Abstract
Aim
Genetic variants contribute to the pathogenesis of bronchopulmonary dysplasia (BPD). The aim of this study is to evaluate the association of 45 SNPs with BPD susceptibility in a Turkish premature infant cohort.
Methods
Infants with gestational age <32 weeks were included. Patients were divided into BPD or no-BPD groups according to oxygen need at 28 days of life, and stratified according to the severity of BPD. We genotyped 45 SNPs, previously identified as BPD risk factors, in 192 infants.
Results
A total of eight SNPs were associated with BPD risk at allele level, two of which (rs4883955 on KLF12 and rs9953270 on CHST9) were also associated at the genotype level. Functional relationship maps suggested an interaction between five of these genes, converging on WNT5A, a member of the WNT pathway known to be implicated in BPD pathogenesis. Dysfunctional CHST9 and KLF12 variants may contribute to BPD pathogenesis through an interaction with WNT5A.
Conclusions
We suggest investigating the role of SNPs on different genes which are in relation with the Wnt pathway in BPD pathogenesis. We identified eight SNPs as risk factors for BPD in this study. In-silico functional maps show an interaction of the genes harboring these SNPs with the WNT pathway, supporting its role in BPD pathogenesis.
Trial registration
NCT03467828.
Impact
-
It is known that genetic factors may contribute to the development of BPD in preterm infants. Further studies are required to identify specific genes that play a role in the BPD pathway to evaluate them as a target for therapeutic interventions.
-
Our study shows an association of BPD predisposition with certain polymorphisms on MBL2, NFKBIA, CEP170, MAGI2, and VEGFA genes at allele level and polymorphisms on CHST9 and KLF12 genes at both allele and genotype level.
-
In-silico functional mapping shows a functional relationship of these five genes with WNT5A, suggesting that Wnt pathway disruption may play a role in BPD pathogenesis.
Similar content being viewed by others
Introduction
Despite recent advances in neonatal intensive care, bronchopulmonary dysplasia (BPD) remains one of the most common cause of neonatal morbidity and mortality, due to the increasing survival of extremely low birth weight (ELBW) infants.1,2 Birth weight and gestational age are the most important risk factors.3,4 In addition, several maternal, perinatal, and postnatal factors including race, sex, infections, altered microbiome, mechanical ventilation, and oxygen injury all contribute to the complex pathogenesis of BPD.2,5
Although approximately 40% of ELBW infants develop BPD, the reported incidence varies widely between centers, not only as a consequence of definition criteria and clinical care practices, but also possibly reflecting innate differences in the populations studied.3,4 In recent years, genetic susceptibility was increasingly recognized as a contributing factor for BPD development in premature infants. In a premature twin cohort study, genetic factors were estimated to account for 53% variance in BPD.6 BPD development and severity are closely associated with both common and rare variants involving a vast array of genes, and outcomes are influenced by complex genetic and environmental interactions.2,7 Rare variants are often unique, thus offering little diagnostic value, but inform on significant genes and pathways. In recent years, genome-wide association studies (GWAS) attempting to determine BPD candidate genes through the identification of common and rare deleterious variants in several preterm infant cohorts showed associations of certain single nucleotide polymorphisms (SNP) on genes such as ACE, MBL2, NFKBIA, TNF, VEGFA, SPOCK-2, and TLR10 with BPD development,8,9,10,11,12,13,14,15 but yielded inconsistent results, with some studies reporting no significant association with any SNP.15,16 The majority of these variants were related to lung development, drug metabolism, and immune response.15 A recent whole-exome sequencing (WES) study in a cohort of 85 infants with extreme severe respiratory phenotypes17 revealed both rare and common variants of 292 genes, 19 of which replicated the findings of a previous WES study,18 and the relation between BPD and various key signaling pathways like gonadotropin and corticotropin-releasing hormones (lung maturation), PKA-cAMP (respiratory epithelial cell differentiation), cardiovascular hypertrophy (cardiac or pulmonary vascular dysfunction) and EGFR/Neuregulin (surfactant, BPD phenotype) were emphasized.
In this study, we sought to validate the correlation between previously identified common allelic variants (SNPs) in 45 selected sites associated with BPD in a Turkish cohort of very premature infants. We then performed bioinformatics pathway analysis in order to explore the potential relationships and pathways involved between the affected genes.
Material and methods
Study design
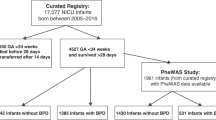
We designed a prospective cohort study comparing the prevalence of selected SNPs between subjects with and without BPD. The study population consisted of 192 infants hospitalized in Kanuni Sultan Suleyman Training and Research Hospital, Neonatal Intensive Care Unit between December, 2016 and March, 2018. Infants born under 32 weeks of gestational age were eligible, excluding those with major congenital anomalies and/or whose parents declined to participating were excluded. Survivors were evaluated for BPD at 28 days of age based on oxygen requirement >21% and divided into two groups (BPD, no-BPD) on a 1-to-1 ratio after obtaining parental consent. The study was planned based on an estimated sample size of 194 subjects (assuming a 20% difference between groups, alpha 0.05, beta 0.2). BPD patients were subsequently stratified into three groups of severity (mild, moderate, severe) based on supplemental oxygen levels and need for mechanical ventilatory support at 36-weeks postmenstrual age according to the 2001 National Institute of Child Health and Human Development (NICHD) consensus statement.19 During the study period, standardized protocols based on both European20 and Turkish21 guidelines were followed for antenatal, delivery room, and NICU care by the same team for all study population. Peripheral blood samples were collected by one investigator after enrollment. The study received the approval of the Ethics Committee of Kanuni Sultan Suleyman Training and Research Hospital (KAEK/2016.12.31).
Selection of relevant SNPs
We performed an extended review of the literature through PubMed and found a number of reported associations with surfactant proteins, lung and vascular development genes, adhesion molecules, antioxidant enzymes, inflammation-related genes, and matrix modeling proteins in different populations. We selected 45 SNPs based on a systematic review of adequately powered genomic studies reporting significant associations with BPD.8,9,10,11,12,13,14,15,16,22,23,24,25,26 These SNPs are located on genes related to oxidases, destruction of free superoxide radicals, zinc-finger proteins, calcium and mannose-binding proteins, certain growth factors, interleukins, inflammation response, and embryonic development. Physical positions, chromosomal locations, gene and allele information are provided in Table 1.
Experimental methods
All methods used in this study were carried out according to iPLEX® Gold Application Guide27 and MassARRAY® Assay Design 3.1 Software Guide28 (Sequenom Inc., San Diego, CA) unless otherwise specified. QIAamp DNA Mini Kit (Qiagen GmbH, Dusseldorf, Germany) was used to isolate leukocyte DNA; HotStarTaq plus DNA polymerase, PCR buffer, and MgCl2 solutions used in PCR were obtained from Qiagen, dNTP solution from Applied Biosystems, Inc (Foster City, CA). Shrimp alkaline phosphatase (SAP) enzyme and enzyme buffer solution, iPLEX enzyme, iPLEX buffer solution, and iPLEX Extension Mix used in single base extension (SBE) reactions, SpectroClean Resin solution, and primers for PCR were obtained from Agena Bioscience GmbH, Hamburg, Germany. DNA isolation was performed according to the manufacturer’s instructions.29 DNA concentrations were measured for each DNA sample by spectrophotometry. All DNA samples had an A260/A280 ratio between 1.7 and 2.0 and concentrations higher than 10 ng/µl by 260/280 nm spectrophotometry,30,31 hence were included in further analyses.
Primer and probe design
Positions of primers and extension probes on the genome sequence were determined by Agena Biosciences, Assay Suite bioinformatics software. Amplification primers were designed to include the polymorphic site as a multiplex PCR product and produce an 80–120 bp length amplicon. A label of 10 nucleotides (5′-ACGTTGGATG-3′) was added to the 5′ end of amplification primers. Extension probes were designed to have a different mass than amplification primers to avoid any confusion in the spectrum. Extension primers were designed to be 15–20 nucleotides long, with a Tm value of ≥60 °C, and able to anneal right next to the SNP site from its 3′ end (Table 2). All forward and reverse custom-designed primers and probes were manufactured by Agena GmbH.
Multiplex PCR
We used MassARRAY® Multiplex PCR (Agena GmbH) for the amplification of target SNP sites, and Matrix-assisted laser desorption/ionization-time of flight mass spectrometry (MALDI-TOF MS) fingerprinting method for genotyping SNPs, as accurate, rapid, and cost-effective for genotyping SNPs by multiplex assays in a single procedure. In brief, following the first PCR, SAP enzyme was used to neutralize dNTPs which were not bonded to the amplification products, by cutting the free phosphate group from dNTPs and turning them permanently into dNDPs as published. The PCR products were then hybridized with extension primers specifically designed for each SNP, and mass-modified SBE reaction was performed. SBE reaction products were then treated with resin to remove Na+, K+, and Mg2+ ions in order to reduce the background noise, and PCR products were transferred to 384-element SpectroCHIP® II by using a nanodispenser and was uploaded to the mass spectrometer (MassARRAY® Analyser 4, Agena GmbH) for analysis.32 MassARRAY® Type 4.0 genotyping software was used to analyze data, obtain allele-specific peaks and spectrum images.27
Genotyping
The spectrum image of the rs755622 polymorphism is provided as an example in Fig. 1. The molecular weight (MW) of the extension primer designed for this polymorphism is 4964.3 Da. It is known that the C or G alleles added to this sequence with the iPLEX reaction increase the nucleotide MW to 5210.8 and 5250.5 Da, respectively. These three MW values are identified as A, B, and C peaks; the “A” peak corresponding to unexpanded primers (UEP) with a MW of 4964.3 Da, the “B” peak corresponding to the 5210.8 Da sequence of the C-extended allele, and the “C” peak corresponding to the 5250.5 Da sequence of the G-extended allele.
Statistical analysis
All statistical analyses were performed using SPSS software (Statistical Packages of Social Sciences, SPSS for Windows, Version 20.0, Chicago, IL). Results with OR > 1 and p ≤ 0.05 were considered statistically significant. Chi-squared tests, performed to compare observed vs. expected genotype frequencies for deviations from Hardy–Weinberg Equilibrium (HWE), showed that the control and BPD study groups were statistically in balance for 38 out of the 45 selected SNPs (p > 0.05), while deviating from HWE for seven (rs1049269, rs1966265, rs3771171, rs650950, rs72791417, rs769217, and rs8192287), which were excluded from subsequent analyses.
The major allele in the control group was referred to as the wild-type allele. Odds ratios (OR) of a minor (presumably pathogenic) vs. major alleles were calculated with a 95% confidence interval (CI). Associations between genotypes and BPD were determined in comparison with the prevalent genotype in the control group using both homozygote (e.g., AA vs. CC) and dominant (e.g., AA + AC vs. CC) comparison models. Sample size determination using the one-sided McNemar’s test resulted in 192 individuals (96 in each arm) with 80% power and a 0.05 level of significance. Clinical data were reported by number and percentage of cases.
Functional relationship analysis
We generated functional relationship webs of the genes carrying the most significant BPD-associated SNPs at the allelic plus/minus genotypic levels in this cohort using an online bioinformatics tool computing various functional genomic datasets such as gene expression, cellular localization, and DNA/protein binding assays (PathwayNet, Troyanskaya Lab, Princeton University, Princeton, NJ).33,34 The findings were validated using a tissue-specific functional genomic network tool (HumanBase, Flatiron Institute, Simons Foundation, New York, NY).35
Results
Demographic data
After initial exclusion, postnatal demise, consent withdrawal, and technical issues, a total of 192 infants constituted the study cohort. From these, 96 infants with a diagnosis of BPD were referred as the study group, while 96 infants without BPD referred to as the control group, as shown on the cohort flow chart (Fig. 2). In the study group, 44 (46%), 34 (35%), and 18 (19%) infants had mild, moderate, and severe BPD, respectively (Table 3). The study group had significantly lower birth weight and gestational age compared with the control group (both p < 0.001) (Table 3). Duration of invasive and non-invasive mechanical ventilation and oxygen exposure was significantly higher in infants with BPD compared with the control group. There were no significant differences in terms of sex, antenatal steroid status, breastmilk feeding, neonatal morbidities, or mortality (p > 0.05).
Association of BPD predisposition and SNPs at the allele level
Eight polymorphisms (rs11003125, rs2233406, rs3138053, rs55716084, rs62468577, rs833061, rs4883955, and rs9953270) harbored in seven genes (VEGFA, CHST9, NFKBIA, CEP170, MAGI2, MBL2, and KLF12) were associated with BPD risk, since the prevalence of the risk alleles in these SNPs was statistically higher among the BPD subjects than among the no-BPD group (Table 4A).
Association of BPD predisposition and SNPs at the genotype level
Two out of 38 polymorphisms resulted associated with BPD at the genotype level. The TT genotype of rs4883955 and the CC genotype of rs9953270 polymorphisms were significantly enriched in the BPD compared to the control group [OR = 5.48 (1.48–20.33), p = 0.01 and OR = 2.71 (1.02–2.58), p = 0.04 respectively] (Table 4B). Statistical results for polymorphisms that were not found to be in an association with BPD in this study are available in the Supplementary Information.
Functional relationship of genes associated with BPD
The functional relationship map performed for VEGFA, CHST9, NFKBIA, MBL2, and KLF12 indicated direct functional interactions between four out of five of these genes (except CHST9) with weak to moderate confidence. In addition, the map revealed a novel functional convergence of these five genes on another gene, WNT5A, with moderate to strong confidence. In particular, CHST9 and KLF12, the two genes associated with BPD at both allele and genotype level, were directly and independently related with WNT5A with confidence indices of 0.34 (WNT5A-CHST9) and 0.6 (WNT5A-KLF12). The map also suggested a functional connection of four of the five BPD-associated genes within another gene, PHLDA1, although with a weaker confidence index (Fig. 3a). Tissue-specific pathway analysis focusing on the 3 genes (WNT5A, KLF12, and CHST9) in lung (Fig. 3b) and fetal tissue (Fig. 3c) confirmed the findings for the WNT5A-KLF12 (evidence 0.13 for lung and 0.06 for fetal tissue) and WNT5A-CHST9 interactions (0.06 for lung and 0.07 for fetal tissue). Due to analyzing limitation of 5 genes in PathwayNet tool, CEP170 and MAGI2 genes were excluded from the relationship web shown in Fig. 3a, as PathwayNet and HumanBase bioinformatics tools do not show any association of these genes with WNT5A.
a Functional relationships of KLF12, CHST9, VEGFA, MBL2, and NFKBIA human genes (pathwayNet, http://pathwaynet.princeton.edu). b, c Tissue-specific relationships of KLF12 and CHST9 with WNT5A in lung (b) and fetal tissue (c) (HumanBase, https://hb.flatironinstitute.org).
Discussion
BPD remains the most frequent complication of prematurity, resulting from the complex interactions of antenatal and postnatal environmental exposures with an innate background of the developing lung. BPD risk and long-term outcomes are determined by the sequential influence of maternal and fetal conditions, acute injury and repair, and healing and remodeling processes, at each step of which individual gene variation plays a key modulating role.1,36 Major risk factors for BPD include prematurity and intrauterine growth restriction. In fact, if 80% of infants born at 22–24 weeks of gestation will develop BPD, only 20% of infants born at 28 weeks will do so.1 In concordance with the literature, infants who developed BPD in our study had significantly lower gestational age and birth weight. Hyperoxia and mechanical ventilation are also recognized as other important risk factors for BPD.37 Indeed, duration of invasive or non-invasive mechanical ventilation and total oxygen exposure were significantly higher in infants with BPD in our study. Several postnatal comorbidities such as ventilator-induced lung injury, infection/sepsis, patent ductus arteriosus, and nutritional deficiencies may also influence the onset and severity of BPD. In order to minimize the impact of these variables, standard delivery room and NICU management policies have been developed for BPD prevention and treatment.38,39 Herein, in order to mitigate the confounding effect of these risk factors and limit treatment-related disease heterogeneity, strictly standardized care protocols were implemented for life support and comorbidities management in this cohort.
BPD is also, at least in part, a heritable condition. Twin studies suggested the possible role of genetic contribution on the development of BPD. Although genetic variation has been extensively studied in BPD, most studies have failed to identify rare variants consistently present in affected infants, and the strongest and most frequent associations have been found with common variants (SNPs). Several studies revealed functional mechanisms by which SNPs, located both in protein-coding and non-coding genes, affect gene transcription (mRNAs), regulation (miRNAs), splicing, stability, and post-transcriptional processes, thus contributing to the pathophysiology of various multifactorial diseases and allowing the identification of candidate genes playing a role in organ development function and homeostasis.40,41 In particular, SNPs studies in the BPD population have highlighted the importance of genes involving lung development, fibrosis, maturation, oxidative stress, inflammation, angiogenesis, or tissue injury and repair.42 In general, most of these studies focused on relatively few genes or pathways and were based on limited samples and populations (one or few centers). Most studies focusing on rare variants failed to identify a single -or a small cluster of- candidate genes associated with BPD.18 One of the first GWAS studies on BPD allowed to identify one critical gene (SPOCK2) and novel pathways including adenosine deaminase and targets of miR-219,43 but was not consistently reproduced in subsequent studies, making a call for more clinical and translational studies aimed at elucidating the role of genetics in BPD development. In another pilot study, five rare and novel candidate genes (MMP1, TLR1, NOS2, CRP, and LBP) were identified in severe BPD infants by next-generation sequencing.44 Subsequently, several other candidate rare variants were identified in two large WES studies (including FBN1, DAG1, MRPL16, POLR3A, PPP1R3A, NCAM1, SLC38A2, GABRA2, SOX6).17,18 However, connecting and integrating these data from various sources and identifying central pathophysiological pathways remains a major challenge. Our study highlights the association of variations in five genes with BPD susceptibility, in particular CHST9 and KLF12, and suggests a functional interaction of these genes with the Wnt pathway.
CHST9 gene encodes a protein that belongs to the sulfotransferase 2 family, which is located on the Golgi membrane, catalyzing the transfer of sulfate to position 4 of non-reducing N-acetylgalactosamine (GalNAc) residues in N-glycans and O-glycans.45,46 These sulfate groups on carbohydrates play essential roles in cellular interactions, signal transmission, and embryonic development as they can augment glycoprotein, glycolipids, and proteoglycan functions. In human, CHST9 is associated with acute myelogenous leukemia, schizophrenia, breast, and gastric cancer.47,48,49 It is highly expressed in the trachea and fetal lung,48,49 but no evidence of any relation between CHST9 and BPD or other lung diseases has been reported to our best knowledge.
Krüppel-like factors (KLF) belong to a family of zinc-finger transcription factors playing key roles in cellular development, metabolism, differentiation, and activation.50 Currently a total of 18 mammalian KLFs were reported to be expressed in various tissues and during periods of development.50 KLF12 induces the programmed cell death process (anoikis) by supporting the G1/S transition in the cell cycle. KLF12 silencing in mouse models leads to increased tumoral lung cell survival.51 Another KLF family member, KLF5, modulates genes regulating surfactant lipid and protein homeostasis, vasculogenesis (including VEGFa), and smooth muscle cell differentiation, and plays an important role in perinatal lung morphogenesis and function.52
The WNT gene family consists of structurally-related genes that encode intercellular signaling proteins. Canonical WNT/β-catenin signaling is essential for lung development in utero. WNT5A−/− mice die immediately after birth out of hypoxic respiratory failure, due to defective alveolar-vascular coupling and interstitium thickening.53 Fetal WNT5A inhibition is associated with abnormal branching of distal airways together with defects in capillary and distal airspace formations.54,55 WNT5A overexpression in distal lung epithelium also leads to epithelial branching defects and dilated distal airways,56 suggesting a complex balance in WNT ligands and receptors time and age-related expression patterns, and tightly regulated signal dosages leading to specific sequential effects in lung development, maturation, and regeneration.57 Intra-amniotic lipopolysaccharide exposure, an established BPD model, decreases canonical WNT signaling in the developing lung of preterm lambs, differently modulated by corticosteroids according to the timing of treatment.58 During alveologenesis, WNT signaling activation leads to Type 2 alveolar epithelial cell (AEC) proliferation whereas WNT inhibition promotes epithelial maturation and transdifferentiation of type 2 to type 1 AEC.59 WNT5A regulates branching morphogenesis during the pseudoglandular stage and promotes and AEC differentiation during lung maturation from the onset of the saccular stage.60 Increased mesenchymal WNT5A during saccular-stage hyperoxia injury leads to alveolarization impairment and septal thickening similar to a BPD phenotype.61 In postnatal life, WNT/β-catenin signaling plays a critical role in lung injury repair processes,62 as observed in chronic obstructive pulmonary disease, idiopathic pulmonary fibrosis, and asthma.54,57,63,64 Postnatal WNT5A inactivation in a conditional loss-of-function mouse model results in alveologenesis interruption resembling BPD, and WNT5A expression is decreased in human BPD lung samples.65 In summary, multiple evidences concur to demonstrate the central role of the WNT pathway in airway development, function, and disease.
Recently WNT5A emerged as a key mediator of pulmonary endothelial-pericyte interaction. WNT5A loss leads to pulmonary arterial hypertension by reducing the viability of newly formed vessels in animal and human.66 A dysregulation of WNT signaling system exists in BPD-associated-pulmonary hypertension.67 This finding may also be important as 40% of preterm infants suffering from severe BPD also suffer from BPD-associated pulmonary hypertension, with a significant contribution to morbidity and mortality.67 KLF12 and WNT5A collaborate for the regulation of metabolic processes of nitrogen compounds.33,34 Nitric oxide (NO) plays important regulatory roles in pulmonary vascular endothelium and airway epithelial functions during development and postnatally.68 Data from our group and others’ show that quantitative expression and distribution pattern of NO synthase isoforms are altered in BPD.68,69,70 Thus, we can speculate that KLF12-related disruption of the NO pathway is a potential mechanism contributing to BPD pathogenesis,68 but functional studies of KLF12 disruption fall beyond the scope of this project. To our knowledge, there are not any published data supporting the hypothesis of a KLF12 dysregulation in BPD-associated pulmonary vascular disease.
PHLDA1 encodes an evolutionarily conserved proline-histidine-rich nuclear protein with epithelial cell tumor-suppressing properties, highly expressed in the lung.71 Although transcriptomics studies have shown a mirror alteration of PHLDA1 and WNT5A in smokers and COPD patients, suggesting a functional interaction between the two genes in lung disease, no data are available in BPD to date,72 hence we opted not to focus on this gene.
In summary, the role of the WNT signaling pathway is increasingly recognized in the pathogenesis of BPD,73 and our data suggest a possible role of CHST9 and KLF12 interaction with WNT5A in this process.
Our study presents some important limitations. Several disease severity indices appear higher in our cohort than in other published studies. As a single-center cohort study, our findings may be influenced by genetic assets of the Turkish population, antenatal and perinatal management of the fetus, and pregnancy (our center is a safety-net public hospital caring for underserved population), and center-specific obstetrics and neonatology practices. Thus, more clinical studies are needed to validate our findings in different populations and environments. With our approach of testing a set of SNPs identified in other cohorts, this study may fail to identify new variants specific to our cohort. Thus, an unbiased genomic approach such as next-generation sequencing might have yielded different or broader findings. Such approach was beyond the scope of the current project but could be pursued as a next step in a broader cohort. In addition, bioinformatic genome-scale functional maps of human issues, by integrating data sets covering several thousands of experiments, may yield proofs of concept, but they should be complemented with molecular experiments in order to demonstrate these specific functional relationships, understand these complex pathway interactions in the precise context of disease, and identify molecular targets for future interventions.
In conclusion, this study conducted in a single center with standardized, evidence-based clinical practices further supports the contribution of common genetic variants in BPD susceptibility, in addition to the well-established roles of environmental factors and comorbidities.
Functional in-silico mapping of these BPD-associated genes informs on specific molecular pathways potentially relevant for pathogenesis. We highlight the functional interdependence of these genes with WNT5A, a key player in lung morphogenesis, homeostasis, and injury repair both in utero and postnatally, suggesting the implication of its pathway in the pathogenesis of BPD. This study illustrates the potential of functional relationship analysis in SNP studies in order to identify novel therapeutic targets for the prevention and cure of BPD.
A deeper analysis of Wnt pathway genetic variation in BPD should include a broader list of genes in larger cohorts from different ethnic group. Functional in-vitro or in-vivo studies may be necessary in order to validate the effect of these polymorphisms on WNT5A expression and how it affects the nitric oxide pathway in BPD patients. Moreover, as the effects of common genetic variation on outcome in various conditions affecting the neonate are increasingly emerging, genome-scale polymorphism studies are warranted in order to explore the combined effects of multiple SNPs on BPD pathogenesis.
Data availability
All authors accept that all data support their published claims and comply with field standards.
Material availability
All authors accept that all materials support their published claims and comply with field standards.
References
Thébaud, B. et al. Bronchopulmonary dysplasia. Nat. Rev. Dis. Primers 5, 78 (2019).
Sahni, M. & Bhandari, V. Recent advances in understanding and management of bronchopulmonary dysplasia. F1000Research 9, 703 (2020).
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993 to 2012. Obstet. Anesthesia Dig. 36, 76–77 (2016).
Lapcharoensap, W. et al. Hospital variation and risk factors for bronchopulmonary dysplasia in a population-based cohort. JAMA Pediatr. 169, e143676 (2015).
Thekkeveedu, R. K., Guaman, M. C. & Shivanna, B. Bronchopulmonary dysplasia: a review of pathogenesis and pathophysiology. Respir. Med. 132, 170–177 (2017).
Bhandari, V. et al. Familial and genetic susceptibility to major neonatal morbidities in preterm twins. Pediatrics 117, 1901–1906 (2006).
Leong, M. Genetic approaches to bronchopulmonary dysplasia. NeoReviews 20, e272–e279 (2019).
Hadchouel, A. et al. Identification of SPOCK2 as a susceptibility gene for bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 184, 1164–1170 (2011).
Ryckman, K. K., Dagle, J. M., Kelsey, K., Momany, A. M. & Murray, J. C. Genetic associations of surfactant protein D and angiotensin-converting enzyme with lung disease in preterm neonates. J. Perinatol. 32, 349–355 (2011).
Hilgendorff, A. et al. Association of polymorphisms in the mannose-binding lectin gene and pulmonary morbidity in preterm infants. Genes Immun. 8, 671–677 (2007).
Capoluongo, E. et al. Mannose-binding lectin polymorphisms and pulmonary outcome in premature neonates: a pilot study. Intens. Care Med. 33, 1787–1794 (2007).
Ali, S. et al. Functional genetic variation in NFKBIA and susceptibility to childhood asthma, bronchiolitis, and bronchopulmonary dysplasia. J. Immunol. 190, 3949–3958 (2013).
Mailaparambil, B. et al. Genetic and epidemiological risk factors in the development of bronchopulmonary dysplasia. Dis. Markers 29, 1–9 (2010).
Kwinta, P. et al. Genetic risk factors of bronchopulmonary dysplasia. Pediatr. Res. 64, 682–688 (2008).
Wang, H. et al. A genome-wide association study (GWAS) for bronchopulmonary dysplasia. Pediatrics 132, 290–297 (2013).
Torgerson, D. G. et al. Ancestry and genetic associations with bronchopulmonary dysplasia in preterm infants. Am. J. Physiol. 315, L858–L869 (2018).
Hamvas, A. et al. Exome sequencing identifies gene variants and networks associated with extreme respiratory outcomes following preterm birth. BMC Genet. 19, 94 (2018).
Li, J. et al. Exome sequencing of neonatal blood spots and the identification of genes implicated in bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 192, 589–596 (2015).
Jobe, A. H. & Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 163, 1723–1729 (2001).
Sweet, D. G. et al. European consensus guidelines on the management of respiratory distress syndrome - 2019 update. Neonatology 115, 432–450 (2019).
Özkan, H., Erdeve, Ö. & Kutman, H. Turkish Neonatal Society guideline on the management of respiratory distress syndrome and surfactant treatment. Turk. Pediatr. Ars. 53, S45–S54 (2018).
Giusti, B. et al. Genetic polymorphisms of antioxidant enzymes as risk factors for oxidative stress-associated complications in preterm infants. Free Radic. Res. 46, 1130–1139 (2012).
Rezvani, M. et al. Association of a FGFR-4 gene polymorphism with bronchopulmonary dysplasia and neonatal respiratory distress. Dis. Markers 35, 633–640 (2013).
Hadchouel, A. et al. Matrix metalloproteinase gene polymorphisms and bronchopulmonary dysplasia: identification of MMP16 as a new player in lung development. PLoS ONE 3, e3188 (2008).
Floros, J. et al. IL-18R1 and IL-18RAP SNPs may be associated with bronchopulmonary dysplasia in African-American infants. Pediatr. Res. 71, 107–114 (2011).
Prencipe, G. et al. A polymorphism in the macrophage migration inhibitory factor promoter is associated with bronchopulmonary dysplasia. Pediatr. Res. 69, 142–147 (2011).
Sequenom. iPLEX Gold Application Guide (Matrix, Samsung, Compact) Doc. 11555 R00, CO 060190, 108 (Sequenom Inc, San Diego, CA, 2006).
Sequenom. Massarray® Assay Design 3.4 Software Guide Doc 11546, R03 CO 060094, 122 (Sequenom Inc, San Diego, CA, 2006).
Qiagen. QIAamp DNA Mini and Blood Mini HandBook 5th edn (Qiagen, 2016).
Sambrook, J., Fritsch, E. F. & Maniatis, T. Molecular Cloning: A Laboratory Manual (Cold Spring Harbor Laboratory Press, New York, 1989).
Barbas, C. F., Burton, D. R., Scott, J. K. & Silverman, G. J. General Procedures. Appendix 3, Phage Display (Cold Spring Harbor Laboratory Press, New York, 2001).
Ellis, J. A. & Ong, B. The Massarray® System for Targeted SNP Genotyping. Methods Mol. Biol. 1492, 77–94 (2016).
Park, C. Y. et al. Tissue-aware data integration approach for the inference of pathway interactions in metazoan organisms. Bioinformatics 31, 1093–1101 (2014).
Ashburner, M. et al. Gene ontology: tool for the unification of biology. Nat. Genet. 25, 25–29 (2000).
Greene, C. S. et al. Understanding multicellular function and disease with human tissue-specific networks. Nat. Genet. 47, 569–576 (2015).
Bancalari, E. & Jain, D. Bronchopulmonary dysplasia: 50 years after the original description. Neonatology 115, 384–391 (2019).
Bonadies, L. et al. Present and future of bronchopulmonary dysplasia. J. Clin. Med. 9, 1539 (2020).
Foglia, E. E., Jensen, E. A. & Kirpalani, H. Delivery room interventions to prevent bronchopulmonary dysplasia in extremely preterm infants. J. Perinatol. Nov. 37, 1171–1179 (2017).
Principi, N., Di Pietro, G. M. & Esposito, S. Bronchopulmonary dysplasia: clinical aspects and preventive and therapeutic strategies. J. Transl. Med. 16, 36 (2018).
Ramírez-Bello, J. & Jiménez-Morales, M. Implicaciones Funcionales De Los Polimorfismos de Un Solo Nucleótido (SNP) en Genes Codificantes de Proteínas y No Codificantes en Enfermedades Multifactoriales [Functional implications of single nucleotide polymorphisms (Snps) in protein-coding and non-coding RNA genes in multifactorial diseases]. Gaceta Medica de Mexico 153, 238–250 (2017).
Lavoie, P. M. & Dubé, M. P. Genetics of bronchopulmonary dysplasia in the age of genomics. Curr. Opin. Pediatr. 22, 134–138 (2010).
Lal, C. V., Bhandari, V. & Ambalavanan, N. Genomics, microbiomics, proteomics, and metabolomics in bronchopulmonary dysplasia. Semin. Perinatol. 42, 425–431 (2018).
Lal, C. V. & Ambalavanan, N. Genetic predisposition to bronchopulmonary dysplasia. Semin. Perinatol. 39, 584–591 (2015).
Carrera, P. et al. Exome sequencing and pathway analysis for identification of genetic variability relevant for bronchopulmonary dysplasia (BPD) in preterm newborns: a pilot study. Clin. Chim. Acta 451, 39–45 (2015).
Hiraoka, N., Misra, A., Belot, F., Hindsgaul, O. & Fukuda, M. Molecular cloning and expression of two distinct human N-acetylgalactosamine 4-O-sulfotransferases that transfer sulfate to Galnac 1 4glcnac 1 R in both N- and O-glycans. Glycobiology 11, 495–504 (2001).
Kang, H. G., Evers, M. R., Xia, G., Baenziger, J. U. & Schachner, M. Molecular cloning and expression of an N-acetylgalactosamine-4-O-sulfotransferase that transfers sulfate to terminal and non-terminal β1,4-linkedN-acetylgalactosamine. J. Biol. Chem. 276, 10861–10869 (2001).
Walter, M. J. et al. Acquired copy number alterations in adult acute myeloid leukemia genomes. Proc. Natl Acad. Sci. USA 106, 12950–12955 (2009).
Chen, J. et al. A frameshift variant in the CHST9 gene identified by family-based whole genome sequencing is associated with schizophrenia in Chinese population. Sci. Rep. 9, 12717 (2019).
Yuan, J. et al. CHST9 rs1436904 genetic variant contributes to prognosis of triple-negative breast cancer. Sci. Rep. 7, 11802 (2017).
Sweet, D. R., Fan, L., Hsieh, P. N. & Jain, M. K. Krüppel-like factors in vascular inflammation: mechanistic insights and therapeutic potential. Front. Cardiovasc. Med. 5, 6 (2018).
Godin-Heymann, N. et al. Tumour-suppression function of KLF12 through regulation of anoikis. Oncogene 35, 3324–3334 (2015).
Wan, H. et al. Kruppel-like factor 5 is required for perinatal lung morphogenesis and function. Development 135, 2563–2572 (2008).
Li, C., Xiao, J., Hormi, K., Borok, Z. & Minoo, P. Wnt5a participates in distal lung morphogenesis. Dev. Biol. 248, 68–81 (2002).
Kumawat, K. et al. TGF-β-activated kinase 1 (TAK1) signaling regulates TGF-β-induced WNT-5A expression in airway smooth muscle cells via Sp1 and β-catenin. PLoS ONE 9, e94801 (2014).
Loscertales, M., Mikels, A. J., Hu, J. K.-H., Donahoe, P. K. & Roberts, D. J. Chick pulmonary WNT5A directs airway and vascular tubulogenesis. Development 135, 1365–1376 (2008).
Li, C. et al. Wnt5a regulates Shh and Fgf10 signaling during lung development. Dev. Biol. 287, 86–97 (2005).
Raslan, A. A. & Yoon, J. K. WNT signaling in lung repair and regeneration. Mol. Cells 43, 774–783 (2020).
Kuypers, E. et al. Altered canonical wingless-Int signaling in the ovine fetal lung after exposure to intra-amniotic lipopolysaccharide and antenatal betamethasone. Pediatr. Res. 75, 281–287 (2014).
Frank, D. B. et al. Emergence of a wave of Wnt signaling that regulates lung alveologenesis by controlling epithelial self-renewal and differentiation. Cell Rep. 17, 2312–2325 (2016).
Li, C., Bellusci, S., Borok, Z. & Minoo, P. Non-canonical WNT signaling in the lung. J. Biochem. 158, 355–365 (2015).
Sucre, J. et al. Hyperoxia injury in the developing lung is mediated by mesenchymal expression of Wnt5A. Am. J. Respir. Crit. care Med. 201, 1249–1262 (2020).
Ota, C., Baarsma, H. A., Wagner, D. E., Hilgendorff, A. & Königshoff, M. Linking bronchopulmonary dysplasia to adult chronic lung diseases: role of WNT signaling. Mol. Cell. Pediatr. 3, 34 (2016).
Baarsma, H. A. et al. Correction: noncanonical WNT-5A signaling impairs endogenous lung repair in COPD. J. Exp. Med. 214, 565–565 (2017).
Vuga, L. J. et al. WNT5A is a regulator of fibroblast proliferation and resistance to apoptosis. Am. J. Respir. Cell Mol. Biol. 41, 583–589 (2009).
Li, C. et al. WNT5a-ROR signaling is essential for alveologenesis. Cells 9, 384 (2020).
Yuan, K. et al. Loss of endothelium-derived wnt5a is associated with reduced pericyte recruitment and small vessel loss in pulmonary arterial hypertension. Circulation 139, 1710–1724 (2019).
Chao, C. M. et al. Targeting bronchopulmonary dysplasia-associated pulmonary hypertension (BPD-PH): potential role of the FGF signaling pathway in the development of the pulmonary vascular system. Cells 9, 1875 (2020).
Davis, C. W. et al. Expression of nitric oxide synthases and endogenous NO metabolism in bronchopulmonary dysplasia. Pediatr. Pulmonol. 43, 703–709 (2008).
Auten, R. L. et al. Inhaled ethyl nitrite prevents hyperoxia-impaired postnatal alveolar development in newborn rats. Am. J. Respir. Crit. Care Med. 176, 291–299 (2007).
Cetinkaya, M. et al. O-213 Association of E-nos gene polymorphism in development of bronchopulmonary dysplasia. Archiv. Dis. Childhood 99, A105–A106 (2014).
Cárdenes, N. et al. Human ex vivo lung perfusion: a novel model to study human lung diseases. Sci. Rep. 11, 490 (2021).
Matsumura, K. & Ito, S. Novel biomarker genes which distinguish between smokers and chronic obstructive pulmonary disease patients with machine learning approach. BMC Pulm. Med. 20, 29 (2020).
Lingappan, K. & Savani, R. C. The Wnt signaling pathway and the development of bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 201, 1174–1176 (2020).
Acknowledgements
This study was supported by a grant from the Scientific Research Project Programme of the Yıldız Technical University with a project number of 2016-07-04-DOP02.
Author information
Authors and Affiliations
Contributions
A.A.; conceptualization, methodology, acquisition of data, formal analysis and investigation, resources, and writing—original draft preparation, S.Y.S; conceptualization, methodology, acquisition of data, and writing—original draft preparation, O.M.U.; formal analysis and investigation, and resources, A.E.; formal analysis and investigation, and resources. M.C.; conceptualization, methodology, acquisition of data, and writing—review and editing. O.D.; writing—review, editing, and providing the final version of the manuscript. D.T.-B.; conceptualization, methodology, acquisition of data, formal analysis and investigation, resources, and writing—original draft preparation, funding, and supervision.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the local Ethics Committee of Kanuni Sultan Suleyman Training and Research Hospital (KAEK/2016.12.31).
Competing interests
The authors declare no competing interests.
Consent to participate
Written and signed informed consent was taken from all parents of all included infants.
Consent for publication
All authors approve and give consent for this version to be published.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akat, A., Yilmaz Semerci, S., Ugurel, O.M. et al. Bronchopulmonary dysplasia and wnt pathway-associated single nucleotide polymorphisms. Pediatr Res 92, 888–898 (2022). https://doi.org/10.1038/s41390-021-01851-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01851-6