Abstract
Background
The objective of this study was to examine the association of an integrated model (composed of retinal arteriolar caliber, height, and sex) with blood pressure (BP) among a group of Chinese children, and assess the predictive value of the integrated model for childhood hypertension.
Methods
This study included 1460 candidates aged 12.634 ± 0.420 years. Height, weight, waist circumference, and BP were obtained and ophthalmological measurements were taken. The computer-imaging program (IVAN, University of Wisconsin, Madison, WI) was used to measure calibers of retinal vessels. Receiver-operating characteristic curve (ROC) analyses were performed to assess the accuracy of the integrated model as a diagnostic test of elevated BP in children.
Results
The accuracy of the integrated model (assessed by area under the curve) for identifying elevated BP was 0.777 (95% confidence interval: 0.742–0.812). The optimal threshold of the integrated model for defining hypertension was 0.153, and the calculation formula for the specific predictive risk was: Logit (p/1 − p) = −5.666 − 0.261 × retinal arteriolar caliber + 0.945 × sex + 0.438 × height. In identifying elevated BP, the sensitivity and specificity were 0.711 and 0.736, respectively.
Conclusions
The model containing eye message is a comprehensive and relatively effective index to identify elevated BP in 12-year-old children, which can offer assistance to further understand childhood microcirculation disease.
Impact
-
We firstly incorporated retinal vascular diameter, sex, and height into one integrated model to identify hypertension in 12-year-old children.
-
The current discrimination of hypertension in children is difficult. There have been some studies to simplify the diagnosis of children’s hypertension, but they were limited to anthropometric measurements. We proposed a composed model containing microcirculation information to predict childhood hypertension.
-
Based on the knowledge that microcirculation is not only a means to study the manifestations but also early pathogenic correlates of hypertension, the combined model containing microcirculation message as a method may provide new insights into the diagnosis of childhood hypertension.
Similar content being viewed by others
Introduction
High blood pressure (BP) is a major public health problem and is responsible for 9.4 million deaths annually.1 In the past, the judgments on an increased risk of hypertension (HTN) had been practically focused on adults or relatively older subjects. However, in the past few decades, due to the increasing prevalence of obesity and unhealthy lifestyle habits (such as excessive salt intake, lack of exercise, etc.) among children,2,3,4 high BP in children and adolescents has become more and more common in western countries and China.5,6,7 Longitudinal studies have reported that elevations of BP in pediatric levels often turned into stable HTN and increased cardiovascular burden on adulthood, and may provide a window in the life course where timely and effective prevention could be focused.8,9,10 Consequently, identifying children most at risk of developing future HTN is of important significance.
HTN has profound effects on the structure and function of the microvasculature.11 With the development of computer-assisted analysis systems, retinal fundus examination was employed by population-based studies to measure individual arterioles and venules and combine them into central retinal arteriolar equivalent and central retinal venule equivalent, representing the average arteriolar and venular caliber of that eye, respectively.12 What deserves attention is that a few studies have shown that elevated BP in children is associated with retinal vessel caliber, suggesting that elevated BP may affect the retinal microvascular system in young children.13,14,15,16
In fact, identifying HTN in children and adolescents is much more complicated than in adults because there are 476 sex-, age-, and height-specific cutoffs to assess elevated BP among children aged 1–17 years for both sexes,7 which are less easily used by even professional pediatricians in clinical practice. Being aimed at the diagnosis problems with elevated BP in children, this study examined the association of an integrated model (combined three covariates: retinal arteriolar caliber, height, and sex) with elevated BP among 12-year-old children in a relatively large population of China and to assess the predictive value of the integrated model to elevated BP in adolescents aged 12 years.
Materials and methods
Study population
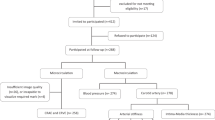
The Anyang Childhood Eye Study is a school-based cohort study designed to observe the occurrence and development of myopia as well as other diseases in schoolchildren living in Anyang urban area, Henan Province, Central China. The detailed methodology of the study has been previously described.17 In brief, 1460 grade 7 students aged 12.634 ± 0.420 years have been examined from October 2011 to December 2011. The flowchart of participants included in the present study was shown in Fig. 1. Ethics approval was obtained from the institutional review board of Beijing Tongren Hospital, Capital Medical University, and followed the tenets of the Declaration of Helsinki. Informed written consent was obtained from at least one parent. Verbal assent was obtained from each child.
Retinal photography and measurement of retinal vascular caliber
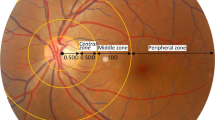
The children were examined at the health examination station of the Anyang Eye Hospital. A non-mydriatic fundus camera (Canon CR-2, Tokyo, Japan) was used to capture 45° fundus images centering on the optic disc and macular area of children’s right eyes by a well-trained operator. Children with abnormal fundus images (such as confounding pathology, out of focus, or too dark) would also undergo left eye measurements.
According to a standardized protocol described previously,12 the computer-imaging program (IVAN, University of Wisconsin, Madison, WI) was used to measure calibers of all retinal arterioles and venules. One grader masked to children’s identity and characteristics performed all measurements. Before starting the measurement, 50 randomly selected retinal images were repeatedly measured by the grader with an interval of 2 weeks. The reliability was high with interclass correlation coefficients of 0.85 for arteriolar caliber and 0.97 for venule caliber.
BP measurement
BP of children was measured in a seated position after 5 min of rest using an automated sphygmomanometer (HEM-907, Omron, Kyoto, Japan) with appropriate cuff size (bladder length ≈80% and width at least 40% of the arm circumference, covering the upper arm but not obscuring the antecubital fossa). Systolic and diastolic BP (SBP and DBP, respectively) readings were taken. Two readings were taken 5 min apart and averaged for analysis.
We used the age- and sex-specific BP reference standard of Chinese children and adolescents to identify the children with elevated BP. That is, SBP or DBP ≥ 90th percentile of the SBP or DBP with the same age and sex, or BP ≥ 120/80 mm Hg, even if this figure is <90th percentile, were defined as elevated BP.7
Other measurements
Any abnormality of the anterior segment was observed and recorded using a slit-lamp (YZ5J, 66 Vision Tech Co, Suzhou, China). Cycloplegic spherical equivalent refraction was measured using an autorefractor (HRK7000 A, Huvitz, Gunpo, South Korea) with three readings taken and averaged.18 Axial length was measured using IOL Master (Carl Zeiss Meditec AG, Jena, Germany) with five repeated measurements taken and averaged.19 Height and weight were measured using an automatic and professional integrated set. Body mass index (BMI) was calculated as weight/height2 (kg/m2). Waist circumference was measured with a tape measure and was defined as the narrowest part of the student’s trunk. Birth information including gestational weeks, birth weight, and birth length were collected by administrating questionnaires to the parents.
Statistical analysis
The average value ± standard deviation was used to describe the measurement data, and the frequency distribution was used to describe the counting data. Before the single-factor analysis, the normal state of the grouping data (according to the HTN grouping) was tested by Shapiro test; p > 0.05 was considered to conform to the normal distribution; if not satisfying the normal state, the rank and test of two independent samples were adopted, with the test level α = 0.05. The variants with statistical significance in the single-factor analysis were incorporated into multivariate logistic regression analysis. To facilitate the interpretation of the results, the independent variables were converted into quartile classification data before the regression analysis. The receiver-operating characteristic curve (ROC) analyses were used to examine the predictive value of the integrated model and to determine the cut-off values by the Youden’s index. All analyses were performed by SAS (SAS Institute Inc., 100 SAS Campus Drive Cary, NC 27513-2414, USA). P < 0.05 were considered statistically significant.
Results
A total of 1460 subjects aged 12.634 ± 0.420 years were conducted in our study; 52.95% (n = 773) were males. The prevalence of elevated BP in children was 12.808% (males: 7.503%; females: 18.777%). Compared with boys, girls had higher SBP, higher waist circumference and BMI, and narrower retinal arteriolar and venular caliber. (The data were shown in Table 1.)
The results of single-factor analysis were provided with Table 2, with the test level α = 0.05; if subjects with elevated BP might be affected by retinal arteriolar caliber, axial length, waist circumference, BMI, birth weight, age, weight, height, and sex (P < 0.05), then these nine indices were chosen into multiple logistic regression model, and the results were shown in Table 3, and the logistic regression assignment list was shown in Table 4. Consequently, retinal arteriolar caliber, sex, and height were selected from the nine indices to predict elevated BP in children, and integrated covariates were also made, as showed in Table 5.
Based on the area under the curve (AUC) of the integrated covariates in the prediction of elevated BP in children, we could see that the AUC of integrated covariates was significantly higher than that of other indices such as retinal arteriolar caliber, sex, and height in the prediction of children hypertension.
According to the results of multivariate regression, we simultaneously fitted a regression formula to predict the risk of elevated BP in children, the formula was as follows:
Logit(p/1 − p) = −5.666 – 0.261 × retinal arteriolar caliber + 0.945 × sex + 0.438 × height.
Discussion
Unlike the definition used in the diagnostic criteria for adult HTN, which is supported by thhe outcome data such as cardiovascular morbidity and mortality, investigators recommend using population-based normative data to define pediatric HTN because BP approximates a normal distribution. BP between the 90th and 95th percentile is pre-HTN, and in adolescents, BP ≥ 120/80 mm Hg is pre-HTN even if this figure is <90th percentile, and BP ≥ 95th percentile may be HTN. However, these percentiles have to be adjusted for children’s age, sex, and height percentiles, which are variables known to influence BP.20 The age-, sex- and height-specific standards of SBP and DBP are less easily used by even professional pediatricians in clinical practice.21,22 Therefore, improved or auxiliary diagnostic methods are more important for children with HTN, and nowadays, different methods have been put forward to simplify the diagnosis of HTN among children.23,24,25 In this study, we proposed an integrated model to predict the risk of elevated BP in adolescents, which is composed of three elements (retinal arteriolar caliber, height, and sex). When using the integrated covariates as a whole to predict HTN in adolescents, the overall predictive validity is 0.777, and the optimal cut-off point of the integrated covariates is 0.153. In identifying elevated BP in adolescents, the sensitivity is 0.711 and the specificity is 0.736.
Our integrated model has several advantages in practice for predicting the risk of elevated BP in adolescents:
First, the three key elements in our formula are all significantly related to BP in children. Retinal arteriolar caliber is associated with elevated BP in several epidemiological studies based on the pediatric population, with each 10 mm Hg increase in SBP/DBP associated with a 1.70–2.08 μm decrease in retinal arteriolar caliber from preschoolers to adolescents.13,14,15,16 The other two important components, sex and height, are closely associated with BP in adolescents, and identifying HTN in children and adolescents is based on a set of sex- and height-specific references of SBP and DBP.21,26,27,28
Second, although BP has been generally accepted as a reasonable diagnostic criterion, it still has potential limitations. The value of BP measurement is susceptible to external environments and conditions. More importantly, a physician or researcher must be able to accurately judge out whether a child has white-coat HTN or masked HTN. The reported frequency of white-coat HTN varies, perhaps as a result of the criteria used to establish the diagnosis, with values ranging from 1% to as high as 44%,29 and the masked HTN occurs in ~10% of children and adolescents.30 The two phenomenons are less well determined in children than in adults. Sometimes ambulatory BP monitoring is required to make this diagnosis, and in fact, there is little consensus on how to manage children with white-coat HTN or masked HTN.30,31 However, the three indexes included in our formula are relatively objective measurements, less influenced by the subject’s emotion and psychology, and do not need repeated measurements on different occasions.
Third, the retina is the only part of the body that microvascular system can be observed directly, and retinal vascular imaging is a technology that allows objectively noninvasive in vivo assessment and monitoring of the microvasculature. The examination and analysis process of fundus blood vessels can be achieved by professionals using ophthalmic equipment and software. The presence of microvascular disease is regarded as an important pathological feature of HTN.11 At the same time, the increase in peripheral vascular resistance relates to changes in the microcirculation, which has also played an important role in the pathogenesis and development of HTN.11,32 In the past, the studies on the simplified prediction of elevated BP in children were confined to anthropometric measurements such as BP itself, height, weight, waist circumference, hip circumference, and so on.24,33,34 Since the importance of microcirculation as both a means to study the manifestations and early pathogenic correlates of HTN, we firstly incorporated retinal microscopic vascular diameter into the predictive model expecting to achieve a more comprehensive, relatively effective prediction of elevated BP in children. Since BP is still considered a reasonable diagnostic standard, this study also used BP as a reference to examine the effectiveness of the model, and we hope that this composed model can play an active role in the diagnosis of elevated BP in children.
Fourth, in our study, the comprehensive model combined three factors closely related to HTN, and the diagnostic value of this comprehensive model for children with elevated BP was evaluated by the ROC curve. With the model as a whole to predict HTN, the cut-off value point was 0.153, and the overall predictive effectiveness of the model could reach 0.777. The results of this study underscore the importance of taking synthetic covariants into account, because childhood HTN itself is very complex and affected by many factors, and the benefits of the comprehensive model reflect that HTN itself is a comprehensive indicator that is affected by multiple factors.
According to the formula of our study, girls were more likely to have elevated BP than boys. A few researchers had indicated that the risk of developing sustained HTN was higher in boys compared to that in girls.35 However, the effect of children’s sex on HTN prevalence remains unclear, as data showed that on controlling all covariates including BMI, BP had increased among girls but decreased among adolescent boys aged 13–17 years during 2003–2006 when compared with 1988–1994.36 Rosner et al. also reported that the prevalence of elevated BP significantly increased among girls (8.2 versus 12.6%; P = 0.007), but was only of borderline significance among boys (15.8 versus 19.2%; P = 0.057), after analyzing a population-based sample of 3248 children in National Health and Nutrition Examination Survey (NHANES) III (1988–1994) and 8388 children in continuous NHANES (1999–2008), aged 8–17 years.3 Compared with boys in our study, girls were heavier and had higher waist and BMI, which might also explain the BP difference between the two sexes to some extent, considering the effects of weight and obesity on BP.
Our main outcome measure was elevated BP (SBP or DBP ≥90th percentile or SBP/DBP ≥120/80 mm Hg). The scope of this study covered adolescents with HTN and pre-HTN/high-normal BP. Both the United States20 and European Society of Hypertension Guidelines37 introduced the concept termed “pre-hypertension/high-normal BP”, defined as SBP or DBP ≥90th percentile but <95th percentile or BP ≥ 120/80 mm Hg but below 95th percentile. The previous data suggested that pre-HTN/high-normal BP implies increased risk not only for future HTN but also for the emergence of early target-organ damage.38,39 In our study, the risk of HTN in adolescents with pre-HTN/high-normal BP was also taken into account, hence the adolescents with pre-HTN/high-normal BP were also treated as a target group.
There are some limitations in this study, first, it only included Chinese adolescents 12 years old, limiting the ability to apply the study results to other children groups. Second, the study design is cross-sectional and does not provide temporal information on the associations. Third, the possible selection bias giving rise to the exclusion of students by ineligibility and ungradable retinal photographs may play a part in the real association between BP and retinal vessel diameters.
In conclusion, since the importance of the microcirculation as both a means to study the manifestations and early pathogenic correlates of HTN, we firstly incorporated retinal microscopic vascular diameter into an integrated model, expecting to achieve a more comprehensive and relatively effective prediction of elevated BP in children, especially in the case of some complex and uncertain conditions such as white-coat effect and masked HTN. To better understand the role of microcirculation in the diagnosis of HTN in children, and to further evaluate the predictive ability of this composite model for other children groups, such as children of different ages, different regions/countries, as well as diseased children, more in-depth researches are needed.
References
Lim, S. S. et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2224–2260 (2012).
Kumar, S. & Kelly, A. S. Review of childhood obesity: from epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clinic Proc. 92, 251–265 (2017).
Rosner, B., Cook, N. R., Daniels, S. & Falkner, B. Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988-2008. Hypertension 62, 247–254 (2013).
Lava, S. A., Bianchetti, M. G. & Simonetti, G. D. Salt intake in children and its consequences on blood pressure. Pediatr. Nephrol. 30, 1389–1396 (2015).
Karatzi, K. et al. Prevalence of hypertension and hypertension phenotypes by age and gender among schoolchildren in Greece: The Healthy Growth Study. Atherosclerosis 259, 128–133 (2017).
Muntner, P., He, J., Cutler, J. A., Wildman, R. P. & Whelton, P. K. Trends in blood pressure among children and adolescents. JAMA 291, 2107–2113 (2004).
Liang, Y. J. et al. Trends in blood pressure and hypertension among Chinese children and adolescents: China Health and Nutrition Surveys 1991–2004. Blood Pressure 20, 45–53 (2011).
Lurbe, E. et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J. Hypertens. 34, 1887–1920 (2016).
Moyer, V. A. Screening for primary hypertension in children and adolescents: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 159, 613–619 (2013).
Juhola, J. et al. Combined effects of child and adult elevated blood pressure on subclinical atherosclerosis: the International Childhood Cardiovascular Cohort Consortium. Circulation 128, 217–224 (2013).
Feihl, F., Liaudet, L., Waeber, B. & Levy, B. I. Hypertension: a disease of the microcirculation? Hypertension 48, 1012–1017 (2006).
Hubbard, L. D. et al. Methods for evaluation of retinal microvascular abnormalities associated with hypertension/sclerosis in the Atherosclerosis Risk in Communities Study. Ophthalmology 106, 2269–2280 (1999).
Mitchell, P. et al. Blood pressure and retinal arteriolar narrowing in children. Hypertension 49, 1156–1162 (2007).
Li, L. J. et al. Influence of blood pressure on retinal vascular caliber in young children. Ophthalmology 118, 1459–1465 (2011).
Gishti, O. et al. Retinal microvasculature and cardiovascular health in childhood. Pediatrics 135, 678–685 (2015).
Gopinath, B. et al. Influence of blood pressure and body mass index on retinal vascular caliber in preschool-aged children. J. Hum. Hypertens. 27, 523–528 (2013).
Li, S. M. et al. Design, methodology and baseline data of a school-based cohort study in central China: the Anyang Childhood Eye Study. Ophthalmic Epidemiol. 20, 348–359 (2013).
Atchison, D. A. et al. Relative peripheral hyperopia does not predict development and progression of myopia in children. Invest. Ophthalmol. Vis. Sci. 56, 6162–6170 (2015).
Li, S. M. et al. Distribution of ocular biometry in 7- and 14-year-old Chinese children. Optom. Vis. Sci. 92, 566–572 (2015).
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114, 555–576 (2004).
Hansen, M. L., Gunn, P. W. & Kaelber, D. C. Underdiagnosis of hypertension in children and adolescents. JAMA 298, 874–879 (2007).
Bijlsma, M. W., Blufpand, H. N., Kaspers, G. J. & Bokenkamp, A. Why pediatricians fail to diagnose hypertension: a multicenter survey. J. Pediatr. 164, 173–177 (2014). e177.
Somu, S., Sundaram, B. & Kamalanathan, A. N. Early detection of hypertension in general practice. Arch. Dis. Childhood 88, 302 (2003).
Chiolero, A., Paradis, G., Simonetti, G. D. & Bovet, P. Absolute height-specific thresholds to identify elevated blood pressure in children. J. Hypertens. 31, 1170–1174 (2013).
Kaelber, D. C. & Pickett, F. Simple table to identify children and adolescents needing further evaluation of blood pressure. Pediatrics 123, e972–e974 (2009).
Rosner, B., Prineas, R. J., Loggie, J. M. & Daniels, S. R. Blood pressure nomograms for children and adolescents, by height, sex, and age, in the United States. J. Pediatr. 123, 871–886 (1993).
Regnault, N. et al. Components of height and blood pressure in childhood. Int. J. Epidemiol. 43, 149–159 (2014).
Xi, B. et al. Establishing international blood pressure references among nonoverweight children and adolescents aged 6 to 17 years. Circulation 133, 398–408 (2016).
Lurbe, E., Torro, M. I. & Alvarez, J. Ambulatory blood pressure monitoring in children and adolescents: coming of age? Curr. Hypertens. Rep 15, 143–149 (2013).
Di Salvo, G. et al. Masked hypertension in young patients after successful aortic coarctation repair: impact on left ventricular geometry and function. J. Hum. Hypertens. 25, 739–745 (2011).
Wuhl, E. et al. Strict blood-pressure control and progression of renal failure in children. N. Engl. J. Med. 361, 1639–1650 (2009).
Levy, B. I., Ambrosio, G., Pries, A. R. & Struijker-Boudier, H. A. Microcirculation in hypertension: a new target for treatment? Circulation 104, 735–740 (2001).
Kakinami, L. et al. Association between different growth curve definitions of overweight and obesity and cardiometabolic risk in children. CMAJ 184, E539–E550 (2012).
Ashwell, M., Gunn, P. & Gibson, S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes. Rev. 13, 275–286 (2012).
Lurbe, E. et al. Sexual dimorphism in the transition from masked to sustained hypertension in healthy youths. Hypertension 62, 410–414 (2013).
Ostchega, Y. et al. Trends of elevated blood pressure among children and adolescents: data from the National Health and Nutrition Examination Survey 1988–2006. Am. J. Hypertens. 22, 59–67 (2009).
Lurbe, E. et al. Management of high blood pressure in children and adolescents: recommendations of the European Society of Hypertension. J. Hypertens. 27, 1719–1742 (2009).
Redwine, K. M., Acosta, A. A., Poffenbarger, T., Portman, R. J. & Samuels, J. Development of hypertension in adolescents with pre-hypertension. J. Pediatr. 160, 98–103 (2012).
Drukteinis, J. S. et al. Cardiac and systemic hemodynamic characteristics of hypertension and prehypertension in adolescents and young adults: the Strong Heart Study. Circulation 115, 221–227 (2007).
Acknowledgements
We thank the support from the Anyang city government for helping to organize the survey. We acknowledge the UW Fundus Photograph Reading Center and Nicola Ferrier of the School of Engineering at UW for providing the software for measuring retinal vessel calibers. This work was supported by grants from the capital health research and development of special (2020-2-1081), Beijing Talents Found (2016000021223ZK28), the National Natural Science Foundation of China (82071000), and Beijing Natural Science Foundation (JQ20029).
The Anyang Childhood Eye Study Group
STUDY CHAIR’S OFFICE: Ningli Wang4, Shi-Ming Li4, Luo-Ru Liu5, Paul Mitchell6; COORDINATING CENTER: Xiuzi Zhou7, Weixin He8, Wenjie Li5, Yazhou Ji5, Fangrong Shi5, Jiyuan Guo5; MAIN INVESTIGATORS: Fengju Zhang4, Si-Yuan Li4, Meng-Tian Kang4, Jin Fu4, Lei Li4, Shiqiang Zhao4, Yang Wang4, Yan Xu4, Zhou Yang4, Bi-Dan Zhu9, Yazhou Ji5, Hailin Meng5, He Li5, Fangrong Shi5, Yongfang Tu5, Yipeng Wang5, Hongliang Zhang5, Donghai Yang5, Wenfang Niu5, Jinling Li5, Jiyuan Guo5, Baohong Han5, Lin Jia5, Zuowei Qi5, Zhenhuai Kang5, Bing Cao5, Xianfang Du5, Yicao Zhang5, Chuanqi Xie5, Bingqi Zhang5, Songtao Li5, Xiaoyuan Yang10, Bo Wang11; COMMITTEES Data and Safety Monitoring: Si-Yan Zhang12, Hongyuan Wang12, Xiaoxia Peng13, Lei Li4
Author information
Authors and Affiliations
Consortia
Contributions
Y.H.: drafting manuscript and data analysis/interpretation; S.-M.L.: concept and design; Q.Z.: data analysis/interpretation; K.C.: data analysis/interpretation and statistical analysis; M.-T.K.: data acquisition and data analysis/interpretation; L.-R.L.: data acquisition, admin, technical, or material support; H.L.: data acquisition, admin, technical, or material support; N.W.: concept and design, and supervision and final approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Informed written consent was obtained from at least one parent. Verbal assent was obtained from each child.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
He, Y., Li, SM., Zhang, Q. et al. The performance of an integrated model including retinal information in predicting childhood hypertension. Pediatr Res 91, 1600–1605 (2022). https://doi.org/10.1038/s41390-021-01535-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01535-1