Abstract
Aim
The rising number of children carrying chronic disease with them into adulthood presents the research community with an obligation to address their unique needs. Authentic involvement of individuals and communities directly affected by the condition being studied ensures that research answers the questions of those most affected. Our aim was to identify the highest priority research questions of young people living with chronic illness and their caregivers.
Materials and Methods
We conducted a qualitative study using the Research Prioritization by Affected Communities (RPAC) method. Participants were recruited from two hospitals and two community organizations to participate in focus groups.
Results
Twenty three participants developed and prioritized 300 potentially researchable questions. Thematic analysis of the priority research topics revealed three health dimensions of chronic illness (physical health, social-emotional health and navigating the health care system) and two cross-cutting dimensions (living with a chronic illness and future with a chronic illness).
Conclusion
Young people experiencing different chronic conditions were able to achieve consensus on the same set of condition-agnostic research priorities, age and role influenced research priorities. We report these research priorities to inform and influence local and national research agendas and funding priorities.
Impact
-
Patients and caregivers affected by different chronic illnesses were able to achieve consensus on condition-agnostic research priorities. Age and role influenced research priorities.
-
Questions posed by young people experiencing different chronic conditions fell under three themes (physical, social–emotional and health care system) and two cross-cutting dimensions (living with a chronic illness and future with a chronic illness).
-
Use of the Research Prioritization by Affected Communities (RPAC) method, which begins with the patient’s lived experiences, provided nuanced insights into the complexity of living with a chronic illness and surfaced under-studied research topics to guide future research investment.
Similar content being viewed by others
Introduction
There has been a growing international movement in recent years for greater patient and public involvement (PPI) in all aspects of the research process, including determining the focus, design, implementation, analysis, and dissemination of findings. Authentic involvement of individuals and communities directly affected by the condition being studied ensures that research answers the questions of those most affected by the condition.1 Although patients, families, and communities are frequently engaged in pediatric service delivery planning, there remains a need for greater PPI in the field of pediatric research.2 Because PPI remains relatively new within pediatric research, there is little understanding regarding topics of interest for patients and their families. The research interests of pediatric patients living with chronic conditions, which will last throughout adulthood, remain an important knowledge gap. In this report, we present research priorities of young people living with chronic conditions and their caregivers for the purpose of informing and influencing local and national research agendas and funding priorities.
Methods
Study design
We conducted focus groups according to the Research Prioritization by Affected Communities (RPAC) method3 to investigate young people’s and caregivers’ unanswered questions about chronic conditions in the context of their own experiences. As specified by the RPAC method, research questions and topics were generated directly from individuals most affected by the condition, rather than beginning with a review of the medical literature, which prioritizes the questions of academics and clinicians. The RPAC method has been used effectively to illuminate the priorities of women and men from communities at high risk for preterm birth and parents of preterm infants.3,4 We also followed the long-form checklist from the Guidance for Reporting Involvement of Patients and the Public (GRIPP2), developed by international consensus to ensure quality, transparency, and consistency of reporting PPI in research.5
Participant recruitment
Participants were recruited by flier and website advertisements from two local children’s hospitals, Benioff Children’s Hospital San Francisco (BCH-SF) and Oakland (BCH-O), which serve different populations, and from two local community organizations, San Francisco Support for Families of Children with Disabilities (SFCD), and California Children’s Services, which provide a range of support services for families of children with chronic illness. Three cohorts of participants were recruited: adolescent patients age 15–18 years, young adult patients age 19–25 years, and caregivers (parents or guardians). The inclusion criteria for patients were: English literate and living with a chronic illness for >1 year, which was anticipated to last into adulthood.6 Caregivers were included if they were English literate and caring for a child or young adult patient with a chronic condition. Only one participant per family and no more than two patients with the same condition were included in any focus group. The project was approved by the University of California, San Francisco Institutional Review Board (#17-23588). Each participant received a $25 Target gift card. Compensation for child care and travel, and refreshments were offered for each focus group session.
Procedures
Focus groups were held at BCH-O and SFCD. Following the RPAC method,3 facilitators used scripts tailored to each group and setting. During the first focus group session participants shared their experiences of living (or caring for someone) with a chronic condition and generated an extensive list of questions. The research team then categorized these questions by topic. During the second focus group, participants prioritized the topics they wanted researchers to focus on and ranked the specific questions they were most eager to have answered.
Analysis
The ranking of the priority topics was compared across the five groups to identify patterns by role and location. Using qualitative thematic analysis, research questions were grouped into themes and subthemes.7 The first and last authors listened to the recordings, reviewed the transcripts for accuracy and conducted first-level coding to develop themes and subthemes. The full author group, including two focus group participants, reviewed, discussed, and refined themes, identifying relevant quotes to serve as exemplars. Any disagreements were resolved by further discussion and consensus.
Results
Five cohorts participated in focus group sessions: two caregiver groups, two adolescent patient groups (one each at BCH-O and SFCD) and one young adult patient group at SFCD. A total of 12 caregivers, 5 young adult patients, and 6 adolescents participated. Participants varied in age, race/ethnicity, insurance status, and chronic condition (Table 1). All participants attended two sessions, ~6 weeks apart between February and May, 2018.
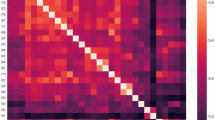
Across the five groups, a total of 300 potentially researchable questions were developed, representing 21 distinct research topics (see Fig. 1 for the top 3 research questions by group, and Supplementary Table S1 for the complete list). Although the top-ranked topic varied by group, the following five topics were priorities across all groups: Health Care System and Care Coordination/Communication; Insurance/Health Care Coverage; Patient–Parent–Provider Relationship and Communication; Social/Emotional/Family Impact and Support; and Transition to Independence: Going from Pediatric to Adult Care (Fig. 2).
All groups highly ranked the following five topics (highlighted in color): Health Care System and Care Coordination/Communication, Insurance/Health Care Coverage, Patient–Parent–Provider Relationship/Communication, Social/Emotional/Family Impact and Support; and Transition to Independence. SFCD San Francisco Support for Families of Children with Disabilities, BCH-O Benioff Children’s Hospital-Oakland.
Differences in prioritization of topics were noted across groups. For example, medication research was included in the top-ranked topics for all three patient groups, but not the caregiver groups. Stress and coping research only appeared as a priority topic for the young adult patient group. They also expressed concern about burdening their parents. In contrast, the caregiver groups posed questions focused on support for caregivers, health care systems, communication, and support for their child in the future should the caregiver become incapacitated or deceased. The caregivers described a notion of “the parent as the expert” and the burden of the caregiver’s duties as “a second job”. The young adult patients’ research questions focused on the future in relation to the long-term effects of both their medications and their chronic condition, as well as the importance of research related to finding a “new normal” and promoting hope. The adolescent patient’s questions focused on the impact of chronic illness on school and family life and finding ways to better understand and manage their symptoms. They also described facing a daily ethical dilemma around accepting school accommodations.
Thematic analysis of the highest ranking potentially researchable questions across all groups revealed three health dimensions of chronic illness research: questions about physical health, social–emotional health, and navigating the health care system. In addition, the research team recognized two cross-cutting dimensions that reflected the interconnectedness of domains and the dimension of time (living with a chronic illness and future with a chronic illness).
Discussion
Using the RPAC method, pediatric chronic illness patients and their caregivers generated numerous researchable questions and topics that may be used to guide future research and study planning. The RPAC method was selected because our aim was to elicit research questions and achieve consensus on priority research topics directly from the individuals who experience the health condition of interest.3 Inclusion of patients in research follows a continuum from engagement, to participation, to involvement.8 Involvement, the highest level of contact between researchers and the public, occurs when patients or members of the affected community are actively involved in all aspects of the research process, including the development of research priorities.9 RPAC was developed to enhance the involvement of patients in identifying research priorities by engaging directly with participants about their personal experiences, rather than beginning with survey data or researcher developed topics. Similar to prior studies, our findings include pediatric chronic illness research interests across a wide range of topics.10 Our work adds to the literature by identifying research priorities that are condition agnostic. Moreover, many of the priorities focus on health service delivery and finance, similar to the priorities generated by a multi-stakeholder group for children and youth with special healthcare needs.11
Holding separate focus groups for participants of different ages and roles allowed us to identify the unique priorities for each group. Adolescents were most concerned with symptom management and school, young adults focused primarily on future health and employment, and caregivers prioritized both current and long-term challenges navigating the health care system. Anchoring the focus group discussion in participants’ personal experiences allowed us to achieve greater insight into the complexity of living with a chronic illness. Several important worries emerged, such as young people’s concerns about burdening their parents and the feeling among caregivers that caring for the chronically ill child was akin to a second job. While all groups shared common themes, we gained insight into how age and role may contribute to the types of questions that are most relevant to individuals impacted by chronic illness. Our findings have informed a collaborative process with patients and researchers working side by side to develop a research protocol that answer’s a high priority question in our community.
We note several limitations of this study. Although the study sample was small, and included only English speakers, the impressive number of questions that were generated demonstrates the power of the RPAC method. In addition, the thematic analysis was performed by consensus and thus subject to bias from more influential members of the group; however, the inclusion of two focus group participants in the analysis enhanced the trustworthiness of the process.
Our primary aim was to identify research priorities for patients and caregivers and to make them available publicly so that research funders, researchers, and communities can pursue or advocate for research on these priorities (https://childhoodchronicillness.ucsf.edu/patientfamilypriorities). Our findings have other applications more broadly in the health care arena. Our hope is that the power and importance of involving patients and caregivers in research and the development of interventions is more widely recognized. We also encourage healthcare and social service providers to use these findings to direct the development of educational and clinical interventions that address the patient’s greatest areas of concern. Finally, PPI is a compelling method to inform and engage individuals in their own healthcare, which beyond its value to research has the potential to positively impact health literacy, patient empowerment, trust, and service quality.12,13
Molloy et al.2 challenge the pediatric research community to embrace PPI in child health research. Our work builds upon this recommendation, and we encourage researchers and donors to include patients and caregivers in decisions about research priorities and funding. Partnership at all levels and stages of research ensures that resources are directed to activities that are impactful and desirable for communities directly affected by pediatric chronic illness. Lifting up the voices of patients and caregivers is a crucial part of identifying the research questions that will shape the future of chronic illness care.
References
Forsythe, L. P. et al. Patient engagement in research: early findings from the patient-centered outcomes research institute. Health Aff. 38, 359–367 (2019).
Molloy, E. J., Mader, S., Modi, N. & Gale, C. Parent, child and public involvement in child health research: core value not just an optional extra. Pediatr. Res. 85, 2–3 (2019).
Franck, L. S. et al. A novel method for involving women of color at high risk for preterm birth in research priority setting. J. Vis. Exp. 131, 1–9 (2018).
Edwards, B. N. et al. What about the men? Perinatal experiences of men of color whose partners were at risk for preterm birth, a qualitative study. BMC Pregnancy Childbirth 20, 1–11 (2020).
Staniszewska, S. et al. GRIPP2 reporting checklists: Tools to improve reporting of patient and public involvement in research. BMJ 358, 1–7 (2017).
Stein, R. E., Bauman, L. J., Westbrook, L. E., Coupey, S. M. & Ireys, H. T. Framework for identifying children who have chronic conditions: the case for a new definition. J. Pediatr. 122, 342–347 (1993).
Braun, V. & Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101 (2006).
Belone, L. et al. Community-based participatory research conceptual model: community partner consultation and face validity. Qual. Health Res. 26, 117–135 (2016).
Cowan, K., & Oliver, S. The James Lind Alliance Guidebook: Version 5. http://www.jlaguidebook.org/pdfguidebook/guidebook.pdf (2013).
Odgers, H. L. et al. Research priority setting in childhood chronic disease: a systematic review. Arch. Dis. Child. 103, 942–951 (2018).
Coller, R. J. et al. Health system research priorities for children and youth with special health care needs. Pediatrics 145, 1–12 (2020).
Frank, L. et al. Conceptual and practical foundations of patient engagement in research at the patient-centered outcomes research institute. Qual. Life Res. 24, 1033–1041 (2015).
Domecq, J. P. et al. Patient engagement in research: a systematic review. BMC Health Serv. Res. 14, 1–9 (2014).
Acknowledgements
Research reported in this publication was funded through a Patient-Centered Outcomes Research Institute® (PCORI®) Award (5134413).
Author information
Authors and Affiliations
Contributions
E.v.S. contributed as follows: substantial contributions to conception and design, acquisition of data, analysis and interpretation of data, drafting the article and revising it critically for important intellectual content, and final approval of the version to be published. B.K.N. contributed as follows: substantial contribution to acquisition of data, analysis, and final approval of the version to be published. I.C.C. contributed as follows: substantial contribution to analysis and interpretation of the data, and final approval of the version to be published. R.K. contributed as follows: substantial contribution to analysis and interpretation of the data, and final approval of the version to be published. L.S.F. contributed as follows: substantial contribution to conception and design, acquisition of data, analysis and interpretation of data, drafting the article and revising it critically for important intellectual content, and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
All participants provided informed consent as per the UCSF Institutional Review Board approved protocol (17-23588).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
von Scheven, E., Nahal, B.K., Cohen, I.C. et al. Research Questions that Matter to Us: priorities of young people with chronic illnesses and their caregivers. Pediatr Res 89, 1659–1663 (2021). https://doi.org/10.1038/s41390-020-01207-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01207-6
This article is cited by
-
How do we best engage young people in decision-making about their health? A scoping review of deliberative priority setting methods
International Journal for Equity in Health (2023)