Abstract
Background
An epidemic of thunderstorm asthma in pediatric patients occurred in Yulin, a northwest city of China, on 11 September 2018. We described the epidemic and retrospectively analyzed the demographic and clinical aspects of the involved children.
Methods
The caseload data of patients were collected from the hospital information system in Yulin Pediatric Hospital. The detailed document of hospitalized children with thunderstorm asthma was sourced from the medical records.
Results
The mean number of daily visits to emergency/outpatient department and the daily admission to hospital were 2.7 and 16 times, respectively, than on the other days of September. A gender prominence of males was observed in both emergency/outpatient and inpatient department. Among the 51 hospitalized children with detailed medical records, 56% of them had never experienced or were diagnosed with asthma and 25% had confirmed diagnosis of asthma. Sixty-seven percent had a history of allergic rhinitis during August and September. Seventy-six percent of the hospitalized children presented as moderate asthma. Ninety-four percent of the pediatric patients had positive IgE against mugwort pollen and 78% were monosensitized to pollen.
Conclusion
Thunderstorm asthma can affect children, especially who has allergic rhinitis or asthma without preventive management. Mugwort is also an aeroallergen in thunderstorm asthma attacks.
Impact
-
Thunderstorm can induce asthma attacks in children with allergic rhinitis owing to mugwort and aggravate symptoms in children with confirmed diagnosis of asthma.
-
Children with mugwort allergy are susceptible to thunderstorm asthma and a preponderance of boys was observed.
-
Better identification of allergic children to mugwort, giving suitable protective measures during thunderstorm and standard therapy to existing allergic situation could be a benefit for children at risk of thunderstorm asthma.
Similar content being viewed by others
Introduction
Thunderstorm asthma refers to a rare phenomenon of sudden onset or exacerbation of asthma symptoms during or shortly after a thunderstorm, which leads to a markedly increased number of patients with respiratory problems in the emergency department over a short period. Thunderstorm asthma is thought to have first been reported in 1983 by Packe and Ayres.1 Twenty-six patients who developed asthma symptoms following a thunderstorm event visited the emergency department of East Birmingham Hospital in the United Kingdom (UK), whereas the usual asthma attendance was only two or three patients, on average. Since then, many studies have described an association between thunderstorms and the onset of asthma, mainly in the UK and Australia but also in Canada, Italy, and Iran.2,3,4,5,6,7,8,9,10 Among these, the most striking and devastating event occurred on 21 November 2016 in Melbourne, Australia, involving more than 3000 patients and 10 possible deaths owing to thunderstorm asthma.11
The mechanism of thunderstorm asthma has not been clarified. These events have been observed to be associated with extremely high allergen levels during a thunderstorm.12 The predominant aeroallergens are grass pollen and occasionally fungal spores.2,3,4,5,6,7,8,9,10 Currently, the generally accepted hypothesis is that pollen is entrained by upward airflows into the humid cloud base of a thunderstorm, which ruptures owing to osmotic shock and releases respirable allergenic particles. Then, downdrafts and rain transport these particles to ground level. Pollen debris can deposit into the lower airway and trigger an asthma attack in susceptible people with pollen allergies.13
Yulin City is in Shanxi Province, which is located in northern China covering an area of 43,578 km2. According to the census in 2017, Yulin has a permanent population of 3.7 million, with per capita gross national product of US$19,356. It has been estimated that about 12% of people in Yulin City have seasonal rhinitis and 80–90% have symptoms during the summer and autumn, i.e., from July to September. Mugwort (Artemisia desterorum Spreng) is the most important allergen during this period. For desertification control, mugwort has been planted at a large scale in the area due to the ecological value of the plant for its ability to solidify sand. On 11 September 2018, the emergency and outpatient services of Yulin Pediatric Hospital were overwhelmed with children who had sudden onset of shortness of breath, cough, or wheezing during and shortly after a thunderstorm event.
We aimed to report an epidemic of thunderstorm asthma among children in Yulin City, northwest China, where thunderstorm asthma has not been investigated. In addition, we sought to characterize, for the first time, the clinical features of pediatric patients with thunderstorm asthma.
Methods
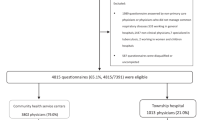
We retrospectively reviewed the data of pediatric patients who attended the emergency and outpatient departments of Yulin Pediatric Hospital owing to sudden onset or aggravated wheezing or asthma during or shortly following a thunderstorm event in Yulin City, Shanxi Province, China. Extreme weather conditions involving thunderstorms and wind began around 18:00 on 11 September 2018 in Yulin City, and lasted until 22:00 on the same day, followed by a sudden increase in the number of children who visited the emergency pediatric department between 11 and 13 September, complaining of respiratory problems. We collected information of patients who attended the hospital from 18:00 on 11 September 2018 to 23:59 on 13 September 2018, and reviewed the data of patients with a preliminary diagnosis of “asthma”, “wheezing”, “cough”, or “shortness of breath”. Then, patients with a confirmed diagnosis of asthma were included in our study and those with a final diagnosis of infectious respiratory disease or diagnosis rather than asthma were excluded. The diagnosis of asthma was based on the Global Initiative for Asthma (GINA) (2015) guidelines. All data were sourced from the hospital information system for the study period.
Children with severe asthma symptoms were admitted to the hospital. Pulmonary function, fractional concentration of exhaled nitric oxide (FeNO), and responses to common allergens were measured. AllergyScreen (Mediwiss Analytic GmbH, Moers, Germany) was used to test for specific IgE against house dust, dust mites, mixed molds (Penicillium chrysogenum, Cladosporium herbarum, Aspergillus fumigatus, Aspergillus niger, and Alternaria alternata), cat and dog dander, mulberry, mixed weed pollens (careless weed, goosefoot, Japanese hop, and dandelion), mugwort/ragweed, and mixed tree pollens (mountain juniper, elm, maple leaf sycamore, white ash, willow, birch, oak, cottonwood, alder, and hazel). Clinical data were obtained from the patients’ medical records. GraphPad Prism 5.01 was used for graphic analysis.
Results
Increased number of patients with asthma owing to thunderstorms in the emergency, outpatient, and inpatient departments
The thunderstorm occurred from 18:00 to 22:00 on 11 September 2018 in Yulin City. Following the weather event, there was a sudden increase in the number of children who visited the emergency pediatric department between 11 and 13 September, complaining of shortness of breath, wheezing, and dyspnea (Fig. 1). During the 3 days following the thunderstorms, there were 391 pediatric patients with shortness of breath, wheezing, dyspnea (Fig. 1). Among them, 102 were female and 290 were male children. The patient caseload during the 3 days following the thunderstorms comprised 23% of the total 1685 children with the same complaints during the entire month of September. The mean number of daily visits to the pediatric emergency and outpatient departments owing to shortness of breath, wheezing, or dyspnea from 11 to 13 September was 130, which was 2.7 times that on other days in September (mean = 48).
A total of 157 patients were admitted to the inpatient department because of asthma during the entire month of September; among the total, 101 patients were admitted to the hospital between 11 and 13 September (Fig. 1). Of these 101 children, 73 were boys. The mean number of daily admissions to the hospital during 11−13 September was 33, which was 16 times that during the other days in September (mean = 2).
Among the total 391 patients, 241 (62%) visited the emergency or outpatient department in the first 24 h after the thunderstorms began, and the peak visits were during the first 18−24 h. Among the 101 patients admitted to the inpatient department, 48 (48%) were admitted during the first 24 h after the thunderstorm event, with peak admissions during the first 24−30 h. The hourly caseload of patients with shortness of breath, wheezing, or dyspnea in the emergency/outpatient, and inpatient departments is illustrated in Fig. 2.
Clinical features of thunderstorm asthma among the admitted pediatric patients
We descriptively analyzed the data of 51 hospitalized children diagnosed with asthma who had complete medical records. Among them, 44 children were male. Patients’ ages ranged from 3 to 14 years old, and the median age was 7 years.
Twenty-nine patients (57%) had never been diagnosed with asthma and had not experienced any previous asthma manifestations; the first asthma attack in these patients occurred following the abovementioned thunderstorm event. Among these 29 patients, 76% (n = 22/29) had a history of allergic rhinitis during August and September, 10% (n = 3/29) had eczema, and 17% (n = 5/29) had no atopic history. Thirteen (25%) pediatric patients had a previously confirmed diagnosis of asthma; 11 (21%) had been free of asthma symptoms for more than 6 months and did not use any preventive medication before the thunderstorm event; and 2 (4%) patients had current asthma but were not receiving therapy at the time of the thunderstorm. In addition, nine children (18%) were considered to have underdiagnosed asthma because they experienced paroxysmal shortness of breath, labored breath, or wheezing suggestive of asthma.
Among the total of 51 hospitalized children, 34 (67%) had a history of allergic rhinitis during August and September, 9 (18%) had previously presented with eczema, and 6 children had no history of atopic diseases.
All 51 pediatric patients presented with wheezing. According to the definitions of the severity of acute asthma exacerbations of the GINA guidelines, 39 (76%) children were classified as having moderate asthma, 8 (16%) as mild asthma, and 4 (8%) as severe asthma. Nine children had onset of cough after the thunderstorms, and 38 (74%) children had symptoms of rhinitis. Clinical manifestations and the results of pulmonary function tests are shown in Table 1.
Of the total hospitalized children, 32 underwent serum-specific IgE testing against common airborne allergens including tree and weed pollens, mold, and dust mites. Thirty (94%) children were IgE-positive against mugwort pollen, including 25 (78%) who were monosensitized to this pollen and 5 were also IgE-positive against dust mites. The allergen profile is illustrated in Fig. 3.
Discussion
In this study, we described a thunderstorm asthma epidemic among pediatric patients in Yulin City, China and retrospectively analyzed the features of this cohort, which are reported for the first time.
Asthma symptoms have been thought to only be aggravated in adults during thunderstorms and not in children.8,14 It has been reported that thunderstorm asthma affects less than 15% of children.4,5,6,14 Our data demonstrated that thunderstorm asthma is not rare in pediatric patients. Without the profile of adults during our study period, it was difficult to estimate the age proportion of the affected individuals. However, according to the literature, more than 50% of emergency patients with thunderstorm asthma are children.15
Male sex predominated among patients in both the emergency/outpatient department (74%, n = 290/391) and inpatient department (72%, n = 73/101). This preponderance with respect to gender is also found among adults owing to a greater number of men in the workforce.16 However, it is difficult to explain the sex distribution among children in the same manner.
About half of patients attended the emergency/outpatient department within 24 h after the thunderstorm event, with a peak 18–24 h following the event. The exact time course between thunderstorm exposure and asthma attacks is difficult to calculate because the children were unable to recall the precise time when they began to feel uncomfortable. However, based on the time frame of presentation to medical services, it can be estimated that the most severe asthma symptoms among half of patients occurred approximately 18–24 h following the thunderstorm.
In our study, 76% of children were classified as have asthma of moderate severity, which emphasizes the seriousness and heavy burden of epidemic thunderstorm asthma. Only two children had current asthma before the thunderstorm event. Moreover, 21% had a confirmed diagnosis of asthma but had been symptom-free for 6 months. In these patients, appropriate prophylactic medication may be effective in preventing severe attacks of thunderstorm asthma. It has been found that among patients taking preventive medications, the emergency demand for these medicines during thunderstorms was much lower than among patients who used bronchodilators alone (21% vs. 103%).17 A total 18% of patients had symptoms suggestive of asthma but were undiagnosed. Early identification of such patients and the provision of appropriate preventive medication may reduce the burden of asthma attacks during thunderstorms. Similar to previous studies, more than half of the hospitalized children in our study had never been diagnosed or had presented with asthma previously.10,11 Most patients who were asthma-naive had a history of allergic rhinitis in summer and autumn (August−September). Additionally, the prevalence of a history of summer/autumn allergic rhinitis among all hospitalized children was 66%. In line with the literature, allergic rhinitis appears to be a risk factor of thunderstorm asthma attacks. According to the hypo-theory of “one airway, one disease”, treating allergic rhinitis would benefit comorbid allergic asthma, which has been proven in several retrospective studies. Therefore, we infer that standard therapy for pollen allergic rhinitis may also be effective in preventing thunderstorm asthma. Further well-designed, cohort-controlled studies are needed to confirm such conclusions.
In our cohort from the inpatient department, 94% were allergic to mugwort, which was first described in thunderstorm asthma. Mugwort is the most important allergen in northern China during late summer and autumn. It has been estimated that 58% of patients with pollinosis are sensitized to mugwort in the north of the country.18 The role of mugwort is similar to that of grass pollen and fungal spores in the pathogenesis of thunderstorm asthma, which has been demonstrated in many studies.
In summary, we described a thunderstorm asthma epidemic among pediatric patients in northern China. Male children were more frequently affected by thunderstorm asthma. We implicated weed pollen as another common aeroallergen in thunderstorm asthma attacks. Allergic rhinitis and asthma without preventive treatment were identified as risk factors of thunderstorm asthma. Hence, early identification of high-risk patients, standard treatment of current allergic rhinitis, proper diagnosis of potential asthma, and prescription of preventive medication would be beneficial in preventing thunderstorm asthma attacks.
References
Packe, G. E. & Ayres, J. G. Asthma outbreak during a thunderstorm. Lancet 2, 199–204 (1985).
Davidson, A. C. et al. A major outbreak of asthma associated with a thunderstorm: experience of accident and emergency departments and patients’ characteristics. Thames Regions Accident and Emergency Trainees Association. BMJ 312, 601–604 (1996).
Venables, K. M. et al. Thunderstorm-related asthma—the epidemic of 24/25 June 1994. Clin. Exp. Allergy 27, 725–736 (1997).
Pulimood, T. B. et al. Epidemic asthma and the role of the fungal mold Alternaria alternata. J. Allergy Clin. Immunol. 120, 610–617 (2007).
Girgis, S. T. et al. Thunderstorm-associated asthma in an inland town in south-eastern Australia. Who is at risk? Eur. Respir. J. 16, 3–8 (2000).
Bellomo, R. et al. Two consecutive thunderstorm associated epidemics of asthma in the city of Melbourne. The possible role of rye grass pollen. Med. J. Aust. 156, 834–837 (1992).
Woodhead, M. Hospitals overwhelmed with patients after “thunderstorm asthma” hits Melbourne. BMJ 355, i6391 (2016).
Wardman, A. E. D. et al. Thunderstorm-associated asthma or shortness of breath epidemic: a Canadian case report. Can. Respir. J. 9, 267–270 (2002).
D’Amato, G. et al. Thunderstorm-related asthma: not only grass pollen and spores. J. Allergy Clin. Immunol. 121, 537–538 (2008).
Forouzan, A. et al. An overview of thunderstorm-associated asthma outbreak in southwest of Iran. J. Environ. Public Health 2014, 504017 (2014).
Thien, F. et al. The Melbourne epidemic thunderstorm asthma event 2016: an investigation of environmental triggers, effect on health services, and patient risk factors. Lancet Planet Health 2, e255–e263 (2018).
Newson, R. et al. Effect of thunderstorms and airborne grass pollen on the incidence of acute asthma in England, 1990−94. Thorax 52, 680–685 (1997).
Taylor, P. E. & Jonsson, H. Thunderstorm asthma. Curr. Allergy Asthma Rep. 4, 409–413 (2004).
Egan, P. Weather or not. Med. J. Aust. 142, 330 (1985).
Jariwala, S. et al. The association between asthma-related emergency department visits and pollen and mold spore concentrations in the Bronx, 2001-2008. J. Asthma 51, 79–83 (2014).
Taylor, P. E. et al. Release of allergens as respirable aerosols: a link between grass pollen and asthma. J. Allergy Clin. Immunol. 109, 51–56 (2002).
Andrew, E. et al. Stormy weather: a retrospective analysis of demand for emergency medical services during epidemic thunderstorm asthma. BMJ 359, j5636 (2017).
Hao, G.-D. et al. Prevalence of sensitization to weed pollens of Humulus scandens, Artemisia vulgaris, and Ambrosia artemisiifolia in northern China. J. Zhejiang Univ. Sci. B 14, 240–246 (2013).
Author information
Authors and Affiliations
Contributions
Y.-Y.X. made substantial contributions to conception and design, analysis and interpretation of data, and drafting the article. T.X. and H.-R.L. made substantial contributions to the acquisition of data. K.G. made substantial contributions to conception and design, and gave the final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xu, YY., Xue, T., Li, HR. et al. Retrospective analysis of epidemic thunderstorm asthma in children in Yulin, northwest China. Pediatr Res 89, 958–961 (2021). https://doi.org/10.1038/s41390-020-0980-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0980-9
This article is cited by
-
Comments on “Impact of meteorological parameters and air pollutants on airborne concentration of Betula pollen and Bet v 1 allergen” by Vašková1, Zuzana et al., https://doi.org/10.1007/s11356-023–29061-z
Environmental Science and Pollution Research (2024)