Abstract
Background
Little is known about the effects of secondhand marijuana smoke on children. We aimed to determine caregiver marijuana use prevalence and evaluate any association between secondhand marijuana smoke, childhood emergency department (ED) or urgent care (UC) visitation, and several tobacco-related illnesses: otitis media, viral respiratory infections (VRIs), and asthma exacerbations.
Methods
This study was a cross-sectional, convenience sample survey of 1500 subjects presenting to a pediatric ED. The inclusion criteria were as follows: caregivers aged 21–85 years, English- or Spanish-speaking. The exclusion criteria were as follows: children who were critically ill, medically complex, over 11 years old, or using medical marijuana.
Results
Of 1500 caregivers, 158 (10.5%) reported smoking marijuana and 294 (19.6%) reported smoking tobacco. Using negative-binomial regression, we estimated rates of reported ED/UC visits and specific illnesses among children with marijuana exposure and those with tobacco exposure, compared to unexposed children. Caregivers who used marijuana reported an increased rate of VRIs in their children (1.31 episodes/year) compared to caregivers with no marijuana use (1.04 episodes/year) (p = 0.02).
Conclusions
Our cohort did not report any difference with ED/UC visits, otitis media episodes, or asthma exacerbations, regardless of smoke exposure. However, caregivers of children with secondhand marijuana smoke exposure reported increased VRIs compared to children with no smoke exposure.
Impact
-
Approximately 10% of caregivers in our study were regular users of marijuana.
-
Prior studies have shown that secondhand tobacco smoke exposure is associated with negative health outcomes in children, including increased ED utilization and respiratory illnesses.
-
Prior studies have shown primary marijuana use is linked to negative health outcomes in adults and adolescents, including increased ED utilization and respiratory illnesses.
-
Our study reveals an association between secondhand marijuana smoke exposure and increased VRIs in children.
-
Our study did not find an association between secondhand marijuana smoke exposure and increased ED or UC visitation in children.
Similar content being viewed by others
Background
According to the most recent National Survey on Drug Use and Health, an estimated 58.8 million Americans aged 12 years or older used tobacco, and an estimated 27.7 million Americans aged 12 years or older used marijuana in the last 30 days.1 Nationally, tobacco use is declining, yet marijuana use is on the rise.1 Despite US federal status of marijuana as a Schedule 1 substance, more states are legalizing marijuana for medical and recreational use. States with legalized recreational use of marijuana tend to have the highest rates of utilization.2 Prior to Colorado legalizing the recreational use of marijuana (2012), 10.4% of the population aged 12 years or older used marijuana in the last 30 days. The most recent survey data show this percentage is now up to 17.3%.1
As mentioned in a review article by Volkow et al., people often view marijuana as a harmless pleasure,3 yet studies investigating the two substances have found marijuana smoke and tobacco smoke contain many of the same toxic chemicals and carcinogens.4 Tobacco smoke and its negative health effects on both adults and children have been extensively studied. As summarized in the latest report from the surgeon general, secondhand tobacco smoke is clearly linked to several known significant health risks, including otitis media, impaired lung function, respiratory illness, and sudden infant death syndrome.5 Secondhand tobacco smoke exposure is also associated with caregivers more frequently seeking medical care for their children, including increased emergency department (ED) visits.6
Similar to tobacco, primary marijuana use in adults has been associated with a number of negative health outcomes, including wheeze, cough, and shortness of breath.7 Primary marijuana use in adolescents has been associated with increased ED visits, with a large number related to psychiatric complaints.8 While adolescent marijuana use/exposure has been studied, marijuana’s impact on younger children has not been fully elucidated. A previous study investigating young children hospitalized with bronchiolitis found almost 50% of children exposed to tobacco also had detectable levels of secondhand marijuana,9 yet just how marijuana smoke affects children has not been studied in depth. With the rise in marijuana use by adults, the known concerning effects from primary exposure to marijuana, and the similarities of marijuana and tobacco smoke, the examination of secondhand marijuana smoke exposure, and its potential effects on child health is of substantial public health importance.
The objective of this study was to estimate the self-reported prevalence of marijuana use among caregivers in a state which has legalized marijuana for both medical and recreational use. Our secondary objectives were to determine the frequency of ED or urgent care (UC) visits and frequency of several tobacco smoke exposure-related illnesses (asthma attacks, ear infections, and viral respiratory infections (VRIs)) in the prior year among children with secondhand marijuana smoke exposure as compared to children with secondhand tobacco smoke exposure and children with neither marijuana nor tobacco smoke exposure. We aimed to find an association between secondhand marijuana smoke exposure and ED/UC visits as well as the tobacco smoke exposure-related illnesses.
Methods
Study design, setting, and subjects
This was a cross-sectional survey of a convenience sample of parents/caregivers presenting (with their children) to a tertiary care, free-standing academic children’s hospital with an annual ED volume of 70,000 patients, between December 1, 2015 and July 30, 2017. The study site was located in a state that had legalized recreational and medicinal use of marijuana several years prior to the study. Inclusion criteria were any caregiver, aged 21–85 years old, English- or Spanish-speaking, presenting to the ED with a child <12 years of age, for any chief complaint. The exclusion criteria were as follows: caregivers of critically ill children (based on triage level), medically complex children, children >11 years of age (to exclude primary marijuana use), children taking medical marijuana, or prior participation in the study. This study was approved by the institution’s Institutional Review Board.
Study procedures
Caregivers were approached for enrollment by study investigators or trained research assistants who were available from 7 a.m. until midnight every day of the week. Informed consent was obtained from all caregivers. Assent was obtained from children over the age of 7 years. Subjects were asked to fill out a survey before medical evaluation (e.g., in the waiting room) or during wait times during their ED stay. Study surveys were self-administered, available in English or Spanish, and completed by participants on a tablet computer. Responses were directly uploaded into a password-protected REDCap database and remained confidential. Tobacco/marijuana use questions were adapted from the Julius B. Richmond Center of Excellence Measurement Core.10 (For a full list of our survey questions, please refer to Appendix 1.) Variables collected in the survey included demographic data such as child age, sex, and race; caregiver age, relationship to child, income level, type of residence/housing, education level, and insurance type; caregiver use of tobacco and/or marijuana; index child medical history; number of overall ED/UC visits in the prior year; and several tobacco smoke exposure-related illnesses in the prior year. Specific marijuana use questions included type of product used (smoked, vaporized, edibles, topical, etc.), location of use (indoors vs outdoors), and frequency of use. Tobacco smoke exposure-related illnesses in question were: acute otitis media, VRIs, and asthma exacerbations: increased incidence of these entities is associated with tobacco exposure.11,12,13 Within the survey, we provided subjects with definitions of the above diseases for clarification. Otitis media episodes were defined as an illness with ear symptoms/signs along with the presence of fever. Asthma exacerbations were defined as any wheezing episode presenting to the ED requiring nebulized therapies, in a patient with a history of asthma. VRIs were defined as common cold, bronchiolitis, or a viral illness with the combination of the following symptoms: runny nose, cough, and low-grade fever.
Sample size and statistical analysis
At the time of study design, based on data from the NSDUH, 12.9% of adults (≥18 years of age) in Colorado admitted to marijuana use. Despite Colorado legalizing recreational marijuana use, we anticipated an under-reporting bias, and expected ~10% of caregivers completing the survey to identify as marijuana users. Consistent with our primary descriptive objective, we enrolled 1500 subjects to achieve a prevalence estimate with 95% confidence level (CI) of ±1.5%.
For descriptive analysis, subjects were classified into four exposure groups: marijuana only, tobacco only, both marijuana and tobacco, and neither marijuana nor tobacco (referent group). The caregiver’s response to substance use questions was used as a proxy to determine the exposure of the child. The primary interest of our study was the association of marijuana exposure/use with four outcomes during the previous 12 months: number of ED or UC visits; number of otitis media episodes; number of VRIs; and number of asthma exacerbations. Descriptive statistics were computed including means and standard deviations of continuous, normally distributed variables; medians and interquartile ranges (IQRs) for continuous, non-normally distributed variables; and frequencies and percentages for categorical variables. Differences in characteristics between the four exposure groups were compared using one-way analysis of variance or Kruskal–Wallis for continuous factors and χ2 tests for categorical factors. Relationships between marijuana and/or tobacco smoke exposures and count outcomes were modeled using negative-binomial regression, since the dispersion of counts for each outcome indicated that a Poisson regression was inappropriate.14 Zero-inflated negative-binomial regression was used to model otitis media due to the large number of zero counts for that outcome.15 Models were constructed using just marijuana and tobacco smoke exposure as predictors, and then adjusted for covariates. Potential interaction between marijuana and tobacco smoke exposure was also examined for each outcome. Model results were expressed using predicted incident rates per 12 months and 95% CIs. All analyses were performed using SAS, Version 9.4 software (SAS Institute Inc., Cary, NC).
Results
A total of 1500 caregivers completed the survey. Nine surveys were excluded because of missing data, leaving 1491 surveys available for analysis. Patients/children presenting to the ED had an overall median age of 4.0 years (mean 4.3 years), with an IQR of 1.8–6.0 (SD 3.2). Seven hundred and seventy-five (52.0%) were male (Table 1). The median age of caregivers was 32.0 years (mean 32.2 years) with an IQR of 27.0–36.0 (SD 7.5), and 1180 (80.2%) were identified as the mother. The total number of caregivers reporting regular marijuana use in any form was 167 (11.1%), with 158 of those (10.5%) indicating smoking/vaping. The nine subjects who did not smoke or vape marijuana reported using other forms such as topical products or edibles, which we determined would not expose children to any secondhand marijuana smoke. These nine subjects were therefore included in the referent, unexposed group. Seventy-eight caregivers (5.2%) reported smoking/vaping only marijuana (characterized as “smoke-only marijuana” group); 80 caregivers (5.4%) reported smoking both marijuana and tobacco (characterized as “smoke marijuana + tobacco” group); 214 caregivers (14.3%) reported smoking only tobacco (characterized as “smoke-only tobacco” group); and 1119 (75.0%) reported neither marijuana nor tobacco use (characterized as the “non-smokers” group)(referent) (Table 1). There were no differences amongst the four groups in child sex, race, or type of health insurance (Table 1).
Demographic comparisons
Differences among the exposure groups were found with child age, caregiver age, Hispanic status, caregiver education, and income level (Table 1). Children of caregivers who smoked only marijuana were the youngest (mean 3.4 years), whereas children of caregivers who smoked only tobacco were the oldest (mean 4.6 years). Caregivers who smoked only marijuana or marijuana plus tobacco were the youngest (mean 29.7 years), whereas the non-smoking caregivers were the oldest (mean 32.5 years). Of the marijuana plus tobacco group, 28.8% identified as Hispanic, compared to 52.9% of the non-smoking caregivers. With respect to education, the least educated group appeared to be the tobacco-only caregivers, with 14% reporting stopping formal education before high school. Caregivers who smoked only marijuana reported the highest percentage of college and/or graduate school education (42%). Finally, in regards to income level, the marijuana plus tobacco group had the lowest income level, with over 86% of caregivers reporting annual household income ≤$50,000, and the non-smoking caregivers reported the highest percentage of annual income >$100,000 (10.7%).
ED visitation
When we examined overall ED or UC visits (for any diagnosis), caregivers who smoked tobacco reported a statistically significant increase in the mean number of visits, 2.25 in the last 12 months, compared to caregivers with no tobacco or marijuana use, 1.96 in the last 12 months, (p = 0.049). Caregivers who used marijuana reported a rate of 2.15 visits in the last 12 months for their children, which did not reach statistical significance (p = 0.095).
When we examined ED/UC visits adjusting for covariates (household income, caregiver age, child age, Hispanic ethnicity, and caregiver education); however, there was no significant difference in the mean number of visits in the last 12 months regardless of exposure. The reported rate of ED/UC visits in the referent, unexposed group was 1.94 visits in the last 12 months. The reported rate in tobacco-exposed children was 2.14 visits (p = 0.087), and the reported rate in marijuana-exposed children was 2.21 visits in the last 12 months (p = 0.066) (Table 3).
Tobacco smoke exposure-related conditions (otitis media, VRIs, and asthma exacerbations)
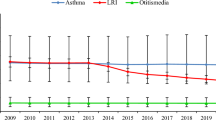
Otitis media
When we examined overall otitis media episodes, caregivers who did not use tobacco or marijuana (referent) reported a rate of 0.79 episodes in the last 12 months in their children. Caregivers who used tobacco reported a similar rate, 0.86 episodes in the last 12 months (p = 0.56). Caregivers who used marijuana reported a slightly higher rate at 1.03 episodes in the last 12 months, but this did not reach statistical significance (p = 0.14) (Table 2).
When we examined otitis media episodes, adjusting for covariates, there continued to be no significant rate difference among the groups. The referent, unexposed group, reported a rate of otitis media of 0.75 episodes in the last 12 months. The reported rate in tobacco-exposed children was 0.83 episodes (p = 0.48), and the reported rate in marijuana-exposed children was 0.96 episodes in the last 12 months (p = 0.16) (Table 3).
Viral respiratory infections
When we examined overall VRIs, caregivers who did not use tobacco or marijuana (referent) reported a rate of 1.05 infections in the last 12 months in their children. Caregivers who used tobacco reported a similar rate, 0.98 infections in the last 12 months (p = 0.35). Caregivers who used marijuana reported a statistically higher rate at 1.37 infections in the last 12 months (p = 0.01) (Table 2).
When we examined VRIs, adjusting for covariates, there continued to be a statistically significant difference among the group exposed to marijuana. The referent, unexposed group, reported a rate of 1.04 infections in the last 12 months. The reported rate in tobacco-exposed children was 1.00 infections (p = 0.65), and the reported rate in marijuana-exposed children was 1.31 infections in the last 12 months (p = 0.02) (Table 3).
Asthma exacerbations
When we examined asthma exacerbations, caregivers who did not use tobacco or marijuana (referent) reported a rate of 0.24 exacerbations in the last 12 months in their children. Caregivers who used tobacco reported a similar rate at 0.19 exacerbations in the last 12 months (p = 0.37). Caregivers who used marijuana also reported a similar rate at 0.34 exacerbations in the last 12 months (p = 0.24) (Table 2).
When we examined asthma exacerbations, adjusting for covariates, there continued to be no statistically significant difference among the groups. The referent, unexposed group, reported a rate of 0.23 exacerbations in the last 12 months in their children. The reported rate in tobacco-exposed children was 0.18 exacerbations (p = 0.31), and the reported rate in marijuana-exposed children was 0.32 in the last 12 months (p = 0.27) (Table 3).
Interaction between marijuana and tobacco smoke exposures
Regression models including a two-way interaction between marijuana and tobacco smoke were fitted for each outcome to examine potential differential or synergistic effects between them. None of those interactions were significant at the 5% alpha-level.
Discussion
We found ~11% of caregivers presenting with their children to a tertiary care children’s hospital ED reported marijuana use. Caregivers who indicated marijuana use within the survey were asked a follow-up question regarding the frequency of use. Of the marijuana users, 95% indicated daily or weekly use, which we considered regular use. Smoking/vaping was the dominant form of marijuana used. When creating exposure groups for statistical analysis, we chose to include caregivers who indicated smoking or vaping within the secondhand marijuana exposure group. We concluded that both vaping and smoking of marijuana can lead to secondhand exposure to children because studies have shown detectable environmental THC (delta-9-tetrahydrocannabinol) after vaporizer use.16
The overall percentage of caregivers who reported marijuana represented a slightly lower portion than represented in the most recent NSDUH at the time of the study (2012–2013) (12.9%), and markedly lower than the current Colorado estimate of 17.3% (of persons 12+ years of age). We also found 19.2% of caregivers admitted to tobacco use. This percentage is similar to the current NSDUH estimate of 21.4% (of persons 12+ years of age).
Our study found several differences in regards to the demographic characteristics of marijuana users vs tobacco smokers and non-smokers. Caregivers who smoked only marijuana seemed to be younger, more educated, less likely to identify as Hispanic, and had a higher income compared to non-smokers or caregivers who smoked only tobacco. Caregivers who smoked marijuana plus tobacco were also younger and less likely to identify as Hispanic compared to non-smokers, yet conversely reported the lowest income level and lower education levels. These demographic findings may help target and focus future preventative efforts and interventions.
In regard to health consequences, after controlling for potential confounders, our study found an association between secondhand marijuana smoke exposure and reported rate of VRIs. Caregivers who admitted to using marijuana reported a statistically significant higher number of VRIs in their children compared to unexposed children. We did not find an association between marijuana smoke exposure and ED/UC visitation or several other tobacco exposure-related illnesses, specifically otitis media and asthma exacerbations.
The potential for increased respiratory infections with marijuana exposure could have significant healthcare implications as more states move toward legalizing the recreational use of marijuana. While the dangers of primary marijuana use are becoming more evident,17,18,19,20 secondhand marijuana smoke exposure may also need to be addressed. Prior studies have indicated that the ED specifically is an effective setting to initiate tobacco cessation interventions.21 Thus, despite the high volume and acuity of patients, the ED may serve as an appropriate setting for initiation of marijuana smoking cessation conversations with caregivers as well.
The results of our research provide several considerations moving forward, given the associations found between secondhand marijuana exposure in children and negative health impacts. The information found in this study may be useful for healthcare providers as they initiate marijuana cessation conversations with caregivers. In addition, public health messaging regarding the potential negative implications of marijuana smoke (similar to that of secondhand tobacco smoke) could be considered. Further research is warranted to determine not only an association but also causation between secondhand marijuana smoke exposure and pediatric diseases.
Limitations
There are several limitations to our study. Our study was conducted in a tertiary care children’s hospital in a state with legalized recreational and medicinal use of marijuana. Thus, the results of our study may not be generalizable to other pediatric populations, hospitals, or states. As with all self-reporting surveys, a recall and reporting bias may have existed when reporting substance use. The under-reporting of substance use by caregivers has been shown in other studies.22 This was minimized by using anonymous, confidential surveys, in a state with legalized marijuana use. Biomarkers were not used to evaluate for systemic exposure in the subjects, and assumptions on the child’s exposure were made by caregiver report of their use. Biochemical validation of the results would have provided a more precise measure of both tobacco smoke exposure and/or marijuana smoke exposure. While similarities exist between smoked and vaped forms of marijuana, we realize that there is likely variation between their emitted chemicals and secondhand effects. The association between our study outcomes and secondhand marijuana may have been slightly different had we separated out caregivers who indicated vaping as their method of choice.
Finally, prior studies have shown an association between tobacco exposure and negative health outcomes such as increased ED visits, otitis media, VRIs, and asthma exacerbations. Our study did not show this same association. The lack of association may be related to the low number of observed events in our study population. As shown in the number of asthma exacerbations, the mean reported rate was <1 per year in all groups (Tables 2 and 3). Our study was initially powered with our primary objective in mind, evaluating the prevalence of substance use. Because of the low reported number of the tobacco smoke exposure-related conditions, we would likely need more enrolled subjects to uncover the association between tobacco smoke exposure and these conditions.
Conclusions
Approximately 10% of caregivers in a tertiary care children’s hospital ED reported regularly smoking or vaping marijuana. Children of caregivers who smoked marijuana had a higher number of reported VRIs compared to children of caregivers who did not smoke marijuana or tobacco. This study provides evidence on the potential negative health consequences from secondhand marijuana smoke exposure, impacting healthcare utilization and tobacco smoke exposure-related conditions. More studies are needed to evaluate the association with and potential causation of negative health impacts and secondhand marijuana smoke exposure in children. Future studies on the impact of other modalities of marijuana on the pediatric population would also be beneficial. Our findings can help shape preventative rules, regulations, and public health messaging to minimize the impacts of marijuana on children.
References
Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19-5068, NSDUH Series H-54) (Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/ (2019).
Center for Behavioral Health Statistics and Quality. 2015 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration, Rockville, MD. https://www.samhsa.gov/data/sites/default/files/NSDUHsaePercents2016/NSDUHsaePercents2016.pdf (2016).
Volkow, N. D., Baler, R. D., Compton, W. M. & Weiss, S. R. B. Adverse health effects of marijuana use. N. Engl. J. Med. 370, 2219–27 (2014).
Moir, D. et al. A comparison of mainstream and sidestream marijuana and tobacco cigarette smoke produced under two machine smoking conditions. Chem. Res. Toxicol. 21, 494–502 (2008).
US Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General (US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014).
Merianos, A. L., Odar Stough, C., Nabors, L. A. & Mahabee-Gittens, E. M. Tobacco smoke exposure and health-care utilization among children in the United States. Am. J. Health Promot. 32, 123–130 (2018).
Martinasek, M. P., McGrogan, J. B. & Maysonet, A. A systematic review of the respiratory effects of inhalational marijuana. Respir. Care 61, 1543–1551 (2016).
Wang, G. S., Davies, S. D., Halmo, L. S., Sass, A. & Mistry, R. D. Impact of marijuana legalization in Colorado on adolescent emergency and urgent care visits. J. Adolesc. Health 63, 239–241 (2018).
Wilson, K. M. et al. Marijuana and tobacco coexposure in hospitalized children. Pediatrics 142, e20180820 (2018).
Groner, J. A. et al. Assessing pediatric tobacco exposure using parent report: comparison with hair nicotine. J. Expo. Sci. Environ. Epidemiol. 28, 530–537 (2018).
Jones, L. L., Hassanien, A., Cook, D. G., Britton, J. & Leonardi-Bee, J. Parental smoking and the risk of middle ear disease in children: a systematic review and meta-analysis. Arch. Pediatr. Adolesc. Med. 166, 18–27 (2012).
Carroll, K. N. et al. Maternal asthma and maternal smoking are associated with increased risk of bronchiolitis during infancy. Pediatrics 119, 1104–1112 (2007).
Burke, H. et al. Prenatal and passive smoke exposure and incidence of asthma and wheeze: systematic review and meta-analysis. Pediatrics 129, 735–744 (2012).
Lawless, J. F. Negative binomial and mixed Poisson regression. Can. J. Stat. 15, 209–225 (1987).
Yau, K. K. W., Wang, K. & Lee, A. H. Zero-inflated negative binomial mixed regression modeling of over-dispersed count data with extra zeros. Biometrical J. 45, 437–452 (2003).
Sempio, C. et al. Surface detection of THC attributable to vaporizer use in the indoor environment. Sci. Rep. 9, 18587 (2019).
Roth, M. D. et al. Airway inflammation in young marijuana and tobacco smokers. Am. J. Respir. Crit. Care Med. 157(Part 1), 928–37 (1998).
Sherrill, D. L., Krzyzanowski, M., Bloom, J. W. & Lebowitz, M. D. Respiratory effects of non-tobacco cigarettes: a longitudinal study in general population. Int. J. Epidemiol. 20, 132–137 (1991).
Moore, B. A., Augustson, E. M., Moser, R. P. & Budney, A. J. Respiratory effects of marijuana and tobacco use in a U.S. sample. J. Gen. Intern. Med. 20, 33–37 (2005).
Taylor, D. R., Poulton, R., Moffitt, T. E., Ramankutty, P. & Sears, M. R. The respiratory effects of cannabis dependence in young adults. Addiction 95, 1669–1677 (2000).
Pelletier, J. H., Strout, T. D. & Baumann, M. R. A systematic review of smoking cessation interventions in the emergency setting. Am. J. Emerg. Med. 32, 713–724 (2014).
Max, W., Sung, H. Y. & Shi, Y. Who is exposed to secondhand smoke? Self-reported and serum cotinine measured exposure in the U.S., 1999-2006. Int. J. Environ. Res. Public Health 6, 1633–1648 (2009).
Author information
Authors and Affiliations
Contributions
A.B.J conceived the study, performed subject recruitment, and drafted the manuscripts. R.D.M., G.S.W., and K.W. helped design the study and performed regular review/modifications of the paper during the review process. R.D.M. oversaw the research design/methods. S.S. and V.R. served as the primary recruiters of subjects, supervised data collection, organized REDCap data, and performed the literature review. D.M.C. performed the initial statistical analysis of the data and made revisions to the study. T.E.C. performed the final statistical analysis and helped with the editing of the manuscript. A.B.J. takes responsibility for the paper as a whole.
Corresponding author
Ethics declarations
Competing interests
G.S.W. receives royalties from Uptodate for authorship contributions on related subjects. G.S.W. is now a co-investigator for an NIH NIDA funded grant. The other authors declare no competing interests.
Consent statement
Informed consent was obtained from all caregivers by trained research assistants prior to the filling out of the survey. Assent was obtained from children aged >7 years.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1 Survey Questions
Appendix 1 Survey Questions
- How many times in the last 12 months has your child been seen in the EMERGENCY ROOM or URGENT CARE Center (including the visit today)?
-How many times in the last 12 months has a healthcare provider (example: doctor, nurse practitioner, physician assistant) diagnosed your child with an EAR INFECTION?
- How many times in the last 12 months has a healthcare provider diagnosed your child with an ASTHMA ATTACK (any wheezing episode that required treatment in the Emergency Room or Urgent Care Center)?
- How many times in the last 12 months has a healthcare provider diagnosed your child with a COLD or RESPIRATORY VIRUS (an episode of runny nose, cough, and low grade fever)?
- Has your child been diagnosed with any of the following medical conditions? (Asthma, allergies, eczema)
- Is there a history of ASTHMA in either of the child’s biological parents?
-Does anyone who lives in your home, or who primarily cares for your child, use smoked TOBACCO PRODUCTS (such as CIGARETTES, CIGARS, PIPES)?
-Does anyone who lives in your home, or who primarily cares for your child, use MARIJUANA (in any form)?
-Has your child been prescribed MEDICAL MARIJUANA for an illness (example: seizures, muscle spasms, pain)?
-In which locations are SMOKED or VAPORIZED MARIJUANA products typically used?
-Has your child’s Pediatrician ever asked or counseled you about MARIJUANA?
-How many adults in your home regularly use MARIJUANA?
-Please indicate the Form and Frequency of MARIJUANA that is used? (Smoked, vaporized, edibles, highly concentrated products, topical, other)
-How old is your child?
-Gender (Sex) of your child?
-Race of your child?
-Caregiver age?
-What is your annual household income?
-What type of health insurance does your child have?
-What is your highest level of education?
-What best describes the type of residence or home in which you and your child currently live?
Rights and permissions
About this article
Cite this article
Johnson, A.B., Wang, G.S., Wilson, K. et al. Association between secondhand marijuana smoke and respiratory infections in children. Pediatr Res 91, 1769–1774 (2022). https://doi.org/10.1038/s41390-021-01641-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01641-0