Abstract
Background
Ketogenic diet (KD) is widely used for drug-resistant epilepsy (DRE). The study was designed to evaluate one of the risk factors for development of renal calculi with KD.
Methods
Twenty patients with DRE on Modified Atkins diet (MAD) were subjected to full history and laboratory investigations, including microscopic urine analysis, urinary calcium after overnight fasting, and calcium/creatinine ratio, as well as pelviabdominal ultrasound. Frequency and severity of seizures assessed by Chalfont severity score were recorded. All assessment measures were repeated after 3 and 6 months of KD therapy.
Results
There were significant reductions in both frequency and severity of seizures, yet 2 patients (10%) developed renal stones after 6 months on KD. Gross hematuria was reported in 1 of those 2 patients (50%), but microscopic hematuria was detected in both patients. The urine calcium and the urine calcium/creatinine ratio were elevated in both patients having renal calculi after 6 months.
Conclusions
KD increases the risk of renal stones with hypercalciuria among the causes. We recommend initiation of prophylactic measures once KD is commenced by maximizing fluid intake and urine alkalinization with regular urinary studies including calcium/creatinine ratio and renal ultrasound for patients with symptoms.
Impact
-
KD has been increasingly used in epilepsy management and beyond. The potential side effects of such diet should be highlighted while valuing the merits.
-
KD increases the risk of renal stones because of hypercalciuria among other causes.
-
We recommend initiation of prophylactic measures once KD is commenced by maximizing fluid intake and urine alkalinization with estimation of urinary calcium/creatinine ratio and renal ultrasound in patients with relevant symptoms.
Similar content being viewed by others
Introduction
The International League Against Epilepsy proposed that drug-resistant epilepsy (DRE) be defined as the failure of adequate trials of two tolerated, appropriately chosen, and administered antiepileptic drugs (AEDs; whether as monotherapy or in combination) to achieve seizure freedom. They also recommended replacing the term “intractable” with “drug-resistant” epilepsy.1
The ketogenic diet (KD) is a well-established treatment for drug-resistant childhood epilepsy with expanding indications, especially in the neuro-metabolic field. Although the underlying mechanisms of action remain partly unclear, several mechanisms of action may exist for the KD, including the disruption of synaptic transmission, the inhibition of glycolysis, and the activation of ATP-sensitive potassium channels.2 Despite positive effects on seizure frequency, repeated studies have shown that the KD is associated with an increased prevalence of kidney stones, ranging from 3 to 6%,3 in comparison to 1 in several thousands in the general population.4 There are several reasons underlying the elevated risk of developing renal calculi in patients on KD especially the uric acid and calcium stones.5
The aim of this prospective study was to evaluate hypercalciuria as one of the risk factors for development of renal stone in children with DRE on KD.
Patients and methods
This prospective study was conducted on 20 patients diagnosed with symptomatic DRE according to the definition of Beleza.6 Their ages ranged between 12 and 60 months (mean age 31 ± 8.67 months). They were 13 males (65%) and 7 females (35%). The patients were recruited from the Pediatric Neurology Outpatient Clinic, Children’s Hospital Ain Shams University. Patients <1 year of age, patients treated with special diet (diabetes, phenylketonurea), patients with nutritional status impairments (e.g., neoplasia, chronic infection), or suffering from any systemic chronic illness or metabolic disease other than epilepsy were excluded from the study.
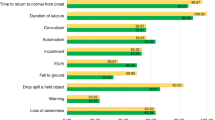
After obtaining the approval of the ethical committee at the Children’s Hospital Ain Shams University, an informed consent was obtained from each parent or caregiver. A full medical history was taken from all enrolled patients initially and repeated after 3 and 6 months of KD. Type of seizure disorder was classified according to the recommendations of the International League against Epilepsy.7 History of AEDs used and their doses, severity of the attacks (scored according to Chalfont seizure severity scale),8 and the frequency of seizure disorders were all recorded. Dietary intake data, the patient’s tolerance of the KD, any complications, family history of renal stones, fluid intake, mobility (defined as ability to crawl, sit, or walk), medications that might alter the risk of developing stones (acetazolamide, prednisone, and topiramate), history of nausea, vomiting, gross hematuria, dysuria, and flank or loin pain while on KD were all assessed.
All enrolled patients received modified Atkins diet (MAD), which consists of a nearly balanced diet (60% fat, 30% protein, and 10% carbohydrates by weight) providing adequate daily calories per body weight, without restrictions of calories, fluids, protein, or need for an inpatient fasting or admission as suggested by Kossoff and collaborators.9
For the first month, carbohydrates were restricted to 10 g/day but were permitted to increase by 5 g/day at intervals of at least 1 month if the child was having difficulty with the restriction of carbohydrates, to a maximum of 10% carbohydrates per day by weight. All patients were instructed to stop all sweets 1 week prior to initiating the diet.
Following the start of the diet, all patients were advised to remain in the hospital for 3 or 4 days to ensure adequate diet adaptation and to have their ketones in urine carefully monitored every day and glucose level monitored every 6 h. A certified dietician also educated the parents or caregivers about diet preparation at home. Multivitamins, calcium, and vitamin D were given as supplements throughout the study. The patients were requested to attend their regular monthly outpatient visits for 6 months to record their seizure frequency and severity.8 Their anthropometric measurements and the laboratory procedures were taken initially and after 3 and 6 months. All patients were kept on the same doses of AEDs throughout the study period, and the drugs were the same in all enrolled patients (valproic acid and carbamazepine in addition to clonazepam). Although changes in the pharmacokinetic and/or pharmacodynamic properties of AEDs linked to the metabolic and energetic changes caused by the KD cannot be ruled out, adjustments in the daily dose of these drugs before the start of the diet were not mandatory. The ketones were monitored daily in the urine of patients on KD (levels of +3 to 4+ were required) and twice weekly in blood (levels between 4 and 5 mmol/L of beta-hydroxybutyrate were desired to ensure effectiveness without any side effects). All parents were instructed to test the urine at home for hematuria.
The addition of KD to AEDs is generally well tolerated. Regarding gastro-intestinal tract manifestations, gastro-esophageal reflux and vomiting were present in 3 patients (15%) but improved on regular anti-emetics, H2 blocker, and fluid replacement. Five patients (25%) suffered from constipation and were advised to increase their fluid intake and decrease the constipating foods in their diet.
Considering urinary manifestations, after 6 months on KD, 3 patients (15%) suffered from loin tenderness, gross hematuria was observed in 1 patient (5%), and dysuria was detected in 3 patients (15%).
Anthropometric measurements were assessed and plotted on the growth curves. All anthropometric measurements were compared with reference values using z scores, which express the difference between the measurement of an individual and the median value of the reference population.
Laboratory procedures
Blood samples were collected in the morning following 8–12 h fasting. Five millimeters were withdrawn from each patient and then divided into two aliquots. The first one contained EDTA, which was used to perform complete blood count by Coulter GEN-S (Coulter, CA). The second part was collected in a dry tube and was centrifuged. The serum was separated and stored at −20 °C till the time of analysis. Blood sugar, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and triglycerides were assayed on the Synchron CX-9 autoanalyzer (Beckman Instruments).
Urinary samples were collected in urine bags and then in clear containers for analysis of ketones, pH, specific gravity, and gross and occult hematuria.
Gross hematuria was defined as visible bloody urine that occurred one or more times. As little as 1 mL of blood per liter can produce a visible color change; therefore, gross hematuria does not automatically indicate a large amount of blood. Microscopic hematuria was defined as the presence of ≥3 red blood cells/high-power field in 2 or 3 urine samples.10
Mission expert urinalysis reagent strips (San Diego CA92121) was used to detect urine ketones. The color change occurring on the ketone segment of the strip is compared to a color chart to obtain results.
Overnight fasting urinary calcium (uCa) and calcium/creatinine ratio were estimated for each enrolled patient in a morning urine sample initially, 3 months, and 6 months after KD.
The reference interval for uCa for spot fasting or timed specimens collected after an overnight fast is <0.16 mg/100 mL of glomerular filtrate (GF) calculated by the following equation:
uCa concentration was measured by an automated chemistry analyzer (Hitachi 704) using the Arsenazo ΙΙΙ spectrophotometric method with calcium test (Wako Pure Chemical Industries, Osaka, Japan).
Urinary creatinine was analyzed by the same chemical analyzer using the standard Jaffe kinetic reaction with picric acid (Roche Diagnostic System, Inc., Montclair, NJ).
Urinary Ca/Cr ratio (mg/mg) was calculated as uCa (mg/dL) excretion divided by urinary creatinine (mg/dL) excretion.
Hypercalciuria was defined as fasting urine calcium/creatinine ratio of >0.2 (mg/mg) for patients aged 1–5 years.
Radiological procedure
Pelviabdominal ultrasound was done to all patients at the initiation of KD, after 3 months, and after 6 months for excellent visualization of kidneys, urinary tract dilatation, stones, and nephrocalcinosis.
Statistical methodology
Data were collected in a Microsoft Excel Worksheet and was analyzed using IBM SPSS statistics (V. 17, IBM Corp., 2010). Data were expressed as mean and standard deviation for quantitative parametric measures in addition to both number and percentage for qualitative data. Comparison of different variables in various groups was performed using independent t test. Chi-square test was utilized to study the comparison between two independent groups regarding the categorized data. Paired t test was used to compare the follow-up quantitative data in the same patient. Mixed analysis of variance (ANOVA) (factorial ANOVA with repeated measure) was used to study rate of change in more than one group in repeated measured variables. The rate of change of data upon follow-up was calculated by subtracting the first recording from the second, then dividing by the first one and multiplying by 100. The probability of error at <0.05 was considered significant while <0.01 and < 0.001 were considered highly significant.
Results
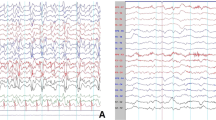
Regarding the etiology of epilepsy among the 20 enrolled patients, 20% of the enrolled patients were post anoxic, 30% were post infectious, 15% were tuberous sclerosis, and 35% were of unknown etiology. Considering the type of epilepsy, 40% had generalized epilepsy, 45% had focal epilepsy, and 15% had infantile spasm.
The clinical complications during the intake of KD diet were minimal, namely, vomiting in 10%, and constipation in 15%. What is worth noting is that all these medical complications responded to simple dietary advice and minor medications such as anti-emetics and H2 blockers. The anthropometric measurements results showed no significant difference in the z score for weight and length when the initial values were compared to those taken after 3 and 6 months. Additionally, no significant changes were detected in the lipid profile of the patients throughout the follow-up period.
After 3 months, 5 patients (25%) had reduction of frequency of seizures ≥50% and after 6 months 2 patients (10%) were seizure free, 14 patients (70%) had ≥50% reduction of seizure frequency/day, and 4 patients (20%) had reduction of seizure frequency <50%. Regarding the severity of seizure as assessed by Chalfont severity scale, after 3 months, 5 patients (25%) had reduction of severity of seizure ≥50%, and after 6 months, 7 patients (35%) had ≥50% reduction of seizure severity. There were significant reductions in frequency of seizures after 3 months (t = 2.209, p = 0.033) and after 6 months (t = 3.796, p < 0.001) among the enrolled patients. Additionally, there were significant reductions in severity of seizures after 3 months (t = 4.070, p = 0.000) and after 6 months (t = 3.600, p < 0.001).
In the current study, among the 20 enrolled patients with DRE, 2 (10%) developed renal stones after 6 months of KD therapy. None of the patients had previous history of renal stones before starting the KD. The mean age (±SD) for the patients who had no renal stones was 29.33 ± 10.27 months with a range of 12–48 months; while for the patients with renal stones mean age (±SD) was 31 ± 7.07 months with a range of 26–36 months.
For the patients who did not develop renal stones, 3 (17%) were from consanguineous parents, 2 (11%) had family history of renal stones, and 6 (33%) had previous history of using medications that increase the risk of renal stones (for example, Topiramate). Regarding the patients who developed renal stones, 1 of the 2 cases (50%) was from consanguineous parents, 1 (50%) had family history of renal stones, and none of them gave history of using medications that increase the risk of developing renal stones.
Regarding urinary complications after 6 months on KD, 2 (11%) of the patients who did not develop renal stones suffered from loin tenderness and 1 (6%) suffered from dysuria. Regarding the patients who developed renal stones, after 6 months on KD 1 (50%) of the two patients suffered from loin tenderness, both (100%) presented with dysuria, and gross hematuria was reported in only 1 (50%) (Table 1).
For the patients who did not develop renal stones, specific gravity showed normal results (1015–1025), pH was acidic in most cases, and no detected microscopic hematuria in urine upon enrollment, after 3 months, and after 6 months of KD. On the other hand, in the patients who developed renal stones, microscopic hematuria was detected in both (100%) patients after 6 months of KD, which is the time of diagnosis of renal stones (Table 2).
The urine calcium after overnight fasting was normal (<0.16 mg/100 ml GF) in the patients who did not develop renal stones upon enrollment, after 3 months, and after 6 months of KD. The patients who developed stones had normal urine calcium after overnight fasting (<0.16 mg/100 ml GF) upon enrollment and after 3 months but after 6 months the levels were high in both patients (100%) (Table 3).
The urine calcium/creatinine ratio was normal in the patients who did not develop renal stones upon enrollment, after 3 months, and after 6 months of KD. The patients who developed stones had normal urine calcium/creatinine ratio upon enrollment and after 3 months, but after 6 months the levels were high in both patients (100%) (Table 4).
For the patients who did not develop renal stones, pelviabdominal ultrasonography was normal with no detected stones throughout the study. On the other hand, in the patients who developed renal stones, the ultrasonography confirmed the diagnosis of renal stones in both patients after 6 months of KD therapy.
Discussion
The anthropometric measurements of the enrolled patients showed no significant change in mean z score of weight or length while using the KD as therapy for 6 months. Regarding the weight, this finding is in accordance with Groleau et al.,11 who studied 24 intractable epilepsy children on KD and found that weight z score was unchanged after 3 months and after 15 months. However, previous authors reported decrease in height for age z scores among their studied patients. Similar to the current work, Tagliabue and collaborators12 studied 18 children on KD prospectively for 6 months wherein they did not find any change in their weight or height. Herrero and collaborators,13 on the other hand, reported that the body mass index remained stable throughout the KD therapy for DRE due to the paralleled decline in growth in both height and weight of their studied 26 pediatric patients.
The significant reduction in seizure frequency among the enrolled patients comes in agreement with Freeman et al.,14 who used MAD with 150 intractable epilepsy children and found that, after 6 months, 98 patients (65%) showed ≥50% reduction in seizure frequency and 53 patients (35%) showed ≥90% reduction in seizure frequency. Similarly, Mirjavadi and collabrators15 treated 66 intractable epilepsy children with MAD and found that, after 3 months, 12 patients (18.2%) were seizure free, and 39 patients (59%) showed ≥50% reduction in seizure frequency. Moreover, Hallböök et al.16 evaluated the efficacy of KD in patients with DRE and 145 of them (50%) were responders (>50% seizure frequency reduction) while 47 patients (16%) were seizure-free after 6 months. El-Rashidy and collaborators17 reported that the rate of change of frequency and severity of seizures showed best improvement in classic KD patients followed by the MAD group compared to the patients on AEDs alone.
The 10% risk of developing renal stones among the enrolled patients is much higher than that reported by Furth and collaborators5 (0.8%). This discrepancy is probably multifactorial but one of the factors could be the fact that the weather is hotter in Egypt compared to the USA. Dehydration may be the most significant factor in calculus formation in children on KD, primarily because ketosis has been shown to interfere with the normal thirst mechanism3 which can be very hazardous in hot weather. Hallböök et al.16 reported kidney stones in only 7 children (2.4%), which is lower than earlier reports of 4–6% by Herzberg et al.,18 Freeman et al.,19 and Suo et al.20 This could be explained by the fact that in their protocol potassium citrate was given to most patients in this study. Interestingly, among the 123 patients who did not receive potassium citrate, 6 had kidney stones compared with 1 patient among the 167 patients who received potassium citrate. This difference was statistically significant (p value = 0.04; Fisher’s exact test). Potassium citrate increases urine pH and solubilizes calcium, thereby decreasing the concentration of free calcium available to crystallize.21 Children on KD show hypocitraturia. Citrate normally binds urine calcium, lowering its concentration, acting as an inhibitor of calcium crystallization. Acidosis induces proximal tubules to both increase citrate absorption and decrease its excretion. As a result, acidosis not only reduces urinary citrate excretion but also increases uCa excretion, aggravating renal stone formation.22
Regarding the urine pH and specific gravity of the enrolled patients, there was no difference between patients with renal stones and those who did not develop stones after 3 months and 6 months. This agrees with Furth et al.,5 who examined the risk factors for the development of stones in 112 children on KD. When the latter authors compared the 6 children who developed stones with the other 106 patients, they did not find any significant difference in the urine pH nor specific gravity after 3 months and 6 months of KD therapy. Worth noting here is that urine pH was acidic in most of the patients in the current study. The chronic acidosis persistently causes low urinary pH, which facilitates uric acid crystal formation due to lowered uric acid solubility. These crystals can act as a nidus for calcium stone formation.23
Regarding the microscopic hematuria, the two stone-forming patients were diagnosed with microscopic hematuria after 6 months on KD, which is the same time when they were diagnosed to have renal stones. This is in accordance with the study conducted by Sampath and collaborators3 in which 197 children with intractable epilepsy with a median age of 3 years were started on KD. When the previous authors compared the 13 patients with kidney stones with the 182 patients without kidney stones, they found that 92% of the stone formers had hematuria at the time of stone presentation.
Regarding urine calcium after overnight fasting, the levels were elevated in stone former patients after 6 months of KD therapy. Similarly, Sampath et al.,3 who compared 13 patients with kidney stones with 182 without kidney stones, found a trend toward higher correlation with the presence of hypercalciuria (92 vs 71% in stone and non-stone formers, respectively, p = 0.08). This could be explained by acidosis, and hypercalciuria may develop due to chronic metabolic acidosis. This metabolic acidosis not only decreases calcium reabsorption in the renal tubules, thus increasing uCa excretion, but also increases bone demineralization because bone phosphate acts as an acid buffer.5
Urine calcium-to-creatinine ratio was high in stone former patients after 6 months. Similarly, Furth et al.5 reported that there was a significant elevation in calcium/creatinine ratio in their series of patients at the time of presentation with renal stone.
Study limitations
The current study has its limitations. The small sample size and the short follow-up duration are the main limitations that should be taken into consideration in future studies.
Conclusion
From the results of the current study, we can conclude that KD is tolerable, and it is an effective adjuvant therapy for DRE. The KD can be a risk factor for kidney stones, and hypercalciuria was more common in those with kidney stones. We recommend initiation of prophylactic measures once KD is commenced by maximizing fluid intake and alkalinizing the urine to prevent the development of renal stones. Any evidence of hematuria and dysuria should be evaluated with both a renal ultrasonography and a nephrology referral. Further larger-scale studies are warranted to identify specific risk factors for renal stone formation during KD therapy, during which routine urine calcium/creatinine ratio would be plausible.
References
Kwan, P. et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 51, 1069–1077 (2010).
Lutas, A. & Yellen, G. The ketogenic diet: metabolic influences on brain excitability and epilepsy. Trends Neurosci. 36, 32–40 (2013).
Sampath, A., Kossoff, E. H., Furth, S. L., Pyzik, P. L. & Vining, E. P. Kidney stones and the ketogenic diet: risk factors and prevention. J. Child. Neurol. 22, 375–378 (2007).
Freeman, J. M., Kossoff, E. H., Freeman, J. B., & Kelly, M. T. The Ketogenic Diet: A Treatment for Children and Others with Epilepsy 4th edn (Demos Medical Publishing, 2007).
Furth, S. L. et al. Risk factors for urolithiasis in children on the ketogenic diet. Pediatr. Nephrol. 15, 125–128 (2000).
Beleza, P. Refractory epilepsy: a clinically oriented review. Eur. Neurol. 62, 65–71 (2009).
Fisher, R. S. The new classification of seizures by the International League Against Epilepsy 2017. Curr. Neurol. Neurosci. Rep. 17, 48 (2017).
Duncan, J. S. & Sander, J. W. The Chalfont Seizure Severity Scale. J. Neurol. Neurosurg. Psychiatry 54, 873–876 (1991).
Kossoff, E. H. et al. Optimal clinical management of children receiving the ketogenic diet: recommendations of the International Ketogenic Diet Study Group. Epilepsia 50, 304–317 (2009).
Bolenz, C., Schroppel, B., Eisenhardt, A., Schmitz-Drager, B. J. & Grimm, M.-O. The INVESTIGATION OF HEMAturia. Dtsch. Arztebl. Int. 115, 801–807 (2018).
Groleau, V., Schall, J. I., Stallings, V. A. & Bergqvist, C. A. Long-term impact of the ketogenic diet on growth and resting energy expenditure in children with intractable epilepsy. Dev. Med. Child. Neurol. 56, 898–904 (2014).
Tagliabue, A., Bertoli, S., Trentani, C., Borrelli, P. & Veggiotti, P. Effects of the ketogenic diet on nutritional status, resting energy expenditure, and substrate oxidation in patients with medically refractory epilepsy: a 6-month prospective observational study. Clin. Nutr. 31, 246–249 (2012).
Herrero, J. R. et al. Safety and effectiveness of the prolonged treatment of children with a ketogenic diet. Nutrients 12, 306 (2020).
Freeman, J. M. et al. A blinded, crossover study of the ketogenic diet. Epilepsia 50, 322–325 (2009).
Mirjavadi, S. A. et al. Efficacy of the ketogenic diet as a therapy for intractable epilepsy in children. Iran. J. Child. Neurol. 4, 27–36 (2010).
Hallbook, T. et al. Effectiveness of the ketogenic diet used to treat resistant childhood epilepsy in Scandinavia. Eur. J. Paediatr. Neurol. 19, 29–36 (2015).
El-Rashidy, O. F. et al. Modified Atkins diet vs classic ketogenic formula in intractable epilepsy. Acta Neurol. Scand. 128, 402–408 (2013).
Herzberg, G. Z., Fivush, B. A., Kinsman, S. L. & Gearhart, J. P. Urolithiasis associated with the ketogenic diet. J. Pediatr. 117, 743–745 (1990).
Freeman, J. M. et al. The efficacy of the ketogenic diet—1998: a prospective evaluation of intervention in 150 children. Pediatrics 102, 1358–1363 (1998).
Suo, C. et al. Efficacy and safety of the ketogenic diet in Chinese children. Seizure 22, 174–178 (2013).
McNally, M. A., Pyzik, P. L., Rubenstein, J. E., Hamdy, R. F. & Kossoff, E. H. Empiric use of oral potassium citrate reduces symptomatic kidney stone incidence with the ketogenic diet. Pediatrics 124, e300–e304 (2009).
Kielb, S., Koo, H. P., Bloom, D. A. & Faerber, G. J. Nephrolithiasis associated with the ketogenic diet. J. Urol. 164, 464 (2000).
Choi, J. N. et al. Renal stone associated with the ketogenic diet in a 5-year old girl with intractable epilepsy. Yonsei Med. J. 51, 457–459 (2010).
Author information
Authors and Affiliations
Contributions
M.F.N. substantially contributed to conception and design of the current study and analysis and interpretation of data, drafted the manuscript, revised it for important intellectual content, and prepared the final form. O.F.E.-R. contributed to the idea of the current study, contributed to acquisition of data and its interpretation, critically revised the manuscript, and approved its final form. M.H.A.-H contributed to the design of the current study, acquisition of data, and editing and revision of the manuscript and approved its final form. M.O.S. contributed to conception and design of the current study, acquisition and analysis of data, and editing and revision of the manuscript and approved its final form. All co-authors have shared this work and have approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical committee approval was obtained, and the parents or caregivers of each patient gave an informed consent before participating in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nassar, M.F., El-Rashidy, O.F., Abdelhamed, M.H. et al. Modified Atkins diet for drug-resistant epilepsy and the risk of urolithiasis. Pediatr Res 91, 149–153 (2022). https://doi.org/10.1038/s41390-021-01732-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01732-y
This article is cited by
-
Dietary weight loss strategies for kidney stone patients
World Journal of Urology (2023)