J., Monuteaux, M. C. & Faraone, S. V. A naturalistic 10-year prospective study of height and weight in children with attention-deficit hyperactivity disorder grown up: sex and treatment effects. J. Pediatr. 157, 635–640.e1 (2010).
Hanć, T. & Cieślik, J. Growth in stimulant-naive children with attention-deficit/hyperactivity disorder using cross-sectional and longitudinal approaches. Pediatrics 121, e967–e974 (2008).
Aparicio, E., Canals, J., Voltas, N., Valenzano, A. & Arija, V. Emotional symptoms and dietary patterns in early adolescence: a school-based follow-up study. J. Nutr. Educ. Behav. 49, 405–414.e1 (2017).
Kaisari, P., Dourish, C. T., Rotshtein, P. & Higgs, S. Associations between core symptoms of attention deficit hyperactivity disorder and both binge and restrictive eating. Front. Psychiatry 9, 103 (2018).
Aparicio, E., Canals, J., Arija, V., De Henauw, S. & Michels, N. The role of emotion regulation in childhood obesity: implications for prevention and treatment. Nutr. Res. Rev. 29, 17–29 (2016).
Sares-Jäske, L., Grönqvist, A., Mäki, P., Tolonen, H. & Laatikainen, T. Family socioeconomic status and childhood adiposity in Europe – a scoping review. Prev. Med. 160, 107095 (2022).
Nemet, D., Ben-Zaken, S., Eliakim, R. A. & Eliakim, A. Reduced exercise-induced growth hormone secretion among children with attention-deficit hyperactivity disorder. Growth Horm. IGF Res. 65, 101485 (2022).
Sung, V., Hiscock, H., Sciberras, E. & Efron, D. Sleep problems in children with attention-deficit/hyperactivity disorder: prevalence and the effect on the child and family. Arch. Pediatr. Adolesc. Med. 162, 336–342 (2008).
Shen, L.-X. et al. Nutritional complexity in children with ADHD related morbidities in China: a cross-sectional study. Asia Pac. J. Clin. Nutr. 31, 108–117 (2022).
Mayes, S. D., Puzino, K., DiGiovanni, C. & Calhoun, S. L. Cross-sectional age analysis of sleep problems in 2 to 17 year olds with ADHD combined, ADHD inattentive, or autism. J. Clin. Psychol. Med. Settings 29, 239–248. https://doi.org/10.1007/S10880-021-09799-9/FIGURES/1 (2022).
Ironside, S., Davidson, F. & Corkum, P. Circadian motor activity affected by stimulant medication in children with attention-deficit/hyperactivity disorder. J. Sleep. Res. 19, 546–551 (2010).
Kim, E. et al. Relationship among attention-deficit hyperactivity disorder, dietary behaviours and obesity. Child Care Health Dev. 40, 698–705 (2014).
Acknowledgements
We thank the Universitat Rovira i Virgili’s Martí Franqués Grant 2020PMF-PIPF-36 and our colleagues Lucía Iglesias-Vázquez and Andrés Díaz-López for their invaluable help. The authors are grateful to the URV English Service for reviewing the manuscript.
Funding
This work was supported by the Ministry of Economy and Competitiveness of Spain and the European Regional Development Fund (ERDF) under Grant PSI2015–64837-P and RTI2018–097124-B-I00.
Author information
Authors and Affiliations
Contributions
Conceptualization: J.C.-S. and V.A.; methodology: J.C.-S. and V.A.; formal analysis: M.R.-M. and V.A.; investigation: P.M.-H., P.E.-F., N.V.-M., and J.C.-S.; data curation: M.R.-M., P.M.-H., N.V.-M., P.E.-F., and J.C.-S.; writing—original draft preparation: M.R.-M., V.A., and J.C.-S.; writing—review and editing: M.R.-M., V.A., P.M.-H, N.V.-M., and J.C.-S.; funding acquisition: J.C.-S. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
Informed consent was obtained from all individual participants included in this study.
Consent for publication
Consent for publication was provided by all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rojo-Marticella, M., Arija, V., Morales-Hidalgo, P. et al. Anthropometric status of preschoolers and elementary school children with ADHD: preliminary results from the EPINED study. Pediatr Res 94, 1570–1578 (2023). https://doi.org/10.1038/s41390-023-02671-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02671-6