Abstract
Background
Health disparities surrounding pediatric severe sepsis outcomes remains unclear. We aimed to measure the relationship between indicators of socioeconomic status and mortality, hospital length of stay (LOS), and readmission rates among children hospitalized with severe sepsis.
Methods
Children 0–18 years old, hospitalized with severe sepsis in the Nationwide Readmissions Database (2016–2018) were included. The primary exposure was median household income by ZIP Code of residence, divided into quartiles.
Results
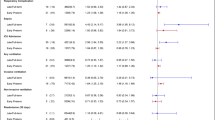
We identified 15,214 index pediatric severe sepsis hospitalizations. There was no difference in hospital mortality rate or readmission rate across income quartiles. Among survivors, patients in Q1 (lowest income) had a 2 day longer LOS compared to those in Q4 (Median 10 days [IQR 4–21] vs 8 days [IQR 4–18]; p < 0.0001). However, there was no difference after adjusting for multiple covariates.
Conclusions
Children living in Q1 had a 2 day longer LOS versus their peers in Q4. This was not significant on multivariable analysis, suggesting income quartile is not driving this difference. As pediatric severe sepsis remains an important source of morbidity and mortality in critically ill children, more sensitive metrics of socioeconomic status may better elucidate any disparities.
Impact
-
Children with severe sepsis living in the lowest income ZIP Codes may have longer hospital stays compared to peers in higher income communities.
-
More precise metrics of socioeconomic status are needed to better understand health disparities in pediatric severe sepsis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets analyzed during the current study are available in the Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project. https://www.hcup-us.ahrq.gov/nrdoverview.jsp
References
Weiss, S. L. et al. Global epidemiology of pediatric severe sepsis: the sepsis prevalence, outcomes, and therapies study. Am. J. Respir. Crit. Care Med. 191, 1147–1157 (2015).
Zimmerman, J. J. et al. Trajectory of mortality and health-related quality of life morbidity following community-acquired pediatric septic shock. Crit. Care Med. 329–337 (2020) https://doi.org/10.1097/CCM.0000000000004123.
Carlton, E. F., Kohne, J. G., Shankar-Hari, M. & Prescott, H. C. Readmission diagnoses after pediatric severe sepsis hospitalization. Crit. Care Med. 47, 583–590 (2019).
Carlton, E. F., Kohne, J. G., Hensley, M. K. & Prescott, H. C. Comparison of outpatient health care use before and after pediatric severe sepsis. JAMA Netw. Open 3, 9–12 (2020).
CSDH. Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. Geneva, World Health Organization. (2008).
Centers for Disease Control and Prevention. CDC Health Disparities and Inequalities Report—United States, 2013. Morb. Mortal. Wkly. report. Surveill. Summ. (Washington, D.C. 2013) 62, (2013).
Kachmar, A. G., Connolly, C. A., Wolf, S. & Curley, M. A. Q. Socioeconomic status in pediatric health research: a scoping review. J. Pediatr. 213, 163–170 (2019).
Mitchell, H. K. et al. Racial, ethnic, and socioeconomic disparities in paediatric critical care in the USA. Lancet Child Adolesc. Heal 5, 739–750 (2021).
Galiatsatos, P. et al. The association between neighborhood socioeconomic disadvantage and readmissions for patients hospitalized with sepsis. Crit. Care Med 48, 808–814 (2020).
Mitchell, H. K. et al. Hospital outcomes for children with severe sepsis in the USA by race or ethnicity and insurance status: a population- based, retrospective cohort study. Lancet Child Adolesc. Heal. (2020) https://doi.org/10.1016/S2352-4642(20)30341-2.
Reddy, A. R., Badolato, G. M., Chamberlain, J. M. & Goyal, M. K. Disparities associated with sepsis mortality in critically Ill children. J. Pediatr. Intensive Care (2020) https://doi.org/10.1055/s-0040-1721730.
Agency for Healthcare Research and Quality: NRD Overview. Healthcare Cost and Utilization Project. https://www.hcup-us.ahrq.gov/nrdoverview.jsp.
Dombrovskiy, V. Y., Martin, A. A., Sunderram, J. & Paz, H. L. Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit. Care Med. 35, 1244–1250 (2007).
Morgan, J. & Roberts, S. Maternal sepsis. Obstet. Gynecol. Clin. North Am. 40, 69–87 (2013).
AHRQ. HCUP Data Elements. https://www.hcup-us.ahrq.gov/partner/MOARef/HCUPdata_elements.pdf (2022).
Feudtner, C., Feinstein, J. A., Zhong, W., Hall, M. & Dai, D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 14, 1–7 (2014).
Prout, A. J. et al. Children with chronic disease bear the highest burden of pediatric sepsis. J. Pediatr. 199, 194–199.e1 (2018).
Estenssoro, E. et al. Health inequities in the diagnosis and outcome of sepsis in Argentina: a prospective cohort study. Crit. Care 23, 250 (2019).
Odetola, F. O., Gebremariam, A. & Freed, G. L. Patient and hospital correlates of clinical outcomes and resource utilization in severe pediatric sepsis. Pediatrics 119, 487–494 (2007).
Balamuth, F. et al. Identifying pediatric severe sepsis and septic shock: accuracy of diagnosis codes. J. Pediatr. 167, 1295–1300.e4 (2015).
Semega, J., Kollar, M., Creamer, J. & Mohanty, A. Income and poverty in the United States: 2018 Current Population Reports. U.S. Census Bur. Curr. Popul. Reports U.S. Gover, P60–P266 (2020).
Chang, L. V. et al. Lost earnings and nonmedical expenses of pediatric hospitalizations. Pediatrics 142, https://doi.org/10.1542/peds.2018-0195 (2018).
Carlton, E. F. et al. School and work absences after critical care hospitalization for pediatric acute respiratory failure: a secondary analysis of a cluster randomized trial. JAMA Netw. Open 4, e2140732 (2021).
Buttigieg, S. C., Abela, L. & Pace, A. Variables affecting hospital length of stay: a scoping review. J. Health Organ. Manag. 32, 463–493, https://doi.org/10.1108/JHOM-10-2017-0275 (2018).
Andrist, E., Riley, C. L., Brokamp, C., Taylor, S. & Beck, A. F. Neighborhood poverty and pediatric intensive care use. Pediatrics 144, e20190748 (2019).
Michel, M., Alberti, C., Carel, J.-C. & Chevreul, K. Association of pediatric inpatient socioeconomic status with hospital efficiency and financial balance + invited commentary + supplemental content and audio. JAMA Netw. Open 2, 1913656 (2019).
Chen, L. et al. Poverty related risk for potentially preventable hospitalisations among children in Taiwan. BMC Health Serv. Res. 10, 196 (2010).
Petrou, S. & Kupek, E. Socioeconomic differences in childhood hospital inpatient service utilisation and costs: prospective cohort study. J. Epidemiol. Community Health 59, 591–597 (2005).
Slain, K. N., Shein, S. L., Stormorken, A. G., Broberg, M. C. G. & Rotta, A. T. Outcomes of children with critical bronchiolitis living in poor communities. Clin. Pediatr. (Philos.). 57, 1027–1032 (2018).
Perelman, J., Shmueli, A. & Closon, M. C. Deriving a risk-adjustment formula for hospital financing: Integrating the impact of socio-economic status on length of stay. Soc. Sci. Med. 66, 88–98 (2008).
Picone, G., Wilson, R. M. & Chou, S.-Y. Analysis of hospital length of stay and discharge destination using hazard functions with unmeasured heterogeneity. Heal. Econ. Heal. Econ. 12, 1021–1034 (2003).
Prout, A. J. et al. Epidemiology of readmissions after sepsis hospitalization in children. Hosp. Pediatr. 9, 249–255 (2019).
Schnegelsberg, A. et al. Impact of socioeconomic status on mortality and unplanned readmission in septic intensive care unit patients. Acta Anaesthesiol. Scand. 60, 465–475 (2016).
Nacht, C. L. et al. Association between neighborhood disadvantage and pediatric readmissions. Matern. Child Health J. 26, 31–41 (2022).
Bettenhausen, J. L. et al. The association of the childhood opportunity index on pediatric readmissions and emergency department revisits. Acad. Pediatr. 22, 614–621 (2022).
Kachmar, A. G., Watson, R. S., Wypij, D., Perry, M. A. & Curley, M. A. Q. Association of socioeconomic status with postdischarge pediatric resource use and quality of life. Crit. Care Med. Publish Ah, 1–12 (2021).
Williams, E. & Takeaways, K. Children with special health care needs: coverage, affordability, and HCBS access. Kaiser Fam. Found. 1–16 (2021).
Galiatsatos, P. et al. Neighbourhood characteristics and health outcomes: evaluating the association between socioeconomic status, tobacco store density and health outcomes in Baltimore City. Tob. Control 27, e19–e24 (2018).
Galiatsatos, P., Sun, J., Welsh, J. & Suffredini, A. Health disparities and sepsis: a systematic review and meta-analysis on the influence of race on sepsis-related mortality. J. Racial Ethn. Heal. Disparities 6, 900–908 (2019).
Chinai, B., Gaughan, J. & Schorr, C. Implementation of the Affordable Care Act: A Comparison of Outcomes in Patients with Severe Sepsis and Septic Shock Using the National Inpatient Sample∗. Crit. Care Med. 783–789 (2020) https://doi.org/10.1097/CCM.0000000000004310.
Keisler-Starkey, K. & Bunch, L. N. Health Insurance Coverage in the United States: 2019 Current Population Reports. 1–20 (2020).
Lu, P. J. et al. Surveillance of vaccination coverage among adult populations—United States, 2018. Mmwr. Surveill. Summ. 70, 1–26 (2021).
Flavin, N. E. et al. Health insurance and the development of diabetic complications. South. Med. J. 102, 805–809 (2009).
Szanton, S. L., Gill, J. M. & Allen, J. K. Allostatic load: a mechanism of socioeconomic health disparities? Biol. Res. Nurs. 7, 7–15 (2005).
Johnson, S. B., Riley, A. W., Granger, D. A. & Riis, J. The science of early life toxic stress for pediatric practice and advocacy. Pediatrics 131, 319–327 (2013).
Recober, A. et al. Sociodemographic factors associated with hospital care for pediatric migraine: a national study using the kids’ inpatient dataset. Pediatr. Neurol. 91, 34–40 (2019).
Berkowitz, S. A., Traore, C. Y., Singer, D. E. & Atlas, S. J. Evaluating area-based socioeconomic status indicators for monitoring disparities within health care systems: Results from a primary care network. Health Serv. Res. 50, 398–417 (2015).
Figueroa, J. F., Frakt, A. B. & Jha, A. K. Addressing social determinants of health: time for a polysocial risk score. JAMA—J. Am. Med. Assoc. 323, 1553–1554 (2020).
Noelke, C. et al. Child Opportunity Index 2.0 Technical Documentation Child Opportunity Index 2.0 Technical Documentation. 1–51 (2020).
Rackers, H., Habteselasse, S., Lantos, H. & Redd, Z. A Review of Tools Measuring Opportunity in the United States. 1–18 (2020).
Hardeman, R. R., Homan, P. A., Chantarat, T., Davis, B. A. & Brown, T. H. Improving the measurement of structural racism to achieve antiracist health policy. Health Aff. 41, 179–186 (2022).
Acknowledgements
The authors would like to thank Mary Dahmer for her critical review of this manuscript.
Funding
Funding for this project was provided by the University of Michigan Department of Pediatrics Diversity, Equity and Inclusion Research Trainee Grant. No extramural funding sources were used.
Author information
Authors and Affiliations
Contributions
Each author has met the Pediatric Research authorship requirements. K.B.P., A.G., and E.F.C made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data. E.A., R.P.B., and G.L.F. helped in drafting and revising the article. All authors gave final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Phelps, K.B., Gebremariam, A., Andrist, E. et al. Children with severe sepsis: relationship between community level income and morbidity and mortality. Pediatr Res 94, 837–844 (2023). https://doi.org/10.1038/s41390-023-02500-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02500-w