Abstract
Background
Illness severity scores predict mortality following pediatric critical illness. Given declining PICU mortality, we assessed the ability of the Pediatric Risk of Mortality-III (PRISM) and Pediatric Logistic Organ Dysfunction-2 (PELOD) scores to predict morbidity outcomes.
Methods
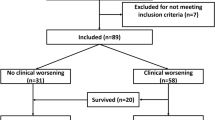
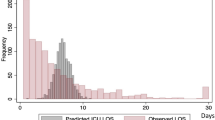
Among 359 survivors <18 years in the Life After Pediatric Sepsis Evaluation multicenter prospective cohort study, we assessed functional morbidity at hospital discharge (Functional Status Scale increase ≥3 points from baseline) and health-related quality of life (HRQL; Pediatric Quality of Life Inventory or Functional Status II-R) deterioration >25% from baseline at 1, 3, 6, and 12 months post-admission. We determined discrimination of admission PRISM and admission, maximum, and cumulative 28-day PELOD with functional and HRQL morbidity at each timepoint.
Results
Cumulative PELOD provided the best discrimination of discharge functional morbidity (area under the receive operating characteristics curve [AUROC] 0.81, 95% CI 0.76–0.87) and 3-month HRQL deterioration (AUROC 0.71, 95% CI 0.61–0.81). Prediction was inferior for admission PRISM and PELOD and for 6- and 12-month HRQL assessments.
Conclusions
Illness severity scores have a good prediction of early functional morbidity but a more limited ability to predict longer-term HRQL. Identification of factors beyond illness severity that contribute to HRQL outcomes may offer opportunities for intervention to improve outcomes.
Impact
-
Illness severity scores are commonly used for mortality prediction and risk stratification in pediatric critical care research, quality improvement, and resource allocation algorithms.
-
Prediction of morbidity rather than mortality may be beneficial given declining pediatric intensive care unit mortality.
-
The PRISM and PELOD scores have moderate to good ability to predict new functional morbidity at hospital discharge following pediatric septic shock but limited ability to predict health-related quality of life outcomes in the year following PICU admission.
-
Further research is needed to identify additional factors beyond illness severity that may impact post-discharge health-related quality of life.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The LAPSE dataset is available at the Eunice Kennedy Shriver NICHD Data and Specimen Hub (DASH): https://dash.nichd.nih.gov/explore/study?q=LAPSE&filters=[]&page=1&sortBy=relevance&asc=true&size=50.
References
Lee, J., Dubin, J. A. & Maslove, D. M. in Secondary Analysis of Electronic Health Records Ch. 21, 315–324 (Springer, 2016).
Pollack, M. M., Patel, K. M. & Ruttimann, U. E. PRISM III: an updated Pediatric Risk of Mortality score. Crit. Care Med. 24, 743–752 (1996).
Leteurtre, S. et al. PELOD-2: an update of the Pediatric Logistic Organ Dysfunction score. Crit. Care Med. 41, 1761–1773 (2013).
Barbaro, R. P. et al. Evaluating mortality risk adjustment among children receiving extracorporeal support for respiratory failure. ASAIO J. 65, 277–284 (2019).
Goncalves, J. P. et al. Performance of PRISM III and PELOD-2 scores in a pediatric intensive care unit. Eur. J. Pediatr. 174, 1305–1310 (2015).
Hamshary, A., Sherbini, S. A. E., Elgebaly, H. F. & Amin, S. A. Prevalence of multiple organ dysfunction in the pediatric intensive care unit: Pediatric Risk of Mortality III versus Pediatric Logistic Organ Dysfunction scores for mortality prediction. Rev. Bras. Ter. Intensiv. 29, 206–212 (2017).
Lalitha, A. V. et al. Sequential organ failure assessment score as a predictor of outcome in sepsis in pediatric intensive care unit. J. Pediatr. Intensive Care 10, 110–117 (2021).
Niederwanger, C. et al. Comparison of pediatric scoring systems for mortality in septic patients and the impact of missing information on their predictive power: a retrospective analysis. PeerJ 8, e9993 (2020).
Shen, Y. & Jiang, J. Meta-analysis for the prediction of mortality rates in a pediatric intensive care unit using different scores: PRISM-III/IV, PIM-3, and PELOD-2. Front. Pediatr. 9, 712276 (2021).
Zhang, L. et al. Performance of PRISM III, PELOD-2, and P-MODS scores in two pediatric intensive care units in China. Front. Pediatr. 9, 626165 (2021).
Zhang, Z. et al. Performance of three mortality prediction scores and evaluation of important determinants in eight pediatric intensive care units in China. Front. Pediatr. 8, 522 (2020).
Burns, J. P., Sellers, D. E., Meyer, E. C., Lewis-Newby, M. & Truog, R. D. Epidemiology of death in the PICU at five U.S. teaching hospitals. Crit. Care Med. 42, 2101–2108 (2014).
Namachivayam, P. et al. Three decades of pediatric intensive care: who was admitted, what happened in intensive care, and what happened afterward. Pediatr. Crit. Care Med. 11, 549–555 (2010).
Maddux, A. B. et al. Postdischarge outcome domains in pediatric critical care and the instruments used to evaluate them: a scoping review. Crit. Care Med. 48, e1313–e1321 (2020).
Manning, J. C., Pinto, N. P., Rennick, J. E., Colville, G. & Curley, M. A. Q. Conceptualizing post intensive care syndrome in children-the PICS-P Framework. Pediatr. Crit. Care Med. 19, 298–300 (2018).
Pollack, M. M. et al. Simultaneous prediction of new morbidity, mortality, and survival without new morbidity from pediatric intensive care: a new paradigm for outcomes assessment. Crit. Care Med. 43, 1699–1709 (2015).
Zimmerman, J. J. et al. Trajectory of mortality and health-related quality of life morbidity following community-acquired pediatric septic shock. Crit. Care Med. 48, 329–337 (2020).
Goldstein, B., Giroir, B. & Randolph, A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr. Crit. Care Med. 6, 2–8 (2005).
Pollack, M. M. et al. The ideal time interval for critical care severity-of-illness assessment. Pediatr. Crit. Care Med. 14, 448–453 (2013).
Leclerc, F. et al. Cumulative influence of organ dysfunctions and septic state on mortality of critically ill children. Am. J. Respir. Crit. Care Med. 171, 348–353 (2005).
Pollack, M. M. et al. Functional Status Scale: new pediatric outcome measure. Pediatrics 124, e18–e28 (2009).
Pollack, M. M. et al. Pediatric intensive care outcomes: development of new morbidities during pediatric critical care. Pediatr. Crit. Care Med. 15, 821–827 (2014).
Varni, J. W., Burwinkle, T. M., Seid, M. & Skarr, D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul. Pediatr. 3, 329–341 (2003).
Varni, J. W. et al. The PedsQL infant scales: feasibility, internal consistency reliability, and validity in healthy and ill infants. Qual. Life Res. 20, 45–55 (2011).
Stein, R. E. & Jessop, D. J. Functional Status II(R). a measure of child health status. Med. Care 28, 1041–1055 (1990).
Killien, E. Y. et al. Health-related quality of life outcome measures for children surviving critical care: a scoping review. Qual. Life Res. 30, 3383–3394 (2021).
Kruse, S., Schneeberg, A. & Brussoni, M. Construct validity and impact of mode of administration of the PedsQL among a pediatric injury population. Health Qual. Life Outcomes 12, 168 (2014).
Rabbitts, J. A., Palermo, T. M., Zhou, C. & Mangione-Smith, R. Pain and health-related quality of life after pediatric inpatient surgery. J. Pain. 16, 1334–1341 (2015).
Rivara, F. P. et al. Persistence of disability 24 to 36 months after pediatric traumatic brain injury: a cohort study. J. Neurotrauma 29, 2499–2504 (2012).
Heneghan, J. A. et al. Outcome measures following critical illness in children with disabilities: a scoping review. Front. Pediatr. 9, 689485 (2021).
Killien, E. Y., Farris, R. W. D., Watson, R. S., Dervan, L. A. & Zimmerman, J. J. Health-related quality of life among survivors of pediatric sepsis. Pediatr. Crit. Care Med. 20, 501–509 (2019).
Dervan, L. A., Killien, E. Y., Smith, M. B. & Watson, R. S. Health-related quality of life following delirium in the PICU. Pediatr. Crit. Care Med. 23, 118–128 (2022).
Zimmerman, J. J. et al. Critical illness factors associated with long-term mortality and health-related quality of life morbidity following community-acquired pediatric septic shock. Crit. Care Med. 48, 319–328 (2020).
Lemeshow, S. & Hosmer, D. W. Jr. A review of goodness of fit statistics for use in the development of logistic regression models. Am. J. Epidemiol. 115, 92–106 (1982).
Matics, T. J., Pinto, N. P. & Sanchez-Pinto, L. N. Association of organ dysfunction scores and functional outcomes following pediatric critical illness. Pediatr. Crit. Care Med. 20, 722–727 (2019).
Ong, C., Lee, J. H., Leow, M. K. & Puthucheary, Z. A. Functional outcomes and physical impairments in pediatric critical care survivors: a scoping review. Pediatr. Crit. Care Med. 17, e247–e259 (2016).
Bone, M. F., Feinglass, J. M. & Goodman, D. M. Risk factors for acquiring functional and cognitive disabilities during admission to a PICU. Pediatr. Crit. Care Med. 15, 640–648 (2014).
Sankar, J. et al. Functional outcomes at 1 year after picu discharge in critically ill children with severe sepsis. Pediatr. Crit. Care Med. 22, 40–49 (2021).
Ravikumar, N., Sankar, J. & Das, R. R. Functional outcomes in survivors of pediatric sepsis: a scoping review and discussion of implications for low- and middle-income countries. Front. Pediatr. 10, 762179 (2022).
Polic, B. et al. Long-term quality of life of patients treated in paediatric intensive care unit. Eur. J. Pediatr. 172, 85–90 (2013).
Ebrahim, S. et al. Adaptive behavior, functional outcomes, and quality of life outcomes of children requiring urgent ICU admission. Pediatr. Crit. Care Med. 14, 10–18 (2013).
Jones, S. et al. Outcome at 6 months after admission for pediatric intensive care: a report of a National Study of Pediatric Intensive Care Units in the United Kingdom. Pediatrics 118, 2101–2108 (2006).
Hordijk, J. et al. Health-related quality of life of children and their parents 6 months after children’s critical illness. Qual. Life Res. 29, 179–189 (2020).
Colville, G. A. & Pierce, C. M. Children’s self-reported quality of life after intensive care treatment. Pediatr. Crit. Care Med. 14, e85–e92 (2013).
Cunha, F. et al. Factors associated with health-related quality of life changes in survivors to pediatric intensive care. Pediatr. Crit. Care Med. 14, e8–e15 (2013).
Ducharme-Crevier, L. et al. PICU follow-up clinic: patient and family outcomes 2 months after discharge. Pediatr. Crit. Care Med. 22, 935–943 (2021).
Meert, K. L. et al. Health-related quality of life after community-acquired septic shock in children with preexisting severe developmental disabilities. Pediatr. Crit. Care Med. 22, e302–e313 (2021).
Buysse, C. M. et al. Surviving meningococcal septic shock in childhood: long-term overall outcome and the effect on health-related quality of life. Crit. Care 14, R124 (2010).
Smith, M. B. et al. The association of severe pain experienced in the PICU and post-discharge health-related quality of life: a retrospective cohort study. Paediatr. Anaesth. 32, 899–906 (2022).
Watson, R. S. et al. Risk factors for functional decline and impaired quality of life after pediatric respiratory failure. Am. J. Respir. Crit. Care Med. 200, 900–909 (2019).
van Gassel, R. J. J., Baggerman, M. R. & van de Poll, M. C. G. Metabolic aspects of muscle wasting during critical illness. Curr. Opin. Clin. Nutr. Metab. Care 23, 96–101 (2020).
Best, K. M., Boullata, J. I. & Curley, M. A. Risk factors associated with iatrogenic opioid and benzodiazepine withdrawal in critically ill pediatric patients: a systematic review and conceptual model. Pediatr. Crit. Care Med. 16, 175–183 (2015).
Puntillo, K. A. & Naidu, R. Chronic pain disorders after critical illness and ICU-acquired opioid dependence: two clinical conundra. Curr. Opin. Crit. Care 22, 506–512 (2016).
Herrup, E. A., Wieczorek, B. & Kudchadkar, S. R. Characteristics of postintensive care syndrome in survivors of pediatric critical illness: a systematic review. World J. Crit. Care Med. 6, 124–134 (2017).
Dervan, L. A., Killien, E. Y., Smith, M. B. & Watson, R. S. Health-related quality of life following delirium in the PICU. Pediatr. Crit. Care Med. 23, 118–128 (2022).
Ernst, M. M. et al. Biopsychosocial predictors of quality of life outcomes in pediatric congenital heart disease. Pediatr. Cardiol. 39, 79–88 (2018).
Svavarsdottir, E. K. & Tryggvadottir, G. B. Predictors of quality of life for families of children and adolescents with severe physical illnesses who are receiving hospital-based care. Scand. J. Caring Sci. 33, 698–705 (2019).
Rennick, J. E. & Childerhose, J. E. Redefining success in the PICU: new patient populations shift targets of care. Pediatrics 135, e289–e291 (2015).
Marcus, K. L., Henderson, C. M. & Boss, R. D. Chronic critical illness in infants and children: a speculative synthesis on adapting icu care to meet the needs of long-stay patients. Pediatr. Crit. Care Med. 17, 743–752 (2016).
Barnert, E. S. et al. A healthy life for a child with medical complexity: 10 domains for conceptualizing health. Pediatrics 142, e20180779 (2018).
Acknowledgements
The investigators sincerely thank all patients and families who participated in this investigation. The following is a summary of study performance sites, Principal Investigators (PI), Co-investigators (CI), Research Coordinators (RC), and Allied Research Personnel. Children’s Hospital of Michigan, Detroit, MI: Kathleen L. Meert, MD (PI); Sabrina Heidemann, MD (CI); Ann Pawluszka, BSN, RN (RC); Melanie Lulic, BS (RC). Children’s Hospital of Philadelphia, Philadelphia, PA: Robert A. Berg, MD (PI); Athena Zuppa, MD, MSCE (PI); Carolann Twelves, RN, BSN (RC); Mary Ann DiLiberto, BS, RN, CCRC (RC). Children’s National Medical Center, Washington, DC: Murray Pollack, MD (PI); David Wessel, MD (PI); John Berger, MD (CI); Elyse Tomanio, BSN, RN (RC); Diane Hession, MSN, RN (RC); Ashley Wolfe, BS (RC). Children’s Hospital of Colorado, Denver, CO: Peter Mourani, MD (PI); Todd Carpenter, MD (CI); Diane Ladell, MPH, CCRC (RC); Yamila Sierra, MPH, BS (RC); Alle Rutebemberwa, MPH, BS (RC). Nationwide Children’s Hospital, Columbus, OH: Mark Hall, MD (PI); Andy Yates, MD (CI); Lisa Steele, RN, BSN, CCRC, CCRN (RC); Maggie Flowers, BSN (RC); Josey Hensley, RN (RC). Mattel Children’s Hospital, University of California Los Angeles, Los Angeles, CA: Anil Sapru, MD, MBBS, MAS (PI); Rick Harrison, MD (CI), Neda Ashtari, BS(RC); Anna Ratiu, MPH (RC). Children’s Hospital of Pittsburgh, University of Pittsburgh Medical Center, Pittsburgh, PA: Joe Carcillo, MD (PI); Michael Bell, MD (CI); Leighann Koch, BS, BSN, RN (RC); Alan Abraham, CRC (RC). Benioff Children’s Hospital, University of California, San Francisco, San Francisco, CA: Patrick McQuillen, MD (PI); Anne McKenzie, BSN, CCRN (RC); Yensy Zetino, BS (RC). Children’s Hospital Los Angeles, University of Southern California, Los Angeles, CA: Christopher Newth, MD, FRCPC (PI); Jeni Kwok, JD, BS (RC); Amy Yamakawa, BS (RC). CS Mott Children’s Hospital, University of Michigan, Ann Arbor, MI: Michael Quasney, MD, PhD (PI); Thomas Shanley, MD (CI); C.J. Jayachandran, BS (RC). Cincinnati Children’s Hospital, Cincinnati, OH: Ranjit Chima, MD (PI); Hector Wong, MD (CI); Kelli Krallman, RN, BSN, MS, CCRC (RC); Erin Stoneman, CCRP (RC); Laura Benken, MBA, BS, CCRP (RC); Toni Yunger, BS (RC). St Louis Children’s Hospital, Washington University, St Louis, MO: Alan Doctor, RN, BSN (PI); Micki Eaton, RN, BSN (RC). Seattle Children’s Hospital, Seattle Children’s Research Institute (LAPSE Follow-up Center), University of Washington, Seattle, WA: Jerry J. Zimmerman, MD, PhD (PI); Catherine Chen, BS, CCRP (RC); Erin Sullivan, MPH (RC); Courtney Merritt, BA (RC); Deana Rich, BA (RC); Julie McGalliard, BA; Wren Haaland, MPH; Kathryn Whitlock, MS; Derek Salud, BS. University of Utah (Data Coordinating Center), Salt Lake City, UT: J. Michael Dean, MD, MBA (PI); Richard Holubkov, PhD (CI); Whit Coleman, MSRA, BSN, RN, CCRC (RC); Samuel Sorenson, BS (RC); Ron Reeder, PhD; Russell Banks, MS; Angie Webster, MStat; Jeri Burr, MS, RN-BC, CCRC; Stephanie Bisping, RN, BSN; Teresa Liu, MPH, CCRP; Emily Stock, BS; Kristi Flick, BS. Texas A&M University, College Station, TX: James W. Varni, PhD.
Funding
This study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development grants R03HD104001 (R.W.R.) and K23HD100566 (E.Y.K.). The LAPSE study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant R01HD073362, and was supported in part by the following cooperative agreements: UG1HD050096, UG1HD049981, UG1HD049983, UG1HD063108, UG1HD083171, UG1HD083166, UG1HD083170, U10HD050012, U10HD063106, and U01HD049934.
Author information
Authors and Affiliations
Contributions
E.Y.K.: conception and design, interpretation of data, article drafting, final manuscript approval. R.S.W.: conception and design, critical revisions for important intellectual content, final manuscript approval. R.K.B.: study design, data analysis, interpretation of data, final manuscript approval. R.W.R.: study design, data analysis, interpretation of data, final manuscript approval. K.L.M.: conception and design, acquisition of data, critical revisions for important intellectual content, final manuscript approval. J.J.Z.: conception and design, acquisition of data, critical revisions for important intellectual content, final manuscript approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
Informed consent was obtained from the parents or legal guardians of all study participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Killien, E.Y., Watson, R.S., Banks, R.K. et al. Predicting functional and quality-of-life outcomes following pediatric sepsis: performance of PRISM-III and PELOD-2. Pediatr Res 94, 1951–1957 (2023). https://doi.org/10.1038/s41390-023-02619-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02619-w