Abstract
The National Institutes of Health’s Environmental influences on Child Health Outcomes (ECHO) Program was designed to address solution-oriented research questions about the links between children’s early life environment and their risks of pre-, peri-, and post-natal complications, asthma, obesity, neurodevelopmental disorders, and positive health. Children born very preterm are at increased risk for many of the outcomes on which ECHO focuses, but the contributions of environmental factors to this risk are not well characterized. Three ECHO cohorts consist almost exclusively of individuals born very preterm. Data provided to ECHO from cohorts can be used to address hypotheses about (1) differential risks of chronic health and developmental conditions between individuals born very preterm and those born at term; (2) health disparities across social determinants of health; and (3) mechanisms linking early-life exposures and later-life outcomes among individuals born very preterm.
Impact
-
The National Institutes of Health’s Environmental Influences on Child Health Outcomes Program is conducting solution-oriented research on the links between children’s environment and health.
-
Three ECHO cohorts comprise study participants born very preterm; these cohorts have enrolled, to date, 1751 individuals born in 14 states in the U.S. in between April 2002 and March 2020.
-
Extensive data are available on early-life environmental exposures and child outcomes related to neurodevelopment, asthma, obesity, and positive health.
-
Data from ECHO preterm cohorts can be used to address questions about the combined effects of preterm birth and environmental exposures on child health outcomes.
Similar content being viewed by others
Introduction
The National Institutes of Health-funded Environmental influences on Child Health Outcomes (ECHO) Program seeks to promote the health and well-being of children in the United States (U.S.) through solution-oriented research. Its overarching goal is to characterize relationships between the environment and children’s health.1 The ECHO Program focuses on pre-, peri-, and postnatal outcomes; neurodevelopmental disorders; asthma; obesity; and positive health. The ECHO Program interprets the environment broadly as including psychosocial factors, chemical exposures, the physical environment, and home and community resources. The ECHO-wide cohort comprises 69 existing cohorts of children and their parents or guardian. Cohorts differ in age and inclusion criteria at enrollment, current life stage, race and ethnic distribution, and geographic region of residence. These differences provide opportunities for harmonizing large datasets, thereby allowing examination of specific questions amongst subgroups of children who may have unique susceptibilities.
Children who are born very preterm (before 32 weeks of gestation) or extremely preterm (before 28 weeks of gestation) are at increased risk for multiple adverse health outcomes. For example, in the Extremely Low Gestational Age Newborn (ELGAN) Study,2 one of the largest research cohorts of individuals born extremely preterm, the frequencies of asthma,3 attention deficit hyperactivity disorder,4 epilepsy,5 autism spectrum disorder,6 and cognitive impairment7 were at least four times the frequencies found in population-based estimates of prevalence among children born at term in the U.S. Thus, ECHO cohorts comprising children born very preterm or extremely preterm will enhance the statistical power of studies of neurodevelopmental disorders and asthma.
The ELGAN cohort is one of three ECHO cohorts composed almost entirely of individuals born very preterm; the other two are the Neonatal Neurobehavior and Outcomes in Very Preterm Infants (NOVI) cohort and the Developmental Impact of Neonatal Intensive Care Unit Exposures (DINE) cohort. In addition to these three cohorts, other cohorts in ECHO that are not composed exclusively of individuals born very preterm have enrolled individuals born very preterm.
Our rationale for focusing this article on the potential contributions of the three ECHO cohorts composed exclusively of individuals born preterm is twofold. First, all three of these cohorts collected detailed data on neonatal morbidities, such as bronchopulmonary dysplasia (BPD) and brain abnormalities identified with neonatal ultrasound, conditions that often are important covariates in analyses of child health outcomes. Second, these three ECHO cohorts account for 97% of very preterm individuals who have consented to participate in ECHO. This subgroup of ECHO participants is at very high risk for health disorders.8
Our goal is to serve as a “roadmap” to aid child health researchers in their efforts to apply data from the ECHO preterm cohorts toward the broad goals of the ECHO program. First, we describe the initial research goals, selection criteria, and key exposures and outcomes for the three preterm infant ECHO cohorts. The rich extant data (data available prior to the start of the ECHO Program) from these cohorts, coupled with new data collected on study participants using the ECHO-wide data collection protocol, is creating a rich and unique dataset to address critical and impactful research questions regarding children born preterm; thus we will describe ways to access data from the ECHO Program. Second, we outline four areas of child health research where data from these preterm infant cohorts are likely to be particularly valuable: (1) identification of modifiable risk factors for adverse child health outcomes, (2) developmental origins of health, (3) health disparities across social class, and (4) resiliency factors that moderate the long-term effects of early-life adversity.
Cohorts of individuals born very preterm
Table 1 summarizes demographic and neonatal characteristics of the three ECHO cohorts of individuals born very preterm. Tables 2–4 summarize follow-up assessments that have been completed or are ongoing in the three cohorts. Information about other variables that are being collected from ECHO study participants can be found in the ECHO-wide Cohort Data Collection Protocol, using this link: https://echochildren.org/echo-program-protocol/. The following three sections provide additional background and details about the three ECHO cohorts of individuals born very preterm.
NOVI
The aim of the NOVI Study was to determine whether neurobehavioral abnormalities at discharge can identify infants with impairment at 2 years corrected age and whether cumulative medical risk and the post-discharge caregiving environment modify associations between neurodevelopmental status at discharge and at 2 years corrected age. The NOVI Study cohort was enrolled from April 2014 through June 2016 at nine university-affiliated neonatal intensive care units (NICUs) in seven U.S. cities: Providence, Rhode Island; Grand Rapids, Michigan; Kansas City, Missouri; Honolulu, Hawaii; Winston-Salem, North Carolina; and Torrance and Long Beach, California. These NICUs were also participating in the Vermont Oxford Network for quality improvement, and the database for that network was used as a source of data for neonatal morbidities. Eligibility was determined based on the following inclusion criteria: (1) birth at <30 weeks postmenstrual age (PMA); (2) parental ability to read and speak English or Spanish; and (3) residence within 3 h of the NICU and follow-up clinic. Exclusion criteria included maternal age <18 years, maternal cognitive impairment, maternal or infant death, and major congenital anomalies. Parents of eligible infants were invited to participate in the study when survival to discharge was determined to be likely by the attending neonatologist. Of 709 infants consented, 704 enrolled, and 679 (96% of those enrolled) had complete neurobehavioral assessment data and 624 (88% of enrollees) had buccal cells collected for epigenomic screening. At the time of the follow-up assessment at 2 years corrected age, 566 infants participated (80% of enrollees). With additional funding from ECHO, 495 (70% of enrollees) children and 440 (62% of enrollees) children participated at 3 and 4 years, respectively. Currently, visits are being completed when NOVI participants are 4.5 and 5 years of age using the ECHO-wide Cohort Protocol. The major findings from NOVI, thus far, relate to associations between infant atypical neurobehavior and specific medical problems such as infant sepsis9 and brain injury.10 These infants also displayed unique epigenetic changes11 and were born to mothers with adverse medical and psychosocial conditions.12 Longitudinal collection of buccal cells, which has provided insight into DNA methylation changes related to neurobehavior and medical health,12,13,14 will allow for deeper understanding of epigenetic changes over time.
DINE
The DINE study unites participants previously enrolled in one of the four NICU-based NIH-supported studies into a single harmonized study cohort. These four studies include the Prematurity and Respiratory Outcomes Program (PROP),15 the Trial of Late Surfactant (TOLSURF) study,16 the Preterm Erythropoietin Neuroprotection Trial (PENUT),17 and the Neonatal Intensive Care Unit Hospital Exposures and Long-Term Health (NICU-HEALTH) study.18 Between January 2010 and March 2020, DINE participants were recruited into their parent study based on enrollment criteria at one of the eight university-affiliated NICUs in New York, New York; Rochester, New York; Buffalo, New York; Nashville, Tennessee; Cincinnati, Ohio; Winston-Salem, North Carolina; Minneapolis, Minnesota; and Jacksonville, Florida. Each parent cohort collected detailed clinical, demographic, and developmental data as well as a rich repository of biospecimens during their initial enrollment period.
PROP was a multi-center, observational, prospective cohort study of 835 preterm infants born at 23–28 completed weeks of gestation between August 2011 and November 2013 (ClinicalTrials.gov NCT01435187).15,19,20,21,22 PROP was a U01 collaboration between the National Heart, Lung, and Blood Institute (NHLBI), a data coordinating center, and 6 clinical centers, with NICUs at 13 hospitals. Of the original NICUs in PROP, 34 clinical centers with 6 recruitment hospitals currently participate in ECHO-DINE. A key aim of PROP was to identify clinical, physiologic, and biochemical markers during NICU hospitalization that predict respiratory morbidity through 1 year of age. Each PROP center participated in multiple hypothesis-driven, biomarker-based studies investigating mechanistic pathways associated with BPD (chronic lung disease of prematurity) and respiratory morbidity one year after hospital discharge. Post-NICU discharge data were obtained at 3, 6, 9, and 12 months corrected age. A diagnosis of BPD at 36 weeks PMA was made in 41% of the cohort; 68% of the cohort experienced respiratory morbidity through 1 year of age.
TOLSURF was an NHLBI-supported masked, randomized, sham-controlled trial conducted in 25 U.S. hospitals to determine the effect of late doses of surfactant on BPD at 36 weeks PMA in preterm infants receiving inhaled nitric oxide (U01HL094338; PI: Roberta Ballard, MD; ClinicalTrials.gov NCT01022580).16,23 Preterm infants were eligible for TOLSURF if they were <28 weeks gestation and required intubation and mechanical ventilation between 7 and 14 days of age. TOLSURF enrolled 511 infants across 25 sites between January 2010 and September 2013. Compared with PROP, infants in TOLSURF had a lower mean birth weight and lower gestational age and were enrolled in week 2 of life rather than week 1. Exclusion criteria were life-threatening congenital abnormalities or airway anomalies, clinical instability, or low likelihood of being available for long-term follow-up. TOLSURF reported that survival without BPD did not differ between the surfactant-treated group and the control group at 36 weeks PMA (31.3 vs 31.7%; 95% CI, 0.75–1.28; P = 0.89).16 TOLSURF infants were followed via pulmonary questionnaires every 3–6 months through 24 months and underwent assessment of neurodevelopmental outcomes at 24 months. Three of the highest enrolling TOLSURF sites participate in the ECHO DINE study.
PENUT was a randomized, multi-center, placebo-controlled trial funded by the National Institute of Neurological Disorders and Stroke (NINDS) to assess whether early high-dose erythropoietin improved survival without neurodevelopmental impairment in infants born between 24 and 28 weeks’ gestational age at 19 centers across the U.S. between December 2013 and September 2016 (U01NS077953; PI: Sandra Juul, MD, PhD; ClinicalTrials.gov NCT01378273).24,25,26 Infants in PENUT were enrolled at <24 h of age. Infants underwent neurodevelopmental assessment at 2 years of age. Exclusion criteria and data collection elements in PENUT closely resemble those in TOLSURF and PROP. Three PENUT sites, which also participated in TOLSURF, participate in the ECHO DINE study. PENUT investigators recently reported that high-dose erythropoietin treatment administered to extremely preterm infants from 24 h after birth through 32 weeks PMA did not result in a lower risk of severe neurodevelopmental impairment or death at 2 years of age.24
NICU-HEALTH was designed from its inception as an environmental health birth cohort study of preterm infants (K23ES022268; PI: Annemarie Stroustrup, MD; ClinicalTrials.gov NCT01420029, NCT01963065).18,27,28,29,30 Funded by the National Institute of Environmental Health Sciences (NIEHS), NICU-HEALTH enrolled 320 infants born at <33 weeks’ gestational age at Mount Sinai Hospital in New York City in two phases between September 2011 and March 2020. NICU-HEALTH collected comprehensive information about both chemical and non-chemical exposures during NICU hospitalization and evaluated the impact of the NICU environment on neurobehavioral outcomes through early childhood. Comprehensive clinical and exposure data, questionnaire information, and biospecimens were collected through the NICU stay and then following discharge to 2 years of age. Longitudinal follow-up included multiple objective and survey assessments of temperament and cognitive, motor, and behavioral performance; questionnaires about home-based environmental exposures and medical comorbidities, including pulmonary outcomes; and biospecimen collection at 3, 6, 12, and 24 months corrected age (age corrected for degree of prematurity). Participants from a subset of parent study sites were re-recruited into DINE with the goal of identifying and quantifying the impact of hospital-based exposures early in life on the long-term development of children born preterm.
Thus far, DINE has re-recruited 549 participants to the ECHO Program with a target enrollment of 655. DINE participants complete annual follow-up visits under the ECHO-Wide Cohort Protocol.
ELGAN
Neonates were enrolled at 14 hospitals in five U.S states between April 2002 and August 2004. The only inclusion criterion was birth before 28 weeks’ gestational age. The only exclusion criterion was anencephaly. ELGAN enrolled 1506 infants, of whom 1200 survived to discharge from the NICU. At the time of the first comprehensive neurodevelopmental assessment at 2 years of age adjusted for prematurity, a total of 1086 infants participated (91% of those surviving to 2 years of age); at the time of the second assessment at 10 years of age, 889 children participated (74% of those surviving to 10 years of age); and at the time of the third assessment at 15 years of age (completed with funding from ECHO), 694 adolescents participated (58% of those surviving to 15 years of age). The overarching hypothesis of the ELGAN Study is that perinatal inflammation is associated with brain structural and functional disorders. To address this hypothesis, placentae were examined for microbes and histological evidence of inflammation. Protein biomarkers of inflammation were measured in neonatal blood, and neonatal and maternal medical records were reviewed for clinical complications and therapies indicative of infection or inflammation. Abundant support for the ELGAN Study’s central hypothesis has been described.31,32,33,34,35,36,37,38,39,40,41,42,43,44,45 While the initial focus of the ELGAN Study was inflammation in the neonate and neurodevelopment, the cohort has also been characterized in terms of placental inflammation,46,47,48 placental epigenetic modification and gene expression,49,50,51,52,53,54,55,56,57 obesity,58,59 asthma,3 and positive health.60
The strengths of the ELGAN Study include longitudinal assessments of cognition, behavior, body mass index/obesity, and asthma (at 2, 10, and 15 years of age); placental microbiology, histology, CpG methylation, miRNAs, transcriptome, and proteomics; and brain magnetic resonance at 15 years of age.
Accessing ECHO Program data
The ECHO Program provides support for 39 cohort awards, a coordinating center, a data analysis center, a Participant-Reported Outcomes Measurement Information System core, and Human Health Exposure Analysis Research core. Investigators who receive funding support from ECHO or who are designated as affiliate investigators may propose analyses of data and publications to the ECHO Publications Committee for review. The URL for the ECHO Publications website is https://echochildren.org/echo-program-publications/. Thus one pathway by which investigators who are not currently affiliated with ECHO can gain access to ECHO data is identify a ECHO Award principal investigator to sponsor the investigator as an affiliate ECHO investigator. A list of ECHO Award principal investigators can be found at https://echochildren.org/map-echo-cohorts-observational-study-sites/. Investigators may contact the ECHO-wide Cohort (ECHO-DAC@rti.org) to collaborate with an ECHO investigator.
Investigators who wish to analyze data outside of a collaboration with ECHO investigators can obtain a public use dataset that is expected to be available in July 2022. A limitation of the public use dataset is that it will contain records only for individuals who have consented to ECHO participation at level 2 participation level (defined as consent to share residential address and exact dates, such as date of birth). In contrast, by collaborating with an ECHO investigator, a researcher can gain access to all of the extant data stored at the ECHO Data Analysis Center.
Research priorities for preterm ECHO cohorts
While not an exhaustive list of prioritized projects, this section presents a high-level view of research opportunities using data from the DINE, NOVI, and ELGAN ECHO cohorts; Table 5 lists selected examples of ongoing projects involving ECHO very preterm cohorts. Exposures in these projects include community-level factors such as air pollution and the built environment, maternal factors such as maternal illnesses and medications, neonatal therapies such as acid suppression medications, and post-NICU exposures such as infant weight gain and the COVID pandemic. Outcomes under study include placenta CpG DNA methylation, BPD, neonatal neurobehavior, behavioral dysregulation, early cognitive functioning, autism, attention deficit hyperactivity disorder, body mass index, sleep health, and positive health.
Identification of modifiable risk factors for adverse child health outcomes
An overarching goal of the ECHO Program is to identify modifiable risk factors for obesity, asthma, and neurodevelopmental impairments, as well as factors associated with positive health, which will be discussed below in the section on resiliency. Except for obesity, the adverse outcomes on which ECHO focuses are more frequent among individuals born very preterm, increasing statistical power when analyzing associations between early life risk factors and child health outcomes.
Few studies have followed extremely preterm children starting at birth and extending through childhood, and few have the extensive biological and developmental data, and data on environment and exposures during childhood, that are needed to support rigorous investigations on etiology. Further, environmental health studies often exclude participants born very preterm. This lack of understanding about etiology and environment presents a critical barrier to progress toward preventing adverse outcomes and promoting positive child health among individuals born preterm. To help address this knowledge gap, the ECHO very preterm cohorts have collected data on early life exposures that are potentially related to child health outcomes; examples include placental pathology (ELGAN), maternal postpartum depression and substance use (NOVI), high-reliability cranial ultrasound interpretations (ELGAN, DINE, and NOVI), details of pulmonary course and outcomes (DINE), phthalate exposures in the NICU (DINE), and clinical markers of acute neonatal kidney injury (DINE).
For the identification of modifiable risk factors, ECHO cohorts composed primarily of individuals not born very preterm provide a large number of controls (individuals born at term). By comparing early childhood environmental exposures for very preterm infants and controls, ECHO is poised to increase understanding of the relative contribution of pre- and post-NICU factors in the development of adverse child health outcomes for which very preterm children are at higher risk. Studies of this type can inform priorities and the design of programs to improve the health of individuals born very preterm.
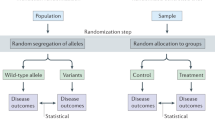
Developmental origins of health
A priority of ECHO very preterm cohorts is to increase understanding of potential mediators of preterm birth-outcome associations, such as parental stress, social determinants of health, and epigenetic variation. This priority aligns with the burgeoning field of the developmental origins of health, which hypothesizes that early-life exposures can program metabolic, immunologic, epigenetic, or physiologic responses that have persisting effects on health.61,62 To facilitate mechanistic studies of the developmental origins of health, ECHO preterm cohorts have collected data on biomarkers of potential mechanisms linking early-life exposures and later-life outcomes, such as epigenetic markers in the placenta52,53,63 and neonatal tissues,12 biomarkers of neonatal inflammation,64,65 and chemical exposures during neonatal intensive care in the first several postnatal months.18 Like the “canary in the coal mine,” it seems likely that at least some of the findings from mechanistic studies will pertain not just to individuals born preterm but also to those born at term.66
Understanding disparities across social determinants of health
In the U.S., child health outcomes on which the ECHO Program concentrates (preterm and low birth weight birth, asthma, obesity, and neurodevelopmental disorders), are more prevalent among non-Hispanic Black children than among non-Hispanic White children.67,68,69,70,71 Identifying factors that contribute to health disparities across race, as well as factors that promote health equity, is an essential step in improving the health of children in the U.S.
Recent epidemiological studies of health disparity across race have focused on social determinants of health, including such factors as systemic racism, environmental pollution, and poverty. Black families, as compared to White families, are more likely to have indicators of socioeconomic disadvantage, such as lower quality housing, and psychological stress,69,70 and have greater exposure to air pollution, lead exposure,72,73,74 neighborhood violence,75,76 racial segregation and discrimination,75,77 and adverse life events. Conversely, Black families are less likely to have access to high-quality daycare78 and nutritious foods during pregnancy. Maternal diet can influence the risks of preterm birth and fetal growth restriction,79 and iron deficiency during pregnancy is associated with worse neurodevelopmental outcomes in the offspring.79
The ECHO-wide cohort protocol includes collection of data across multiple domains related to social determinants of health. Residential address history is being used to derive indicators of structural racism, including neighborhood-level measures of deprivation, segregation, and urbanicity. The Everyday Discrimination Scale80 is being collected to capture self-perceived racism. Family-level markers of economic resources include household income and source of the family’s medical insurance. At the level of mothers and caregivers, data are being collected on educational attainment and occupation, as well as diet, sleep, substance use, and environmental exposures during pregnancy. Data from DINE, NOVI, and ELGAN cohorts are an important resource in analyses of preterm birth as both an outcome of social determinants of health as well as a mediator between social determinants of health and adverse child health outcomes.
Health disparities during the infant’s hospitalization in NICUs81,82,83,84,85,86,87 include nurse understaffing and higher rates of infection,82,83,85,88 mortality,81,84,86,89,90,91 and neonatal morbidities.92 Notably, in NICUs rated as higher quality, differences in morbidity between Black and White infants are smaller.90,93
Disparities across race/ethnicity also have been found among hospital patients. Compared with Black and Hispanic infants, White infants were more likely to receive appropriately timed retinal examinations, antenatal steroid therapy, and breastfeeding education82,85 Parents and healthcare providers report that less attention and education was provided to families of color compared with White families.82 Following discharge from the NICU, families with fewer financial resources have greater difficulty accessing health care.94 Families in rural communities, which typically are farther from regional medical centers, face a larger challenge attending follow-up appointments.95 Thus, health disparities across race are present in the pre-conception interval, and continue during pregnancy and neonatal intensive care hospitalization, and after discharge of infants into the community.81
The coronavirus disease 2019 (COVID-19) pandemic has accentuated health disparities across social class. Given the association between preterm birth and lower socioeconomic status (SES), disparities across indicators of SES in COVID-related health outcomes,96,97 and COVID-19–related disruptions to educational support, we expect that pandemic effects on health and educational outcomes will be larger among children born preterm compared with those born at term.98,99 In the spring of 2020, the ECHO Program modified its study protocol to include the collection of data on disruptions in children’s education, stress, and coping during the COVID-19 pandemic. In the three ECHO cohorts of individuals born very preterm, 1096 individuals have completed questionnaires about the impact of the COVID-19 pandemic on their lives. These ECHO data, combined with data from ECHO cohorts born predominantly at term, form a large racially and ethnically diverse sample for addressing questions related to race, racism, and social determinants of health as modifiers of associations between pandemic-related restrictions and child health outcomes. Further, the longitudinal design of each of the three preterm cohorts provides data on cohort members’ health and developmental outcomes before, during, and after the pandemic.
How can ECHO preterm cohorts inform research on resiliency factors that may moderate the long-term effects of early life adversity?
Despite the many pre-, peri-, and post-natal adversities encountered by fetuses delivered extremely preterm, as many as one-third of children born before 28 weeks’ gestational age who are discharged alive from the NICU have a positive health outcome, defined as the absence of intellectual deficit, cerebral palsy, epilepsy, autism spectrum disorder, severe hearing or visual impairment, obesity, asthma, attention deficit hyperactivity disorder, anxiety, and depression at 10 years of age.60 A goal of the ECHO Program is to identify factors associated with positive health outcomes,100 defined as “a set of resources that are used to adapt to environmental challenges, satisfy needs, and reach a person’s goals … assets that strengthen an individual’s health.”100
Related to positive health is resilience, defined as “a multisystemic dynamic process of successful adaption or recovery in the context of risk or a threat.”101 Factors that confer resilience are those that promote well-being or protect against adverse outcomes in children and adolescents who are at increased risk. For example, in a large Norwegian cohort of adolescents 16–19 years of age, a higher number of negative life events experienced by study participants was correlated with increased depressive symptoms, whereas fewer symptoms were reported by adolescents with potential protective factors, such as goal orientation, self-confidence, social competence, social support, and family cohesion. These findings suggest that even among children who experience negative life events, interventions to enhance resilience factors, such as social support and family cohesion, could reduce the frequency of depression.102
Among children born with extremely low birth weight, resilience was associated with higher SES and favorable proximal home factors, such as higher stimulation for learning, higher parent-child relationship quality, and lower parent burden and distress.103 In the ELGAN cohort, a positive health outcome was associated with higher SES and the absence of pre-pregnancy chronic maternal medical disorders, such as pre-pregnancy obesity or asthma.104
Identifying factors that promote positive health provides targets for interventions to improve outcomes after very preterm birth. Proximal factors associated with higher SES, such as social support for parents, and enhanced educational stimulation, can be provided by supportive programs for families to improve health outcomes after very preterm birth. Direct assessment of parents’ social support and educational resources, with instruments such as the Home Observation for Measurement of the Environment Inventory,105 could identify families with greater need of supportive interventions.
In addition to identifying targets for intervention, ECHO researchers are focusing on identifying the mechanisms by which early life factors confer resiliency. Findings from the NOVI and ELGAN cohorts support the developmental origins of disease hypothesis and suggest that epigenetic markers in the placenta54,55 and neonatal tissue12 are sensitive to early life exposures and are predictive of child health outcomes.50,63 Taken together, these findings suggest that epigenetic modifications could be a mechanism linking early-life exposures to health outcomes in childhood and beyond. Studies from the ELGAN cohort indicate that neonatal systemic inflammation is associated with prenatal factors, such as SES,106 placenta microorganisms,107 and maternal obesity,108 and is also associated with child outcomes 10 years later.31,34,36,109 Thus, neonatal inflammation is another potential mechanism for the developmental origins of health and disease.
Summary
The ECHO-wide cohort study is a resource for researchers interested child health outcomes among individuals born very preterm. Data from very preterm children currently participating in the ECHO-wide cohort, together with about 30,000 children born at term will soon be available publically, and will include information about a broad range of environmental exposures and outcomes related to chronic illness among U.S. children. This resource provides child health researchers with many opportunities to improve understanding of modifiable risk factors and mechanisms leading to chronic illness in children, pointing the way to interventions to optimize the well-being of children in the U.S.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Data availability
The datasets for this manuscript are not publicly available, because per the NIH-approved ECHO Data Sharing Policy, ECHO-wide data have not yet been made available to the public for review/analysis. Requests to access the datasets should be directed to the ECHO Data Analysis Center, ECHO-DAC@rti.org.
References
Blaisdell, C. J. et al. The NIH ECHO Program: investigating how early environmental influences affect child health. Pediatr. Res. https://doi.org/10.1038/s41390-021-01574-8 (2021).
O’Shea, T. M. et al. The ELGAN study of the brain and related disorders in extremely low gestational age newborns. Early Hum. Dev. 85, 719–725 (2009).
Jackson, W. M. et al. Risk factors for chronic lung disease and asthma differ among children born extremely preterm. Pediatr. Pulmonol. 53, 1533–1540 (2018).
Scott, M. N. et al. Neurocognitive correlates of attention-deficit hyperactivity disorder symptoms in children born at extremely low gestational age. J. Dev. Behav. Pediatr. 38, 249–259 (2017).
Douglass, L. M. et al. Cumulative incidence of seizures and epilepsy in ten-year-old children born before 28 weeks’ gestation. Pediatr. Neurol. 73, 13–19 (2017).
Joseph, R. M. et al. Prevalence and associated features of autism spectrum disorder in extremely low gestational age newborns at age 10 years. Autism Res. 10, 224–232 (2017).
Joseph, R. M. et al. ELGAN Study Investigators. Neurocognitive and academic outcomes at age 10 years of extremely preterm newborns. Pediatrics 137, e20154343 (2016).
Risnes, K. et al. Mortality among young adults born preterm and early term in 4 Nordic nations. JAMA Netw. Open 4, e2032779 (2021).
Hofheimer, J. A. et al. Psychosocial and medical adversity associated with neonatal neurobehavior in infants born before 30 weeks gestation. Pediatr. Res. 87, 721–729 (2020).
Helderman, J. et al. Association of abnormal findings on neonatal cranial ultrasound with neurobehavior at neonatal intensive care unit discharge in infants born before 30 weeks’ gestation. JAMA Netw. Open 5, e226561 (2022).
McGowan, E. C. et al. Sociodemographic and medical influences on neurobehavioral patterns in preterm infants: a multi-center study. Early Hum. Dev. 142, 104954 (2020).
Everson, T. M. et al. Serious neonatal morbidities are associated with differences in DNA methylation among very preterm infants. Clin. Epigenet. 12, 151 (2020).
Everson, T. M. et al. Epigenome-wide analysis identifies genes and pathways linked to neurobehavioral variation in preterm infants. Sci. Rep. 9, 6322 (2019).
Aghagoli, G. et al. Epigenome-wide analysis identifies genes and pathways linked to acoustic cry variation in preterm infants. Pediatr. Res. 89, 1848–1854 (2021).
Pryhuber, G. S. et al. Prematurity and respiratory outcomes program (PROP): study protocol of a prospective multicenter study of respiratory outcomes of preterm infants in the United States. BMC Pediatr. 15, 37 (2015).
Ballard, R. A. et al. Randomized trial of late surfactant treatment in ventilated preterm infants receiving inhaled nitric oxide. J. Pediatr. 168, 23.e4–29.e4 (2016).
Juul, S. E., Mayock, D. E., Comstock, B. A. & Heagerty, P. J. Neuroprotective potential of erythropoietin in neonates; design of a randomized trial. Matern. Health Neonatol. Perinatol. 1, 27 (2015).
Stroustrup, A. et al. Cohort profile: the Neonatal Intensive Care Unit Hospital Exposures and Long-Term Health (NICU-HEALTH) cohort, a prospective preterm birth cohort in New York City. BMJ Open 9, e032758 (2019).
Islam, J. Y., Keller, R. L., Aschner, J. L., Hartert, T. V. & Moore, P. E. Understanding the short- and long-term respiratory outcomes of prematurity and bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 192, 134–156 (2015).
Poindexter, B. B. et al. Comparisons and limitations of current definitions of bronchopulmonary dysplasia for the Prematurity and Respiratory Outcomes Program. Ann. Am. Thorac. Soc. 12, 1822–1830 (2015).
Maitre, N. L. et al. Respiratory consequences of prematurity: evolution of a diagnosis and development of a comprehensive approach. J. Perinatol. 35, 313–321 (2015).
Keller, R. L. et al. Bronchopulmonary dysplasia and perinatal characteristics predict 1-year respiratory outcomes in newborns born at extremely low gestational age: a prospective cohort study. J. Pediatr. 187, 89–97 e83 (2017).
Ballard, P. L. et al. Inhaled nitric oxide increases urinary nitric oxide metabolites and cyclic guanosine monophosphate in premature infants: relationship to pulmonary outcome. Am. J. Perinatol. 32, 225–232 (2015).
Juul, S. E. et al. A randomized trial of erythropoietin for neuroprotection in preterm infants. N. Engl. J. Med. 382, 233–243 (2020).
Juul, S. E. & Ferriero, D. M. Pharmacologic neuroprotective strategies in neonatal brain injury. Clin. Perinatol. 41, 119–131 (2014).
Rangarajan, V. & Juul, S. E. Erythropoietin: emerging role of erythropoietin in neonatal neuroprotection. Pediatr. Neurol. 51, 481–488 (2014).
Pourkaviani, S. et al. Clinical validation of the Neonatal Infant Stressor Scale with preterm infant salivary cortisol. Pediatr. Res. 87, 1237–1243 (2020).
Stroustrup, A. et al. Neonatal intensive care unit phthalate exposure and preterm infant neurobehavioral performance. PLoS ONE 13, e0193835 (2018).
Stroustrup, A. et al. Sources of clinically significant neonatal intensive care unit phthalate exposure. J. Expo. Sci. Environ. Epidemiol. 30, 137–148 (2020).
Zhang, X. et al. The association of prenatal exposure to intensive traffic with early preterm infant neurobehavioral development as reflected by the NICU Network Neurobehavioral Scale (NNNS). Environ. Res. 183, 109204 (2020).
Korzeniewski, S. A., Allred, E. N., O’Shea, T. M., Leviton, A. & Kuban, K. C. K. Elevated protein concentrations in newborn blood and the risks of autism spectrum disorder, and of social impairment, at age 10 years among infants born before the 28th week of gestation. Transl. Psychiatry 8, 115 (2018).
Kuban, K. C. et al. The breadth and type of systemic inflammation and the risk of adverse neurological outcomes in extremely low gestation newborns. Pediatr. Neurol. 52, 42–48 (2015).
Kuban, K. C. et al. Systemic inflammation and cerebral palsy risk in extremely preterm infants. J. Child Neurol. 29, 1692–1698 (2014).
Kuban, K. C. et al. Association of circulating proinflammatory and anti-inflammatory protein biomarkers in extremely preterm born children with subsequent brain magnetic resonance imaging volumes and cognitive function at age 10 years. J. Pediatr. 210, 81–90 e83 (2019).
Kuban, K. C. et al. Circulating inflammatory-associated proteins in the first month of life and cognitive impairment at age 10 years in children born extremely preterm. J. Pediatr. 180, 116.e1–123.e1 (2017).
Kuban, K. J. et al. Among children born extremely preterm a higher level of circulating neurotrophins is associated with lower risk of cognitive impairment at school age. J. Pediatr. 201, 40.e4–48.e4 (2018).
Leviton, A. et al. Circulating biomarkers in extremely preterm infants associated with ultrasound indicators of brain damage. Eur. J. Paediatr. Neurol. 22, 440–450 (2018).
Leviton, A. et al. Neonatal systemic inflammation and the risk of low scores on measures of reading and mathematics achievement at age 10 years among children born extremely preterm. Int. J. Dev. Neurosci. 66, 45–53 (2018).
Leviton, A. et al. Two-hit model of brain damage in the very preterm newborn: small for gestational age and postnatal systemic inflammation. Pediatr. Res. 73, 362–370 (2013).
Leviton, A. et al. Early postnatal blood concentrations of inflammation-related proteins and microcephaly two years later in infants born before the 28th post-menstrual week. Early Hum. Dev. 87, 325–330 (2011).
Leviton, A. et al. The relationship between early concentrations of 25 blood proteins and cerebral white matter injury in preterm newborns. J. Pediatr. 158, 897–903 (2011).
Leviton, A. J. et al. The risk of neurodevelopmental disorders at age 10 years associated with blood concentrations of interleukins 4 and 10 during the first postnatal month of children born extremely preterm. Cytokine 110, 181–188 (2018).
O’Shea, T. M. et al. Elevated concentrations of inflammation-related proteins in postnatal blood predict severe developmental delay at 2 years of age in extremely preterm infants. J. Pediatr. 160, 395–401 (2012).
O’Shea, T. M. et al. Elevated blood levels of inflammation-related proteins are associated with an attention problem at age 24 mo in extremely preterm infants. Pediatr. Res. 75, 781–787 (2014).
O’Shea, T. M. et al. Inflammation-initiating illnesses, inflammation-related proteins, and cognitive impairment in extremely preterm infants. Brain Behav. Immun. 29, 104–112 (2013).
Hecht, J. L. et al. Relationship between neonatal blood protein concentrations and placenta histologic characteristics in extremely low GA newborns. Pediatr. Res. 69, 68–73 (2011).
Hecht, J. L. et al. Histological characteristics of singleton placentas delivered before the 28th week of gestation. Pathology 40, 372–376 (2008).
Hecht, J. L. et al. Characterization of chorioamnionitis in 2nd-trimester C-section placentas and correlation with microorganism recovery from subamniotic tissues. Pediatr. Dev. Pathol. 11, 15–22 (2008).
Tilley, S. K. et al. Genomic biomarkers of prenatal intrauterine inflammation in umbilical cord tissue predict later life neurological outcomes. PLoS ONE 12, e0176953 (2017).
Tilley, S. K. et al. Placental CpG methylation of infants born extremely preterm predicts cognitive impairment later in life. PLoS ONE 13, e0193271 (2018).
Martin, E. et al. Sexual epigenetic dimorphism in the human placenta: implications for susceptibility during the prenatal period. Epigenomics 9, 267–278 (2017).
Meakin, C. J. et al. Placental CpG methylation of HPA-axis genes is associated with cognitive impairment at age 10 among children born extremely preterm. Horm. Behav. 101, 29–35 (2018).
Santos, H. P. Jr. et al. Evidence for the placenta-brain axis: multi-omic kernel aggregation predicts intellectual and social impairment in children born extremely preterm. Mol. Autism 11, 97 (2020).
Santos, H. P. Jr. et al. Epigenome-wide DNA methylation in placentas from preterm infants: association with maternal socioeconomic status. Epigenetics 14, 751–765 (2019).
Tomlinson, M. S. et al. Microorganisms in the human placenta are associated with altered CpG methylation of immune and inflammation-related genes. PLoS ONE 12, e0188664 (2017).
Tomlinson, M. S. et al. Microorganisms in the placenta: links to early-life inflammation and neurodevelopment in children. Clin. Microbiol. Rev. 32, e00103–e00118 (2019).
Bulka, C. M. et al. Placental CpG methylation of inflammation, angiogenic, and neurotrophic genes and retinopathy of prematurity. Invest. Ophthalmol. Vis. Sci. 60, 2888–2894 (2019).
Wood, C. T. et al. Antecedents of obesity among children born extremely preterm. Pediatrics 142, e20180519 (2018).
Linthavong, O. et al. Neurocognitive and health correlates of overweight and obesity among ten-year-old children born extremely preterm. J. Pediatr. 200, 84.e4–90.e4 (2018).
Bangma, J. T. et al. Assessing positive child health among individuals born extremely preterm. J. Pediatr. 202, 44.e4–49.e4 (2018).
Nobile, S., Di Sipio Morgia, C. & Vento, G. Perinatal origins of adult disease and opportunities for health promotion: a narrative review. J. Personal. Med. 12, 157 (2022).
Kobayashi, Y. Developmental origins of metaflammation; a bridge to the future between the DOHaD theory and evolutionary biology. Front. Endocrinol. 13, 839436 (2022).
Tomlinson, M. S. et al. Neurocognitive and social-communicative function of children born very preterm at 10 years of age: associations with microorganisms recovered from the placenta parenchyma. J. Perinatol. 40, 306–315 (2020).
Leviton, A., Allred, E. N., Yamamoto, H. & Fichorova, R. N. Relationships among the concentrations of 25 inflammation-associated proteins during the first postnatal weeks in the blood of infants born before the 28th week of gestation. Cytokine 57, 182–190 (2012).
Leviton, A. et al. Inflammation-related proteins in the blood of extremely low gestational age newborns. The contribution of inflammation to the appearance of developmental regulation. Cytokine 53, 66–73 (2011).
Stroustrup, A., Teitelbaum, S. L. & Aschner, J. L. The value of preterm infant environmental health cohorts: the canary in the coal mine. JAMA Pediatr. 171, 1139–1140 (2017).
Martinez, A., de la Rosa, R., Mujahid, M. & Thakur, N. Structural racism and its pathways to asthma and atopic dermatitis. J. Allergy Clin. Immunol. 148, 1112–1120 (2021).
Newsome, F. A., Gravlee, C. C. & Cardel, M. I. Systemic and environmental contributors to obesity inequities in marginalized racial and ethnic groups. Nurs. Clin. North Am. 56, 619–634 (2021).
Culhane, J. F. & Goldenberg, R. L. Racial disparities in preterm birth. Semin. Perinatol. 35, 234–239 (2011).
Burris, H. H. & Hacker, M. R. Birth outcome racial disparities: a result of intersecting social and environmental factors. Semin. Perinatol. 41, 360–366 (2017).
Burris, H. H. et al. The promise and pitfalls of precision medicine to resolve black-white racial disparities in preterm birth. Pediatr. Res. 87, 221–226 (2020).
Li, X. et al. Association between ambient fine particulate matter and preterm birth or term low birth weight: An updated systematic review and meta-analysis. Environ. Pollut. 227, 596–605 (2017).
Stieb, D. M., Chen, L., Eshoul, M. & Judek, S. Ambient air pollution, birth weight and preterm birth: a systematic review and meta-analysis. Environ. Res. 117, 100–111 (2012).
Jelliffe-Pawlowski, L. L., Miles, S. Q., Courtney, J. G., Materna, B. & Charlton, V. Effect of magnitude and timing of maternal pregnancy blood lead (Pb) levels on birth outcomes. J. Perinatol. 26, 154–162 (2006).
Collins, J. W. Jr, David, R. J., Handler, A., Wall, S. & Andes, S. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. Am. J. Public Health 94, 2132–2138 (2004).
Messer, L. C., Kaufman, J. S., Dole, N., Herring, A. & Laraia, B. A. Violent crime exposure classification and adverse birth outcomes: a geographically-defined cohort study. Int. J. Health Geogr. 5, 22 (2006).
Mustillo, S. et al. Self-reported experiences of racial discrimination and Black-White differences in preterm and low-birthweight deliveries: the CARDIA Study. Am. J. Public Health 94, 2125–2131 (2004).
Burris, H. H. et al. Racial disparities in preterm birth in USA: a biosensor of physical and social environmental exposures. Arch. Dis. Child. 104, 931–935 (2019).
Vohr, B. R., Poggi Davis, E., Wanke, C. A. & Krebs, N. F. Neurodevelopment: the impact of nutrition and inflammation during preconception and pregnancy in low-resource settings. Pediatrics 139, S38–S49 (2017).
Couto, P. F., Goto, J. B. & Bastos, J. L. Blood pressure and interpersonal discrimination: systematic review of epidemiologic studies. Arq. Bras. Cardiol. 99, 956–963 (2012).
Beck, A. F. et al. The color of health: how racism, segregation, and inequality affect the health and well-being of preterm infants and their families. Pediatr. Res. 87, 227–234 (2020).
Sigurdson, K., Morton, C., Mitchell, B. & Profit, J. Disparities in NICU quality of care: a qualitative study of family and clinician accounts. J. Perinatol. 38, 600–607 (2018).
Sigurdson, K. et al. Racial/ethnic disparities in neonatal intensive care: a systematic review. Pediatrics 144, e20183114 (2019).
Horbar, J. D. et al. Racial segregation and inequality in the neonatal intensive care unit for very low-birth-weight and very preterm infants. JAMA Pediatr. 173, 455–461 (2019).
Profit, J. et al. Racial/ethnic disparity in NICU quality of care delivery. Pediatrics 140, e20170918 (2017).
Howell, E. A. et al. Double disadvantage in delivery hospital for Black and Hispanic women and high-risk infants. Matern. Child Health J. 24, 687–693 (2020).
Padula, A. M. et al. Multilevel social factors and NICU quality of care in California. J. Perinatol. 41, 404–412 (2021).
Lake, E. T. et al. Disparities in perinatal quality outcomes for very low birth weight infants in neonatal intensive care. Health Serv. Res. 50, 374–397 (2015).
Janevic, T. et al. Association of race/ethnicity with very preterm neonatal morbidities. JAMA Pediatr. 172, 1061–1069 (2018).
Howell, E. A. et al. Differences in morbidity and mortality rates in Black, White, and Hispanic very preterm infants among New York City hospitals. JAMA Pediatr. 172, 269–277 (2018).
Janevic, T. et al. Racial and economic neighborhood segregation, site of delivery, and morbidity and mortality in neonates born very preterm. J. Pediatr. 235, 116–123 (2021).
Mage, D. T., Maria Donner, E. & Holmes, L. Risk differences in disease-specific infant mortality between Black and White US children, 1968–2015: an epidemiologic investigation. J. Racial Ethn. Health Dispar. 6, 86–93 (2019).
Liu, J., Sakarovitch, C., Sigurdson, K., Lee, H. C. & Profit, J. Disparities in health care-associated infections in the NICU. Am. J. Perinatol. 37, 166–173 (2020).
Lakshmanan, A. et al. Viewpoints from families for improving transition from NICU-to-home for infants with medical complexity at a safety net hospital: a qualitative study. BMC Pediatr. 19, 223 (2019).
Harmon, S. L., Conaway, M., Sinkin, R. A. & Blackman, J. A. Factors associated with neonatal intensive care follow-up appointment compliance. Clin. Pediatr. 52, 389–396 (2013).
Saatci, D. et al. Association between race and COVID-19 outcomes among 2.6 million children in England. JAMA Pediatr. 175, 928–938 (2021).
Dennis-Heyward, E. A. Disparities in susceptibility to multisystem inflammatory syndrome in children. JAMA Pediatr. 175, 892–893 (2021).
Dennis-Heyward, E. A. & Shah, S. N. Pediatric COVID-19 disparities and prioritizing equity-children are not spared. JAMA Pediatr. 175, 898–900 (2021).
Dooley, D. G., Bandealy, A. & Tschudy, M. M. Low-income children and coronavirus disease 2019 (COVID-19) in the US. JAMA Pediatr. 174, 922–923 (2020).
Forrest, C. B., Blackwell, C. K. & Camargo, C. A. Jr Advancing the science of children’s positive health in the National Institutes of Health Environmental Influences on Child Health Outcomes (ECHO) research program. J. Pediatr. 196, 298–300 (2018).
Mesman, E., Vreeker, A. & Hillegers, M. Resilience and mental health in children and adolescents: an update of the recent literature and future directions. Curr. Opin. Psychiatry 34, 586–592 (2021).
Askeland, K. G. et al. Life events and adolescent depressive symptoms: protective factors associated with resilience. PLoS ONE 15, e0234109 (2020).
Taylor, H. G., Minich, N., Schluchter, M., Espy, K. A. & Klein, N. Resilience in extremely preterm/extremely low birth weight kindergarten children. J. Int. Neuropsychol. Soc. 25, 362–374 (2019).
Bangma, J. T. et al. Early life antecedents of positive child health among 10-year-old children born extremely preterm. Pediatr. Res. 86, 758–765 (2019).
Bradley, R. H. Children’s home environments, health, behavior, and intervention efforts: a review using the HOME inventory as a marker measure. Genet. Soc. Gen. Psychol. Monogr. 119, 437–490 (1993).
Leviton, A. et al. Socioeconomic status and early blood concentrations of inflammation-related and neurotrophic proteins among extremely preterm newborns. PLoS ONE 14, e0214154 (2019).
Fichorova, R. N. et al. Maternal microbe-specific modulation of inflammatory response in extremely low-gestational-age newborns. Mbio 2, e00280-00210 (2011).
van der Burg, J. W. et al. Is maternal obesity associated with sustained inflammation in extremely low gestational age newborns? Early Hum. Dev. 89, 949–955 (2013).
Allred, E. N. et al. Systemic inflammation during the first postnatal month and the risk of attention deficit hyperactivity disorder characteristics among 10 year-old children born extremely preterm. J. Neuroimmune Pharmacol. 12, 531–543 (2017).
Aris, I. M., Kleinman, K. P., Belfort, M. B., Kaimal, A. & Oken, E. A 2017 US reference for singleton birth weight percentiles using obstetric estimates of gestation. Pediatrics 144, e20190076 (2019).
Acknowledgements
We wish to thank our ECHO colleagues, the medical, nursing and program staff, as well as the children and families participating in the ECHO cohorts. We also acknowledge the contribution of the following ECHO program collaborators: ECHO Coordinating Center: Duke Clinical Research Institute, Durham, North Carolina: Smith PB, Newby KL. ECHO Data Analysis Center: Johns Hopkins University Bloomberg School of Public Health, Baltimore, MD: Jacobson LP; Research Triangle Institute, Durham, NC: Parker CB.
Funding
Research reported in this publication was supported by the Environmental influences on Child Health Outcomes (ECHO) program, Office of The Director, National Institutes of Health, under Award Numbers U2COD023375 (Coordinating Center), U24OD023382 (Data Analysis Center), U24OD023319 (PRO Core), UH3OD023320 (J.L.A.), UH3OD023347 (B.L.), and 5UH3OD023349-06 (T.M.O./R.C.F.).
Author information
Authors and Affiliations
Consortia
Contributions
T.M.O. conceptualized and designed the study, obtained funding for the study, drafted the initial manuscript, and reviewed and revised the manuscript. M.M. conceptualized and designed the study, obtained funding for the study, analyzed data, and reviewed and revised the manuscript. J.L.A., B.L., and R.C.F. conceptualized and designed the study, obtained funding for the study, and reviewed and revised the manuscript. H.P.S., C.M., A.S., C.E., M.H., E.M., and S.P. conceptualized and designed the study and reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Patient consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
O’Shea, T.M., McGrath, M., Aschner, J.L. et al. Environmental influences on child health outcomes: cohorts of individuals born very preterm. Pediatr Res 93, 1161–1176 (2023). https://doi.org/10.1038/s41390-022-02230-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02230-5