Abstract
Background
We investigated the temporal evolution of post-hemorrhagic ventricular dilatation (PHVD) and compared neurodevelopmental impairments (NDI) in newborns with (Group 1) spontaneous resolution of PHVD, (Group 2) persistent PHVD without neurosurgical intervention, and (Group 3) progressive PHVD receiving neurosurgical intervention.
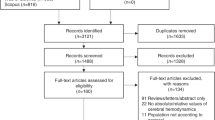
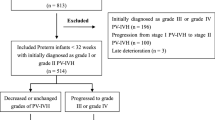
Methods
A multicenter retrospective cohort study of newborns born at ≤34 weeks with PHVD (ventricular index [VI] >97th centile for gestational age and anterior horn width [AHW] >6 mm) from 2012 to 2020. Severe NDI was defined as global developmental delay or cerebral palsy GMFCS III–V at 18 months.
Results
Of 88 survivors with PHVD, 39% had a spontaneous resolution, 17% had persistent PHVD without intervention, and 44% had progressive PHVD receiving intervention. The median time between PHVD diagnosis and spontaneous resolution was 14.0 days (IQR 6.8–32.3) and between PHVD diagnosis and first neurosurgical intervention was 12.0 days (IQR 7.0–22.0). Group 1 had smaller median maximal VI (1.8, 3.4, 11.1 mm above p97; p < 0.001) and AHW (7.2, 10.8, 20.3 mm; p < 0.001) than Groups 2 and 3. Neurodevelopmental outcome data were available for 82% of survivors. Group 1 had reduced severe NDI compared to Group 3 (15% vs 66%; p < 0.001).
Conclusion
Newborns with PHVD without spontaneous resolution are at higher risk for impairments despite neurosurgical interventions, which may be due to larger ventricular dilatation.
Impact
-
The natural evolution of post-hemorrhagic ventricular dilatation (PHVD) and developmental implications of spontaneous resolution are not well established.
-
In this study, approximately one in three newborns with PHVD experienced spontaneous resolution and this subset of newborns had reduced rates of neurodevelopmental impairments.
-
More prominent ventricular dilatation was associated with reduced rates of spontaneous resolution and increased rates of severe neurodevelopmental impairment among newborns with PHVD.
-
Understanding clinically relevant time points in the evolution of PHVD and predictors of spontaneous resolution may help inform the discussion around the optimal timing for intervention and allow for more precise prognostication in this population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
El-Dib, M. et al. Management of post-hemorrhagic ventricular dilatation in the infant born preterm. J. Pediatr. 226, 16–27.e13 (2020).
de Vries, L. S. et al. Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: a randomised controlled trial. Arch. Dis. Child Fetal Neonatal Ed. 104, F70–f75 (2019).
Volpe, J. J. et al. Volpe’s Neurology of the Newborn E-Book 637–398 (Elsevier Health Sciences, 2017).
Cizmeci, M. N. et al. Randomized controlled Early versus Late Ventricular Intervention Study in posthemorrhagic ventricular dilatation: outcome at 2 years. J. Pediatr. 226, 28–35.e3 (2020).
Shankaran, S. et al. Outcomes following post-hemorrhagic ventricular dilatation among infants of extremely low gestational age. J. Pediatr. 226, 36–44.e3 (2020).
Bock, H. C., Feldmann, J. & Ludwig, H. C. Early surgical management and long-term surgical outcome for intraventricular hemorrhage-related posthemorrhagic hydrocephalus in shunt-treated premature infants. J. Neurosurg. Pediatr. 22, 61–67 (2018).
Mazzola, C. A. et al. Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 2: management of posthemorrhagic hydrocephalus in premature infants. J. Neurosurg. Pediatr. 14(Suppl 1), 8–23 (2014).
Shah, P. S. et al. Internal audit of the canadian neonatal network data collection system. Am. J. Perinatol. 34, 1241–1249 (2017).
Volpe, J. J. Intraventricular hemorrhage in the premature infant–current concepts. Part II. Ann. Neurol. 25, 109–116 (1989).
Benavente-Fernandez, I., Lubián-Gutierrez, M., Jimenez-Gomez, G., Lechuga-Sancho, A. M. & Lubián-López, S. P. Ultrasound lineal measurements predict ventricular volume in posthaemorrhagic ventricular dilatation in preterm infants. Acta Paediatr. 106, 211–217 (2017).
Leijser, L. M. & de Vries, L. S. Preterm brain injury: germinal matrix-intraventricular hemorrhage and post-hemorrhagic ventricular dilatation. Handb. Clin. Neurol. 162, 173–199 (2019).
de Vries, L. S., Eken, P. & Dubowitz, L. M. The spectrum of leukomalacia using cranial ultrasound. Behav. Brain Res. 49, 1–6 (1992).
Bélanger, S. A. & Caron, J. Evaluation of the child with global developmental delay and intellectual disability. Paediatr. Child Health 23, 403–419 (2018).
Leijser, L. M. et al. Posthemorrhagic ventricular dilatation in preterm infants: when best to intervene? Neurology 90, e698–e706 (2018).
Cohen, S. et al. Survey of quaternary neonatal management of posthemorrhagic hydrocephalus. Am. J. Perinatol. https://doi.org/10.1055/s-0041-1732417 (2021).
de Vries, L. S. et al. Early versus late treatment of posthaemorrhagic ventricular dilatation: results of a retrospective study from five neonatal intensive care units in the Netherlands. Acta Paediatr. 91, 212–217 (2002).
Bassan, H. et al. Timing of external ventricular drainage and neurodevelopmental outcome in preterm infants with posthemorrhagic hydrocephalus. Eur. J. Paediatr. Neurol. 16, 662–670 (2012).
Cizmeci, M. N., Groenendaal, F. & de Vries, L. S. Timing of intervention for posthemorrhagic ventricular dilatation: an ongoing debate. J. Pediatr. 234, 14–16 (2021).
Whittemore, B.A., Swift, D.M., Thomas, J.M. & Chalak, L. F. A neonatal neuronicu collaborative approach to neuromonitoring of posthemorrhagic ventricular dilation in preterm infants. Pediatr. Res. 91, 27–34 (2022).
Isaacs, A. M. et al. MR diffusion changes in the perimeter of the lateral ventricles demonstrate periventricular injury in post-hemorrhagic hydrocephalus of prematurity. Neuroimage Clin. 24, 102031 (2019).
Limbrick, D. D. Jr. et al. Cerebrospinal fluid biomarkers of pediatric hydrocephalus. Pediatr. Neurosurg. 52, 426–435 (2017).
Lai, G. Y. et al. Ventriculomegaly thresholds for prediction of symptomatic post-hemorrhagic ventricular dilatation in preterm infants. Pediatr. Res. 92, 1621–1629 (2022).
Leijser, L. M. et al. Post-hemorrhagic ventricular dilatation: inter-observer reliability of ventricular size measurements in extremely preterm infants. Pediatr. Res. 90, 403–410 (2021).
Han, R. H. et al. Time-to-event analysis of surgically treated posthemorrhagic hydrocephalus in preterm infants: a single-institution retrospective study. Childs Nerv. Syst. 33, 1917–1926 (2017).
Murphy, B. P. et al. Posthaemorrhagic ventricular dilatation in the premature infant: natural history and predictors of outcome. Arch. Dis. Child Fetal Neonatal Ed. 87, F37–F41 (2002).
Partridge, J. C., Babcock, D. S., Steichen, J. J. & Han, B. K. Optimal timing for diagnostic cranial ultrasound in low-birth-weight infants: detection of intracranial hemorrhage and ventricular dilation. J. Pediatr. 102, 281–287 (1983).
Korobkin, R. The relationship between head circumference and the development of communicating hydrocephalus in infants following intraventricular hemmorrhage. Pediatrics 56, 74–77 (1975).
Srinivasakumar, P. et al. Posthemorrhagic ventricular dilatation-impact on early neurodevelopmental outcome. Am. J. Perinatol. 30, 207–214 (2013).
Lai, G. Y. et al. Degree of ventriculomegaly predicts school-aged functional outcomes in preterm infants with intraventricular hemorrhage. Pediatr. Res. 91, 1238–1247 (2022).
Ballabh, P. & de Vries, L. S. White matter injury in infants with intraventricular haemorrhage: mechanisms and therapies. Nat. Rev. Neurol. 17, 199–214 (2021).
Karas, C. S., Baig, M. N. & Elton, S. W. Ventriculosubgaleal shunts at columbus children’s hospital: neurosurgical implant placement in the neonatal intensive care unit. J. Neurosurg. 107, 220–223 (2007).
Acknowledgements
The authors would like to thank Mme Mylène Leblanc, RN, for assisting in the data collection.
Author information
Authors and Affiliations
Contributions
Each author has met the Pediatric Research authorship requirements. Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: E.G.-B., M.P., M.K., M.B., R.D., M.G., J.G. Drafting the article or revising it critically for important intellectual content: E.G.-B., M.P., M.K., M.B., R.D., A.F., M.G., V.B., J.G. Final approval of the version to be published: E.G.-B., M.P., M.K., M.B., R.D., A.F., M.G., V.B., J.G.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Groulx-Boivin, E., Paquette, M., Khairy, M. et al. Spontaneous resolution of post-hemorrhagic ventricular dilatation in preterm newborns and neurodevelopment. Pediatr Res 94, 1428–1435 (2023). https://doi.org/10.1038/s41390-023-02647-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02647-6