Abstract
Background
Greater ventriculomegaly in preterm infants with intraventricular hemorrhage (IVH) has been associated with worse neurodevelopmental outcomes in infancy. We aim to explore the relationship between ventriculomegaly and school-age functional outcome.
Methods
Retrospective review of preterm infants with Grade III/IV IVH from 2006 to 2020. Frontal–occipital horn ratio (FOHR) was measured on imaging throughout hospitalization and last available follow-up scan. Pediatric Cerebral Performance Category (PCPC) scale was used to assess functional outcome at ≥4 years. Ordinal logistic regression was used to determine the relationship between functional outcome and FOHR at the time of Neurosurgery consult, neurosurgical intervention, and last follow-up scan while adjusting for confounders.
Results
One hundred and thirty-four infants had Grade III/IV IVH. FOHR at consult was 0.62 ± 0.12 and 0.75 ± 0.13 at first intervention (p < 0.001). On univariable analysis, maximum FOHR, FOHR at the last follow-up scan, and at Neurosurgery consult predicted worse functional outcome (p < 0.01). PVL, longer hospital admission, and gastrotomy/tracheostomy tube also predicted worse outcome (p < 0.05). PVL, maximum FOHR, and FOHR at consult remained significant on multivariable analysis (p < 0.05). Maximum FOHR of 0.61 is a fair predictor for moderate–severe impairment (AUC 75%, 95% CI: 62–87%).
Conclusions
Greater ventricular dilatation and PVL were independently associated with worse functional outcome in Grade III/IV IVH regardless of neurosurgical intervention.
Impact
-
Ventriculomegaly measured by frontal–occipital horn ratio (FOHR) and periventricular leukomalacia are independent correlates of school-age functional outcomes in preterm infants with intraventricular hemorrhage regardless of need for neurosurgical intervention.
-
These findings extend the known association between ventriculomegaly and neurodevelopmental outcomes in infancy to functional outcomes at school age.
-
FOHR is a fair predictor of school-age functional outcome, but there are likely other factors that influence functional status, which highlights the need for prospective studies to incorporate other clinical and demographic variables in predictive models.
Similar content being viewed by others
Introduction
The optimal threshold for intervention in preterm infants with post-hemorrhagic ventricular dilatation following intraventricular hemorrhage (IVH) must be weighed between the risks of surgery and potential benefits of earlier intervention. Higher grade of hemorrhage is associated with greater degree of ventricular dilatation and involvement of white matter, which have consistently been shown to be related to worse neurodevelopmental outcomes.1,2,3,4
The Early versus Late Ventricular Intervention Study (ELVIS) trial in Europe was designed to test whether initiation of cerebrospinal fluid (CSF) diversion at a lower degree of ventriculomegaly would improve outcomes. Although there was no significant difference in rates of shunting, patients in the early intervention group who were shunted had better than expected developmental outcomes at 2 years relative to those who did not require shunting.5,6 However, our recent meta-analysis showed that even the late intervention group in the ELVIS trial received intervention sooner than most published studies. Both groups in ELVIS had lower rates of shunting than previously reported, and institutions that intervened earlier had lower conversion rates to ventriculoperitoneal shunt (VPS) and lower rates of moderate–severe neurodevelopmental impairment (NDI).7
The Hydrocephalus Research Network (HCRN) agreed on a radiographic threshold of frontal–occipital horn ratio8 (FOHR) ≥0.55 for neurosurgical consultation, along with monitoring for other signs and symptoms of increasing intracranial pressure (ICP) in the decision to initiate CSF diversion.9 There is likely practice variation with varying treatment thresholds across institutions. While previous studies have shown the presence of hydrocephalus2 and degree of ventriculomegaly4,6 to correlate with worse early NDI, an independent relationship between ventriculomegaly and school-age functional outcomes has yet to be established. The aims of this study were to evaluate the relationship between ventricular size in the neonatal period as measured by FOHR throughout initial hospitalization and functional outcomes at school age and to estimate a maximum threshold of ventriculomegaly to achieve the highest potential level of function.
Methods
Patients
All infants <37 weeks gestational age (GA) admitted to the neonatal intensive care unit (NICU) at Ann and Robert H. Lurie Children’s Hospital of Chicago between 2006 and 2020 were identified through the electronic database. Our hospital is a quaternary pediatric care center. Infants are not delivered at our hospital but are transferred from other hospitals for higher level of care, often to manage problems such as severe bronchopulmonary dysplasia, necrotizing enterocolitis, or other surgical problems. Preterm infants with the diagnosis of non-traumatic IVH affecting a newborn were identified using International Classification of Disease (ICD) codes P52.* and 772.1* (ICD-9 and -10, respectively). All ultrasound (US) scans were reviewed by the first author to confirm diagnosis and grade of IVH and presence of PVL. Patients with congenital anomalies or genetic syndromes and those with intracranial hemorrhage not attributed to germinal matrix hemorrhage (i.e., identified etiologies of hemorrhagic transformation of ischemic stroke, birth trauma-related injuries, cerebrovascular malformations) were excluded. The study was approved by our institutional review board and consent was waived for retrospective review of de-identified data.
Data extraction and definition of functional outcomes
Demographic and clinical data extracted included GA, birth weight (BW), mode of delivery (vaginal or cesarean), parity (singleton or multiple), highest documented grade of hemorrhage (by Papile classification10), diagnosis of periventricular leukomalacia (PVL) as indicated on radiology report, death during initial hospitalization, and hospital length of stay (LOS). Information surrounding neurosurgical management included day of life (DOL) at initial neurosurgical consultation, DOL at first neurosurgical intervention (lumbar puncture, ventricular puncture, temporizing CSF diversion [ventricular access device or ventricular subgaleal drain], or permanent CSF shunt implantation), and DOL at conversion to permanent shunt in those who received temporizing treatment. Discharge with a gastrotomy tube (G-tube) and/or tracheostomy (trach) was noted. For those with any follow-up of at least 2 years, diagnosis of cerebral palsy (CP) was also noted.
The decision for Neurosurgery consult, timing of temporizing treatment, and conversion to permanent CSF shunt were based on the treating medical and surgical teams. There were no standardized care pathways in place in this 15-year study period. The neurosurgical staffing had no external turnover during this time. The NICU team grew from 15 to 32 faculties. The protocol adopted at our institution for head US screening for infants born at <33 weeks GA is to obtain imaging at 1 week, 1 month, and 36 weeks postmenstrual age if still hospitalized. Earlier imaging may be obtained if the infant was unstable. Older infants are screened if unstable or there is suspicion for intracranial pathology. If there is evidence of IVH, scans are repeated biweekly, weekly, or at 2-week intervals depending on severity. Typically, infants with higher-grade hemorrhages with progressive ventricular enlargement and head circumferences crossing percentile lines were those for whom Neurosurgery were consulted. Surgical management is typically initiated when there is evidence of persistent progression of ventricular enlargement and rapid increase of head circumference, along with signs and symptoms of increased ICP, including full fontanel, splayed sutures, and apnea and bradycardia events.
All preterm infants with IVH are referred to our Neonatal and Cardiac Intensive Care Unit Follow-Up Clinic for screening for developmental delay and early initiation of therapies to maximize functional outcome up to the age of 5 years. The Bayley Scales of Infant-Toddler Development—Third Edition (BSID-III, Pearson Assessments, San Antonio, TX) are performed at 6–9 and 12–18 months, with subsequent interval testing using the BSID-III based on individual indications. Children are also tested at 36 months and 5 years using the Differential Ability Scales-II and Bracken Basic Concept Scale—Third edition or Wechsler Preschool Primary Scale of Intelligence—Third Edition and Wechsler Individual Achievement Test (Pearson Assessments, San Antonio, TX). Children unable to participate in specific cognitive testing are evaluated using the BSID-III or informally by the clinic psychologist as appropriate. Rarely other assessments are performed at older ages if there is continued concern for need of supplemental education services. Additionally, the General Pediatrics, Neurology, and Neurosurgery clinic notes often document age-appropriate milestones, social concerns, educational performance, and involvement in sports and hobbies in addition to neurological examination findings. Notes from Pulmonology, Ophthalmology, Audiology, and Cardiology may also contain information about school attendance and need for supplemental school or private therapies. Social work notes documents family concerns and assistance with obtaining educational, social, or financial resources.
In our population, completion of formal testing was limited due to factors including lack of consistent follow-up and incomplete scoring. Additionally, reports for children with significant disabilities limiting testing were often descriptive and did not include scores. To capture as many children as possible and minimize selection bias, the qualitative Pediatric Cerebral Performance Category (PCPC) Scale11,12 was utilized and applied retrospectively to determine functional outcome at a minimum of 4 years (for adaptation of scale, see Supplemental Table S1). The scale is based on the Glasgow Outcome Score for adults and ranges from 1 to 6, where 1 corresponds to good functioning, 2—mild disability, 3—moderate disability, 4—severe disability, 5—vegetative state or comatose, and 6—brain death (we did not score 6). Based on these criteria, we defined each score as follows: 1—good functioning with no supplemental therapy needs or serious medical conditions (i.e., surgeries beyond what a normal child would need to undergo—i.e., tonsillectomy, tympanostomy tubes); 2—largely independent but requires assistance of individualized educational plan, on-going physical, occupational, developmental, or speech therapy, and/or has controlled medical comorbidities associated with prematurity such as feeding via a G-tube, corrected hearing or visual impairments requiring surgical correction, medically controlled seizures; 3—independent with some activities, scoring <10th percentile on milestones or educational assessments >75% of the time, requires a special education classroom due to cognitive or emotional deficits, and/or has uncontrolled medical issues such as recurrent hospitalizations due to medically uncontrolled seizures or shunt malfunction; 4—severe disability requiring significant assistance for activities of daily living, may be wheel-chair dependent, minimally verbal, and/or with significant developmental problems (i.e., severe autism), but still interactive with the environment, and 5—vegetative state where the child is completely dependent with no ability to intentionally interact and communicate.
Scoring was performed independently by two authors based on documentation available through chart review: results from available formal testing, access of educational services (private or school-based therapies whether in the mainstream classroom or special education classroom), and documented clinical (G-tube and trach dependence, controlled or uncontrolled seizures, frequency of surgeries and admissions, behavioral conditions such as attention deficient, autism, and other psychiatric disorders), and developmental–adaptive behavioral function (academic or social concerns, family relationships, and involvement in sports and other extra-curricular activities). Discrepancies between scores were resolved by a third rater.
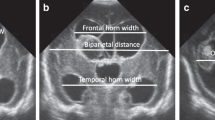
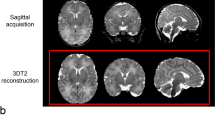
Ultrasound measurements
FOHR measurements were performed by the first author according to previously described methods.8 FOHR was measured for all cranial imaging performed during initial hospitalization of patients with Grade III and IV hemorrhages as well as those with Grade I and II for whom neurosurgery was consulted (US, computed tomography, or magnetic resonance imaging). If permanent shunting was performed after initial discharge, any intervening imaging was also assessed. FOHR was also measured on the last available follow-up scan. Since infants with Grade I and II hemorrhages without Neurosurgery consults likely did not develop any clinically significant degree of ventricular dilatation, measurements were not included from this population.
Statistical analysis
Statistical analyses were performed using R-studio Version 4.0.4 (Boston, MA). Summary statistics were reported as mean ± standard deviation and/or median (interquartile range (IQR)) for continuous variables depending on normality assessed by plotting the data on histogram. Median and IQR were reported for categorical variables. To test for overall effect of IVH grade, Fisher exact test was used for categorical variables, Kruskal–Wallis test for ordinal variables (i.e., PCPC score), and analysis of variance for continuous variables. For pair-wise comparisons, paired t test was used for continuous variables (i.e., FOHR) and Mann–Whitney U test was used for categorical and ordinal variables. For PCPC scoring, inter-rater reliability was assessed using a two-way mixed effect intra-class correlation coefficient (ICC). Two-tailed tests were used when calculating p values.
Ordinal logistic regression was used to determine the relationship between PCPC score and FOHR at the time points of interest (maximum FOHR during initial hospitalization, FOHR immediately preceding time of neurosurgical consult, time of first neurosurgical intervention, time of conversion to permanent shunt, and last follow-up scan in the system). Other variables were GA, BW, LOS, birth year, grade of IVH diagnosis of PVL, and discharge with G-tube or trach. Numeric values of IVH grade, GA, BW, LOS, and birth year were normalized between 0 and 1 prior to regression due to differences in range. We first ran univariable regression for each variable. Multiple regression was then run for each FOHR at each time of interest and confounding variables with p < 0.05 from univariable analyses. For relationships between FOHR and PCPC, only patients with Grade III/IV IVH were included. Subgroup analyses by Grade (III or IV) were also performed. p Values < 0.05 were considered significant.
Receiver operating characteristic analysis was performed to assess predictive value of maximum FOHR for moderate–severe functional impairment (PCPC≥3) using the area under the receiver operating curve (AUC) and 95% confidence interval (CI). The FOHR value that yielded highest sensitivity and specificity was calculated using Youden’s J statistic.
Results
One thousand five hundred and eighty-three preterm infants were admitted to our NICU during the study period. Three hundred and fifty-five had a diagnosis of IVH by ICD codes, of which 75 were excluded after chart review for the following reasons: 10 did not have records from the initial hospitalization, 33 did not have IVH or had some other kind of intracranial hemorrhage based on review of radiology reports and scans, and 32 had a congenital or chromosomal anomaly. Of the included 281 patients with IVH, breakdown by grade were as follows: Grade I 103 (37%), Grade II 42 (15%), Grade III 61 (22%), and Grade IV 75 (27%). See Fig. 1 for flow chart of the included and excluded patients.
Table 1 summarizes demographic and outcome variables by IVH grade. There were differences across grade for GA and BW (p < 0.001), such that patients with Grade II–IV IVH were younger and weighed less than patients with Grade I hemorrhages. Death during hospitalization was lowest for Grade I and increased as grade increased (8, 10, 16, and 31%, p < 0.001). Of the survivors, LOS did not differ between IVH grade (p = 0.881) but proportion of patients discharged with a G-tube and/or trach was higher for those with Grade II and III hemorrhages compared to those with Grade I or IV (p = 0.036). Proportion of patients with CP was highest among those with Grade IV hemorrhage (68%) compared to Grade II and III (24 and 26%, respectively), which were in turn higher than Grade I (9%) (p < 0.001).
The Neurosurgery service was consulted for 70 patients, of whom 40 had a temporizing procedure and 9 had VPS placement as a first procedure. In all, 32/281 (11%) patients required permanent shunting (Grade I 1, Grade II 1, Grade III 13, and Grade IV 17). Table 2 summarizes the course of management for these patients by grade. The two patients with Grade I/II hemorrhages requiring a shunt had meningitis prior to development of ventriculomegaly. Comparing Grade III and IV hemorrhages, the proportion of patients who underwent any neurosurgical procedure (Grade III 31% and Grade IV 25%) and permanent shunting (Grade III 22% and Grade IV 23%) did not differ (p = 0.565 and p = 1.000, respectively).
Functional outcomes
In all, 151/236 (64%) patients survived initial hospitalization and had follow-up beyond the age of 4 years: Grade I 56/96 (59%), Grade II 25/38 (66%), Grade III 37/51 (73%), and Grade IV 33/52 (63%). There was no difference in follow-up rate across grades (p = 0.443). Statistical comparison of demographic and clinical variables between patients aged ≥4 years with and without follow-up showed greater rates of follow-up for those discharged with a G-tube or trach (p < 0.001, Table 3).
Concordance in PCPC scoring between the two raters was 88.7% (ICC = 0.936, 95% CI 0.911–0.954, p < 0.001). PCPC scores differed significantly across grades (p < 0.001), where rates of moderate/severe impairment (score ≥3) increased with increasing grade: Grade I 11/56 (20%), Grade II 6/25 (28%), Grade III 13/37 (35%), and Grade IV 18/33 (55%) (Fig. 2a).
a Percentages of each PCPC score across all IVH Grades. For patients with Grade III/IV hemorrhages, PCPC scores between b those who did or did not have Neurosurgery consult and c those who did or did not require neurosurgical intervention. Scores range from 1 to 5, where 1 is good functional outcome (light gray) and 5 is vegetative state (black).
Of patients with Grade III/IV hemorrhage, 19/37 (51%) of those who received Neurosurgery consult had moderate–severe impairment (PCPC ≥3) and 12/33 (35%) of those did not have moderate–severe impairment (p = 0.236, Fig. 2b). Functional outcomes were worse in patients who received neurosurgical intervention, where 18/26 (69%) of those who had intervention had moderate–severe impairment versus 13/44 (30%) of those who did not (p = 0.002, Fig. 2c).
Patients with Grade IV hemorrhages were also more likely to be diagnosed with CP: Grade I 5/56 (9%), Grade II 6/25 (24%), Grade III 10/38 (26%), and Grade IV 23/34 (68%) (p < 0.001). Of patients with Grade III/IV hemorrhage, rates of CP did not differ based on Neurosurgery consultation: 18/36 (50%) consult versus 15/36 (42%) no consult (p = 0.637). Rates of CP were higher for those who received intervention (17/27 (63%)) versus those who did not (16/44 (36%)) (p = 0.030).
FOHR measurements
For all patients with Grade III/IV and those with Grade I/II hemorrhages with Neurosurgery consultation, mean maximum FOHR was 0.64 ± 0.16 and mean FOHR on last available scan was 0.47 ± 0.10. FOHR at the time of Neurosurgery consult was 0.62 ± 0.13, at the time of first intervention 0.76 ± 0.13, and at the time of shunt placement 0.79 ± 0.09. FOHR was significantly greater at the time of intervention than at the time of consult (p < 0.001) but not between temporizing procedure and subsequent shunting (p = 0.219). Table 2 lists mean FOHR at each stage of neurosurgery involvement by grade.
Patients with moderate–severe functional impairment (PCPC ≥3) had a mean maximum FOHR of 0.73 ± 0.15 compared to 0.59 ± 0.11 for patients with good function or mild impairment (PCPC 1 or 2) (p < 0.001). AUC was 74.07% (95% CI 62.2–86.9) for maximum FOHR as a predictor for moderate–severe impairment. The FOHR threshold with maximum sensitivity and specificity was 0.61 (67.5% specificity and 74.19 sensitivity).
Regression
On univariable regression (Table 4a), longer LOS (p = 0.18), presence of PVL, grade of hemorrhage, and G-tube/trach at time of discharge (p < 0.001) were predictive of functional outcome. Lower GA and BW showed a trend toward worse outcomes (p = 0.052 and 0.051). In terms of FOHR measurements, of Grade III/IV patients, higher maximum FOHR, FOHR at the time of consult, and FOHR on the last available scan were predictive of worse outcome (p < 0.01). For the last scan, FOHR could not be measured for two patients with Grade IV hemorrhages who required permanent shunting due to loss of typical ventricular configuration and severe anatomical abnormalities. Both of these patients had a PCPC score of 4 (severe disability). Separate subgroup analysis of patients with Grade III and Grade IV showed a trend toward significance between maximum FOHR and PCPC score for Grade III (p = 0.057) and significant relationships between maximum FOHR, FOHR at first intervention, and FOHR at latest scan for patients with Grade IV IVH (p < 0.01).
Multiple regression included FOHR, PVL, BW, LOS, and G-tube/trach as predictors. GA was not included in the model because of concerns of collinearity due to the high correlation with BW (r = 0.884, p ≤ 0.001). Of the patients with Grade III/IV IVH (Table 4b), maximum FOHR was predictive of functional outcome (p < 0.001), as well as PVL (p = 0.006). FOHR at the time of consult and latest scan were also predictive of functional outcome, as was PVL (p < 0.05). FOHR at the time of first intervention and shunt insertion was not associated with outcome but PVL remained an independent predictor of worse outcome at first intervention (p = 0.048) and showed at trend at the time of shunt (p = 0.078). Separate subgroup analysis no longer showed a significant relationship between maximum FOHR and PCPC (p = 0.14) or any of the other variables for Grade III. For Grade IV, maximum FOHR and FOHR at consult remained significant predictors of PCPC (p < 0.01) although PVL reached significance only when included in the model with FOHR at the time of consult (p = 0.041).
Discussion
We demonstrate a relationship between the degree of ventriculomegaly and functional outcomes at school age in preterm infants with severe IVH while controlling for PVL, BW, length of hospital stay, birth year, and severity of chronic medical comorbidities related to prematurity as inferred by discharge with G-tube and/or trach. The relationship was strongest between maximum FOHR and functional outcome. Higher FOHR at initial Neurosurgery consult and on last available imaging were also related to worse outcomes. On receiver operating characteristic analysis, maximum FOHR of 0.61 best predicted moderate–severe functional outcome.
We did not demonstrate statistically significant differences between FOHR at the time of first intervention and functional outcome. The raw numbers suggest worse functional status and higher FOHR at the time of first intervention. PVL remained a driving factor for poor outcomes in patients who required intervention. However, the degree of ventriculomegaly at the time of surgical intervention was already much higher (FOHR > 0.7) and patients who received CSF diversion were overall lower functioning than those who did not. Furthermore, our study was limited by the retrospective nature: the power of our statistical models was lower at each stage of escalation of care, where fewer patients received surgical intervention than those who received a Neurosurgery consultation, and fewer received a consultation than who had a diagnosis of severe IVH. Interestingly, separate subgroup analyses for Grade III and IV patients showed a stronger effect of FOHR in patients with Grade IV hemorrhage, even after controlling for PVL. It is possible that parenchymal hemorrhage, one of the defining features of Grade IV hemorrhage, amplifies effects of ventriculomegaly.
To date, ELVIS is the only randomized trial to test the effect of intervention at a lower threshold of ventricular dilatation.5,6 At 2 years of age, there was no overall difference in BSID-III scores. However, patients in the standard intervention group who were shunted did worse than those who did not require VPS while VPS placement did not affect outcome in the early intervention group. They also report higher FOHR for those with lower composite cognitive and motor scores irrespective of randomization. In a separate analysis where ventricular volume was measured, higher volumes preoperatively and postoperatively were associated with worse outcomes.1 Together their findings raise the need to question whether surgical intervention itself increases the risk of poor outcome or whether patients who have VPS placement often have more severe ventriculomegaly at institutions who wait for more severe dilatation prior to shunting.
A number of observational studies comparing outcomes between late and early intervention centers13,14 and between patients who received late/high-threshold versus early/low-threshold intervention within the same institution15,16 have also reported better outcomes in early intervention groups. Several studies demonstrated correlations between greater ventriculomegaly and worse developmental outcomes at term-equivalent age,3 12 months,17 and 18–24 months,4,18,19 although one study found no correlation between ventricular dilatation at the time of intervention and 2-year outcomes in Grade III hemorrhages.20 Our group’s recent meta-analysis showed overall less severe NDI in studies with earlier intervention7 but highlights the bias in reporting outcomes only out of patients treated, such that lower threshold or earlier intervention groups may include patients with better outcomes who may not have received intervention in a later or higher threshold group.
Our center would be considered a “high-threshold” center, with a mean FOHR at intervention of 0.77 (minimum 0.62), which is considerably higher than the HCRN recommendation of ≥0.55 for consideration of intervention.9 In comparison, mean FOHR of patients in the ELVIS trial with and without adverse outcomes were 0.49 ± 0.06 and 0.42 ± 0.04, respectively.6 Of note, only patients with Grade III or IV hemorrhages with an increasing ventricular index toward the 97th percentile were eligible for participation in ELVIS. Despite our denominator being all patients with Grade III and IV hemorrhages irrespective of the degree of ventricular dilatation, our rates of VPS were similar to those reported from ELVIS across both early and late treatment groups (29/134 [22%] for our study versus 16/126 [21%] for ELVIS). In contrast, we report higher rates of CP 30/70 (43% versus 24%) and moderate/severe outcome 32/67 (48% versus 20%). Our outcomes appear more comparable to those reported for severe preterm infants with post-hemorrhagic ventricular dilatation reported in a large US national cohort study (42.9% CP and 46% moderate/severe NDI),21 albeit their population consisted of a younger age group (mean GA 24 weeks versus our mean of 26 weeks).
While there are potential risks associated with neurosurgical intervention associated with surgery or anesthesia related and those of device infection or malfunction, potential benefits may include decreased risk of secondary brain injury from prolonged increased ICP and ventricular dilatation. Brain dysfunction in infants with ventriculomegaly has been demonstrated using cerebral near-infrared spectroscopy22,23 and electroencephalography.24 Decreases in regional cerebral oxygen saturation and amplitude suppression are associated with increased ventriculomegaly and improved after CSF diversion. There is also evidence that larger frontal–temporal horn ratio (FTHR; a measure similar to FOHR) correlates with degree of white matter injury and CP.19 Patients in the high-threshold group of the ELVIS study showed more white matter abnormalities at term-equivalent age1 while another study reported an association between greater cerebral volumes at term-equivalent age with better neurodevelopmental outcomes at 2 years.25
In our study, the relationship between GA/BW and functional outcome did not reach statistical significance as has previously been shown.2,21,26 Discharge with a G-tube and/or trach, a surrogate marker of medical complexity, was also associated with worse outcomes on univariable analysis, but these effects were no longer significant on multivariable analysis. PVL and FOHR were the only variables that remained independent predictors of outcome. It is likely that, while lower GA and BW incurs higher risk of developing IVH, once a patient has IVH, the degree of brain injury becomes more important. Indeed, PVL has consistently been associated with negative outcomes, particularly CP.20,27,28
Due to incomplete scoring of formalized assessments including the commonly cited BSID-III, we decided to use the PCPC scale,12,29 designed to assess functional outcomes after intensive care hospitalization in children and shown to be correlated with scores from the BSID Second Edition, Stanford–Binet Intelligence Scale, and Vineland Adaptive Behavior Scales29 as well as quality-of-life measures.30 The PCPC has been used to assess outcomes in children with meningitis,31 following traumatic brain injury,32 treatment of cerebral vascular malformations,30 and infants on extracorporeal cardiopulmonary resuscitation after cardiac arrest.33 We observed that children who were severely developmentally impaired or have limitations in vision, hearing, or speech often cannot complete formal assessment tasks. Higher-functioning children who no longer require therapies or supplemental school assistance also stop receiving formalized assessments but rather continue more generalized follow-up with their primary care physician. Thus, the PCPC allowed us to score children at the lower and higher extremes for which we have reasonable information regarding their overall functional status without the use for in-person formal assessments. Although we lose more nuanced information regarding specific aspects of cognitive, language, and motor function, we were still able to gauge function on a global and easily relatable scale for children who may otherwise be excluded from studies that solely report on scales such as the BSID.
Specific thresholds for when to initiate CSF diversion varies in the literature, with the HCRN adapting a threshold of FOHR ≥ 0.55 along with clinical signs and symptoms of elevated ICP,9 the ELVIS group recommending treatment at ventricular index (VI) >97th percentile and anterior horn width (AHW) >6 mm regardless of symptomatology,5 and a more recent algorithm proposing use of VI/AHW thresholds, clinical signs and symptoms, and near-infrared spectroscopy.34 The discussion regarding differences in metrics for ventriculomegaly is ongoing.35 All have good to excellent reliability8,36 and shown to correlate with ventricular volume.8,37 Optimal thresholds have been calculated to best predict white matter injury using FTHR19 and similar AUC values calculated for prediction of shunting using VI, AHW, and FOHR.38 Due to the longitudinal nature of our study, many scans fell beyond the reference range of 24–42 weeks GA defined for ventricular index.36 For this study, we decided to use FOHR, which is independent of GA and accounts for dilatation of the posterior and anterior portions of the lateral ventricles. In contrast, VI and AHW only represent dimensions of the frontal horns.
In the present study, while maximum FOHR was a strong predictor of worse outcome on regression analysis, the predictive value of FOHR on receiver operating characteristic analysis yielded only a fair AUC value of 75% compared to >90% reported in the other studies. A confluence of factors likely contributes to functional outcomes years out from the initial injury, such as medical comorbidities and socioeconomic factors.39 Further, PVL is an independent predictor that can occur in infants without IVH40 and likely infers an additive risk in those with IVH. Larger prospective studies will be required to capture these variables and ensure higher follow-up rates to develop tools for clinical decision making.
Limitations of this study include those inherent to the single-center retrospective study design. Although there was high inter-rater reliability for functional outcome scoring, there is an unknown risk of misclassification, especially for children with limited assessment and data. Future studies that do not utilize formalized testing should involve patient/parent contact to determine functional ability. Comparability across studies is furthermore limited by the fact that the patients in our cohort for whom we had follow-up information had higher rates of gastrotomy and trach dependence. There is some degree of bias toward higher acuity infant patients who would thus be expected to have higher rates of disabilities, such as CP. Additionally, as our hospital is a quaternary care center receiving transfer of infants requiring higher levels of care, there would be more medical complexity in our patient population overall. This may be one explanation for the high rates of CP observed in patients with Grade I and II IVH. The high rate of loss to follow-up may also lead to bias of data availability for patients with more serious medical problems. Clinical decision making may have evolved over the 15-year study period although we did not observe a correlation between birth year and outcome. Despite these limitations, there remains an independent association between FOHR and outcome after adjusting for confounders such as BW, length of hospital stay, and discharge with gastrostomy and/or trach tube, which may be surrogate indicators of medical complexity.
In conclusion, our study demonstrates an independent relationship between degree of ventriculomegaly and functional outcome irrespective of shunt status while adjusting for confounders. Presence of PVL remains to be an important predictor, even among patients who require a shunt. However, within patients with Grade IV IVH, ventriculomegaly was still a stronger predictor than PVL, further supporting the conclusion that ventriculomegaly is an independent predictor of outcome. Although we calculated a maximum FOHR that optimally predicted moderate–severe impairment, the specific measures and thresholds of ventriculomegaly that imparts the best outcomes while avoiding invasive treatment for patients who may not progress are yet to be determined in a rigorous way that accounts for confounders, such as PVL. Larger prospective studies or trials are warranted to establish reference ranges that incorporate clinical and demographic factors that need to be considered along with ventriculomegaly to direct intervention for these babies.
References
Cizmeci, M. N. et al. Assessment of brain injury and brain volumes after posthemorrhagic ventricular dilatation: a nested substudy of the randomized controlled Elvis Trial. J. Pediatr. 208, 191.e2–197.e2 (2019).
Vassilyadi, M., Tataryn, Z., Shamji, M. F. & Ventureyra, E. C. Functional outcomes among premature infants with intraventricular hemorrhage. Pediatr. Neurosurg. 45, 247–255 (2009).
Dorner, R. A. et al. Early neurodevelopmental outcome in preterm posthemorrhagic ventricular dilatation and hydrocephalus: Neonatal ICU Network Neurobehavioral Scale and imaging predict 3-6-month motor quotients and Capute Scales. J. Neurosurg. Pediatr. https://doi.org/10.3171/2019.9.PEDS19438 (2019).
Srinivasakumar, P. et al. Posthemorrhagic ventricular dilatation-impact on early neurodevelopmental outcome. Am. J. Perinatol. 30, 207–214 (2013).
de Vries, L. S. et al. Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: a randomised controlled trial. Arch. Dis. Child. Fetal Neonatal Ed. 104, F70–F75 (2019).
Cizmeci, M. N. et al. Randomized controlled Early versus Late Ventricular Intervention Study in posthemorrhagic ventricular dilatation: outcome at 2 years. J. Pediatr. 226, P28.E3–P35.E3 (2020).
Lai, G. Y. et al. Timing of temporizing neurosurgical treatment in relation to shunting and neurodevelopmental outcomes in post-hemorrhagic ventricular dilatation of prematurity: a meta-analysis. J. Pediatr. https://doi.org/10.1016/j.jpeds.2021.01.030 (2021).
Radhakrishnan, R. et al. Frontal occipital and frontal temporal horn ratios: comparison and validation of head ultrasound-derived indexes with MRI and ventricular volumes in infantile ventriculomegaly. AJR Am. J. Roentgenol. 213, 925–931 (2019).
Wellons, J. C. 3rd et al. Shunting outcomes in posthemorrhagic hydrocephalus: results of a hydrocephalus clinical research network prospective cohort study. J. Neurosurg. Pediatr. 20, 19–29 (2017).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J. Pediatr. 92, 529–534 (1978).
Fiser, D. H. Assessing the outcome of pediatric intensive care. J. Pediatr. 121, 68–74 (1992).
Pollack, M. M. et al. Relationship between the functional status scale and the pediatric overall performance category and pediatric cerebral performance category scales. JAMA Pediatr. 168, 671–676 (2014).
Leijser, L. M. et al. Posthemorrhagic ventricular dilatation in preterm infants: when best to intervene? Neurology 90, e698–e706 (2018).
van Zanten, S. A., de Haan, T. R., Ursum, J. & van Sonderen, L. Neurodevelopmental outcome of post-hemorrhagic ventricular dilatation at 12 and 24 months corrected age with high-threshold therapy. Eur. J. Paediatr. Neurol. 15, 487–492 (2011).
de Vries, L. S. et al. Early versus late treatment of posthaemorrhagic ventricular dilatation: results of a retrospective study from five neonatal intensive care units in the Netherlands. Acta Paediatr. 91, 212–217 (2002).
Bassan, H. et al. Timing of external ventricular drainage and neurodevelopmental outcome in preterm infants with posthemorrhagic hydrocephalus. Eur. J. Paediatr. Neurol. 16, 662–670 (2012).
Lo, M., Kishimoto, J., Eagleson, R., Bhattacharya, S. & de Ribaupierre, S. Does ventricular volume affect the neurodevelopmental outcome in infants with intraventricular hemorrhage? Childs Nerv. Syst. 36, 569–575 (2020).
Cizmeci, M. N. et al. Periventricular hemorrhagic infarction in very preterm infants: characteristic sonographic findings and association with neurodevelopmental outcome at age 2 years. J. Pediatr. 217, 79–85 (2020). e71.
Obeid, R. et al. The utility of the fronto-temporal horn ratio on cranial ultrasound in premature newborns: a ventriculomegaly marker. Pediatr. Res. https://doi.org/10.1038/s41390-020-01337-x (2021).
Jary, S., Kmita, G., Wroblewska, J. & Whitelaw, A. Quantitative cranial ultrasound prediction of severity of disability in premature infants with post-haemorrhagic ventricular dilatation. Arch. Dis. Child. 97, 955–959 (2012).
Shankaran, S. et al. Outcomes following post-hemorrhagic ventricular dilatation among infants of extremely low gestational age. J. Pediatr. https://doi.org/10.1016/j.jpeds.2020.07.080 (2020).
Norooz, F. et al. Decompressing posthaemorrhagic ventricular dilatation significantly improves regional cerebral oxygen saturation in preterm infants. Acta Paediatr. 104, 663–669 (2015).
Vesoulis, Z. A., Whitehead, H. V., Liao, S. M. & Mathur, A. M. The hidden consequence of intraventricular hemorrhage: persistent cerebral desaturation after IVH in preterm infants. Pediatr. Res. 89, 869–877 (2021).
Klebermass-Schrehof, K. et al. Can neurophysiological assessment improve timing of intervention in posthaemorrhagic ventricular dilatation? Arch. Dis. Child. Fetal Neonatal Ed. 98, F291–F297 (2013).
Jary, S., De Carli, A., Ramenghi, L. A. & Whitelaw, A. Impaired brain growth and neurodevelopment in preterm infants with posthaemorrhagic ventricular dilatation. Acta Paediatr. 101, 743–748 (2012).
McClugage, S. G. et al. Functional outcomes at 2 years of age following treatment for posthemorrhagic hydrocephalus of prematurity: what do we know at the time of consult? J. Neurosurg. Pediatr. https://doi.org/10.3171/2019.12.PEDS19381 (2020).
Dorner, R. A. et al. The relationship between clinical imaging and neurobehavioral assessment in posthemorrhagic ventricular dilation of prematurity. Front. Physiol. 10, 64 (2019).
Brouwer, A. et al. Neurodevelopmental outcome of preterm infants with severe intraventricular hemorrhage and therapy for post-hemorrhagic ventricular dilatation. J. Pediatr. 152, 648–654 (2008).
Fiser, D. H. et al. Relationship of pediatric overall performance category and pediatric cerebral performance category scores at pediatric intensive care unit discharge with outcome measures collected at hospital discharge and 1- and 6-month follow-up assessments. Crit. Care Med. 28, 2616–2620 (2000).
Abecassis, I. J. et al. Toward a comprehensive assessment of functional outcomes in pediatric patients with brain arteriovenous malformations: the pediatric quality of life inventory. J. Neurosurg. Pediatr. 18, 611–622 (2016).
Rohlwink, U. K. et al. Imaging features of the brain, cerebral vessels and spine in pediatric tuberculous meningitis with associated hydrocephalus. Pediatr. Infect. Dis. J. 35, e301–e310 (2016).
Lichenstein, R. et al. Presentations and outcomes of children with intraventricular hemorrhages after blunt head trauma. Arch. Pediatr. Adolesc. Med. 166, 725–731 (2012).
Raymond, T. T. et al. Outcomes among neonates, infants, and children after extracorporeal cardiopulmonary resuscitation for refractory inhospital pediatric cardiac arrest: a report from the National Registry of Cardiopulmonary Resuscitation. Pediatr. Crit. Care Med. 11, 362–371 (2010).
Whittemore, B. A., Swift, D. M., Thomas J. M. & L. F. Chalak, L. F. A neonatal neuroNICU collaborative approach to neuromonitoring of posthemorrhagic ventricular dilation in preterm infants. Pediatr. Res. https://doi.org/10.1038/s41390-021-01406-9 (2021).
Cizmeci, M. N. & de Vries, L. S. Fronto-temporal horn ratio: yet another marker of ventriculomegaly? Pediatr. Res. 10.1038/s41390-021-01379-9 (2021).
Brouwer, M. J. et al. New reference values for the neonatal cerebral ventricles. Radiology 262, 224–233 (2012).
Beijst, C. et al. Two-dimensional ultrasound measurements vs. magnetic resonance imaging-derived ventricular volume of preterm infants with germinal matrix intraventricular haemorrhage. Pediatr. Radiol. 50, 234–241 (2020).
Leijser, L. M. et al. Post-hemorrhagic ventricular dilatation: inter-observer reliability of ventricular size measurements in extremely preterm infants. Pediatr. Res. https://doi.org/10.1038/s41390-020-01245-0 (2020).
Benavente-Fernandez, I., Siddiqi, A. & Miller, S. P. Socioeconomic status and brain injury in children born preterm: modifying neurodevelopmental outcome. Pediatr. Res. 87, 391–398 (2020).
Wang, L. W. et al. Isolated cystic periventricular leukomalacia differs from cystic periventricular leukomalacia with intraventricular hemorrhage in prevalence, risk factors and outcomes in preterm infants. Neonatology 111, 86–92 (2017).
Author information
Authors and Affiliations
Contributions
G.Y.L. contributed to the concept and design, acquisition of data, analysis and interpretation of the data, and drafting the article. S.A. contributed to the acquisition of data. M.L.V.D. and S.K.L. were involved in the concept and design of the study. M.L.V.D., S.K.L., R.-A.O.D.R., and D.G.-S. contributed to the interpretation of the data. All authors contributed to critically revising the article for important intellectual content and approved the final version of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent
No consent was required for retrospective review of the anonymized data.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lai, G.Y., Abdelmageed, S., DeRegnier, RA.O. et al. Degree of ventriculomegaly predicts school-aged functional outcomes in preterm infants with intraventricular hemorrhage. Pediatr Res 91, 1238–1247 (2022). https://doi.org/10.1038/s41390-021-01631-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01631-2